Acid reflux with tirzepatide is a recognised gastrointestinal side effect of this dual GIP and GLP-1 receptor agonist, licensed in the UK for type 2 diabetes and weight management. Marketed as Mounjaro, tirzepatide slows gastric emptying to promote satiety, which can increase the likelihood of gastro-oesophageal reflux, particularly during initial treatment phases. Whilst reflux symptoms may be troublesome for some patients, they can often be effectively managed through lifestyle modifications and, when necessary, pharmacological interventions such as alginates or proton pump inhibitors. Understanding the mechanisms behind this side effect and implementing appropriate management strategies enables patients to continue benefiting from tirzepatide therapy whilst maintaining quality of life.
Quick Answer: Acid reflux with tirzepatide occurs because the medication slows gastric emptying, increasing the time food remains in the stomach and the likelihood of reflux into the oesophagus.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereTirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus and, more recently, for weight management in adults with obesity or overweight with weight-related comorbidities. Marketed under the brand name Mounjaro, this injectable medication has demonstrated significant efficacy in glycaemic control and weight reduction. For weight management, tirzepatide is prescribed according to NICE criteria and is typically initiated by specialist services.
Acid reflux, also known as gastro-oesophageal reflux or heartburn, is recognised as a gastrointestinal adverse reaction associated with tirzepatide. According to the Mounjaro Summary of Product Characteristics (SmPC), gastrointestinal disorders are very common side effects, with dyspepsia and gastro-oesophageal reflux disease specifically listed among the adverse reactions. The primary gastrointestinal side effects observed during pivotal studies include nausea, vomiting, diarrhoea, and constipation, which affect a substantial proportion of users, particularly during dose escalation. Acid reflux symptoms may manifest as a burning sensation in the chest, regurgitation of stomach contents, or an unpleasant sour taste in the mouth.
Understanding the potential mechanisms and management strategies is essential for both patients and healthcare professionals to optimise treatment outcomes and maintain quality of life during tirzepatide therapy. If you experience side effects while taking tirzepatide, you can report them via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
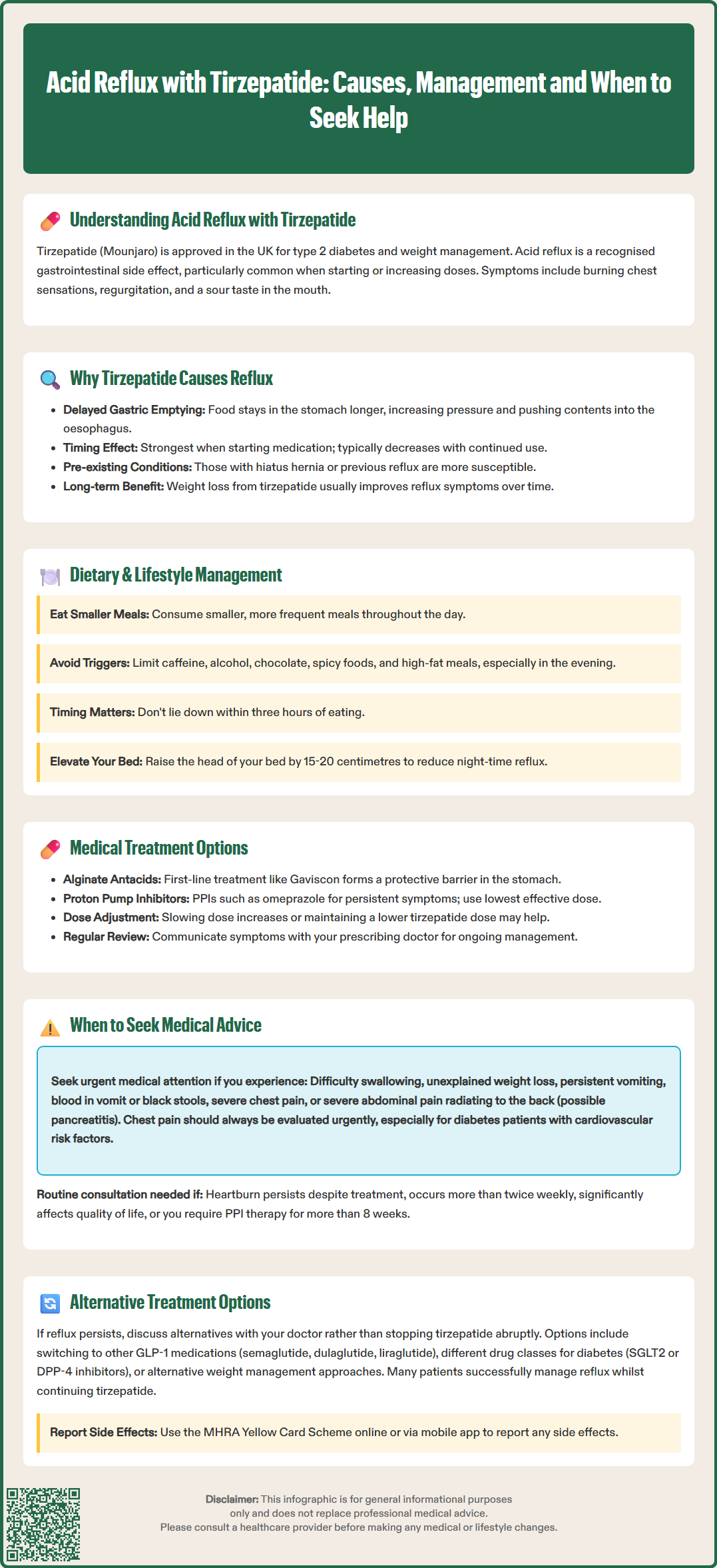
The mechanism by which tirzepatide contributes to acid reflux relates primarily to its effects on gastric motility and emptying. As a GLP-1 receptor agonist component, tirzepatide significantly slows gastric emptying, which is one of the key mechanisms through which it promotes satiety and aids weight loss. This delayed emptying means food and gastric contents remain in the stomach for longer periods, potentially increasing intragastric pressure and the likelihood of reflux into the oesophagus, particularly when the lower oesophageal sphincter is compromised. It's worth noting that this gastric emptying delay is typically most pronounced after initial doses and tends to attenuate with continued use.
While some patients may experience temporary changes in reflux symptoms during the initial phases of treatment and weight loss, sustained weight loss typically improves reflux symptoms in the longer term. This improvement occurs because obesity itself is a significant risk factor for gastro-oesophageal reflux disease (GORD), and reducing excess weight often leads to better reflux control.
The nausea and delayed gastric emptying associated with tirzepatide may also lead patients to alter their eating patterns—consuming smaller, more frequent meals or eating closer to bedtime—which can inadvertently increase reflux risk. Furthermore, individual susceptibility varies considerably; patients with pre-existing hiatus hernia, previous GORD, or other anatomical predispositions may be more vulnerable to experiencing reflux symptoms when gastric emptying is pharmacologically delayed. The dual agonist action on both GIP and GLP-1 receptors may produce different gastrointestinal effects compared to single GLP-1 agonists, though comparative data specifically regarding reflux incidence remain limited.
Effective management of acid reflux whilst continuing tirzepatide therapy typically involves a combination of lifestyle modifications and, when necessary, pharmacological interventions. Patients should be advised to implement dietary changes that reduce reflux triggers, including avoiding large meals, particularly in the evening, and limiting intake of known precipitants such as caffeine, alcohol, chocolate, spicy foods, and high-fat meals. Eating smaller, more frequent meals can help accommodate the delayed gastric emptying without overwhelming the stomach's capacity.
Postural and timing strategies are equally important. Patients should avoid lying down within three hours of eating and may benefit from elevating the head of the bed by 15–20 centimetres using blocks or a wedge pillow, which uses gravity to reduce nocturnal reflux. Maintaining a healthy posture during and after meals, avoiding tight clothing around the abdomen, and refraining from bending or stooping immediately after eating can all help minimise symptoms.
When lifestyle measures prove insufficient, pharmacological management may be appropriate. Alginate-based antacids (such as Gaviscon) are often effective first-line options, forming a protective raft on top of stomach contents to prevent reflux. Other antacids containing aluminium hydroxide or magnesium carbonate can provide rapid, short-term symptom relief for occasional heartburn. For more persistent symptoms, proton pump inhibitors (PPIs) such as omeprazole or lansoprazole are highly effective at reducing gastric acid production. Low-dose PPIs (omeprazole 10 mg, esomeprazole 20 mg) are available over the counter for short-term use, but patients should consult their pharmacist or GP before prolonged use. According to NICE guidance (CG184), PPIs should be used at the lowest effective dose with periodic review and step-down attempts for long-term therapy. H2-receptor antagonists like famotidine represent alternative acid-suppressing options.
Patients should also review and minimise use of non-steroidal anti-inflammatory drugs (NSAIDs) where possible, as these can worsen dyspepsia and reflux. Maintaining open communication with the prescribing clinician about reflux symptoms is important, as dose adjustment or temporary treatment interruption may occasionally be warranted. However, many patients find that reflux symptoms improve as they adapt to the medication over several weeks.
Whilst mild, occasional acid reflux can often be managed with lifestyle modifications and over-the-counter remedies, certain symptoms warrant prompt medical evaluation. Patients should contact their GP or prescribing clinician if they experience persistent heartburn that does not respond to initial management strategies, particularly if symptoms occur more than twice weekly or significantly impact quality of life and daily activities.
Red flag symptoms requiring urgent medical attention include difficulty swallowing (dysphagia) at any age, unintentional weight loss beyond that expected from tirzepatide therapy (especially in combination with upper abdominal pain, reflux or dyspepsia in those aged 55 and over), persistent vomiting, evidence of gastrointestinal bleeding (such as vomiting blood or passing black, tarry stools), or severe, unremitting chest pain. These symptoms may indicate complications such as oesophagitis, stricture formation, or, rarely, more serious pathology that requires investigation. Chest pain, in particular, should always be evaluated urgently to exclude cardiac causes, especially in patients with diabetes who may have cardiovascular risk factors.
In accordance with NICE guidance (NG12) on suspected cancer referral pathways, patients with dysphagia or those with alarm features should be referred for urgent endoscopic investigation to exclude upper gastrointestinal malignancy. Additionally, if reflux symptoms are accompanied by severe, persistent abdominal pain radiating to the back (with or without vomiting), this may indicate pancreatitis—a rare but serious adverse effect associated with GLP-1 receptor agonists as noted in the tirzepatide SmPC—and requires immediate medical assessment.
For patients requiring long-term PPI therapy (beyond 8 weeks) to control reflux symptoms whilst on tirzepatide, review by a gastroenterologist may be appropriate to investigate underlying causes and consider endoscopic evaluation, as recommended in NICE CG184. Regular medication review ensures that the benefits of continuing tirzepatide outweigh any adverse effects and that reflux is being optimally managed.
When acid reflux symptoms prove troublesome despite optimal management strategies, several options exist for adjusting tirzepatide therapy or considering alternatives. Dose modification represents the first consideration; slowing the rate of dose escalation or temporarily maintaining a lower dose may allow the gastrointestinal system to adapt whilst still providing therapeutic benefit. The standard titration schedule for tirzepatide involves gradual increases every four weeks, but this can be individualised based on tolerability. Some patients may achieve adequate glycaemic control and weight loss at lower maintenance doses that produce fewer gastrointestinal side effects.
If reflux symptoms remain intolerable despite these measures, alternative GLP-1 receptor agonists may be considered. Different agents within this class have varying effects on gastric emptying and gastrointestinal tolerability. Semaglutide, dulaglutide, and liraglutide are established alternatives, though they too can cause gastrointestinal side effects. The choice depends on individual patient factors, treatment goals, and previous medication history. For patients primarily using tirzepatide for type 2 diabetes management, other drug classes such as SGLT2 inhibitors or DPP-4 inhibitors may be appropriate alternatives in line with NICE guidance (NG28), though they lack the same degree of weight loss benefit.
For patients using tirzepatide specifically for weight management, alternative approaches include other anti-obesity medications such as semaglutide (Wegovy), which is also subject to NICE approval criteria (TA875) and specialist initiation, or orlistat. Naltrexone-bupropion combination therapy has limited NHS availability and is not routinely commissioned in many areas. Non-pharmacological interventions, including structured lifestyle programmes, dietetic support, and psychological interventions, remain fundamental components of weight management and may be intensified if medication is not tolerated.
Decisions regarding treatment modification should always be made in consultation with the prescribing clinician, considering the overall benefit-risk profile, treatment objectives, and individual patient circumstances. Abrupt discontinuation of tirzepatide is not typically necessary for reflux symptoms alone, and many patients successfully continue therapy with appropriate supportive management. Regular follow-up allows for ongoing assessment of both therapeutic efficacy and tolerability, ensuring optimal outcomes.
Gastrointestinal disorders, including gastro-oesophageal reflux and dyspepsia, are listed as very common side effects in the Mounjaro Summary of Product Characteristics. Reflux symptoms are particularly likely during dose escalation and often improve as patients adapt to the medication.
Yes, alginate-based antacids such as Gaviscon and proton pump inhibitors like omeprazole can be used alongside tirzepatide to manage reflux symptoms. Consult your GP or pharmacist before starting long-term acid suppression therapy.
Abrupt discontinuation is not typically necessary for reflux symptoms alone. Most patients successfully continue tirzepatide with lifestyle modifications and appropriate medical management, though you should discuss persistent symptoms with your prescribing clinician.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.