Ozempic (semaglutide) is a widely prescribed GLP-1 receptor agonist for type 2 diabetes management in the UK, known primarily for its gastrointestinal side effects such as nausea and diarrhoea. Whilst hiccups are not listed as an official adverse reaction in MHRA-approved prescribing information, some patients have reported experiencing them during treatment. Understanding whether hiccups represent a genuine side effect of Ozempic requires examining the medication's mechanism of action, clinical evidence, and the theoretical links between delayed gastric emptying and diaphragmatic irritation. This article explores the relationship between Ozempic and hiccups, when to seek medical advice, and practical management strategies.
Quick Answer: Hiccups are not listed as an official side effect of Ozempic in UK prescribing information, though anecdotal patient reports exist and theoretical mechanisms through delayed gastric emptying may explain occasional occurrences.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Administered as a once-weekly subcutaneous injection, it works by mimicking the action of the naturally occurring hormone GLP-1, which stimulates insulin secretion in a glucose-dependent manner, suppresses glucagon release, and slows gastric emptying. These mechanisms help improve glycaemic control in people with type 2 diabetes.
The most frequently reported side effects of Ozempic are gastrointestinal in nature, affecting a significant proportion of patients, particularly during the initial weeks of treatment or following dose escalation. According to the Summary of Product Characteristics (SmPC) approved by the Medicines and Healthcare products Regulatory Agency (MHRA), common adverse effects include:
Nausea (very common, affecting more than 1 in 10 patients)
Diarrhoea (very common)
Vomiting (common, affecting up to 1 in 10 patients)
Constipation (common)
Abdominal pain (common)
Dyspepsia (common)
Decreased appetite (very common)
Abdominal distension (common)
Flatulence and eructation (common)
Injection-site reactions (common)
These gastrointestinal symptoms typically diminish over time as the body adjusts to the medication. Less common but more serious adverse effects include pancreatitis, gallbladder disease, and hypoglycaemia (particularly when used in combination with insulin or sulphonylureas). Patients should also be aware of the risk of diabetic retinopathy complications and the potential for dehydration leading to acute kidney injury with severe gastrointestinal effects.
Patients should be counselled about these potential side effects before initiating treatment, and healthcare professionals should monitor for tolerability throughout the treatment course. Understanding the expected side effect profile helps patients distinguish between typical reactions and symptoms that may warrant further medical evaluation.
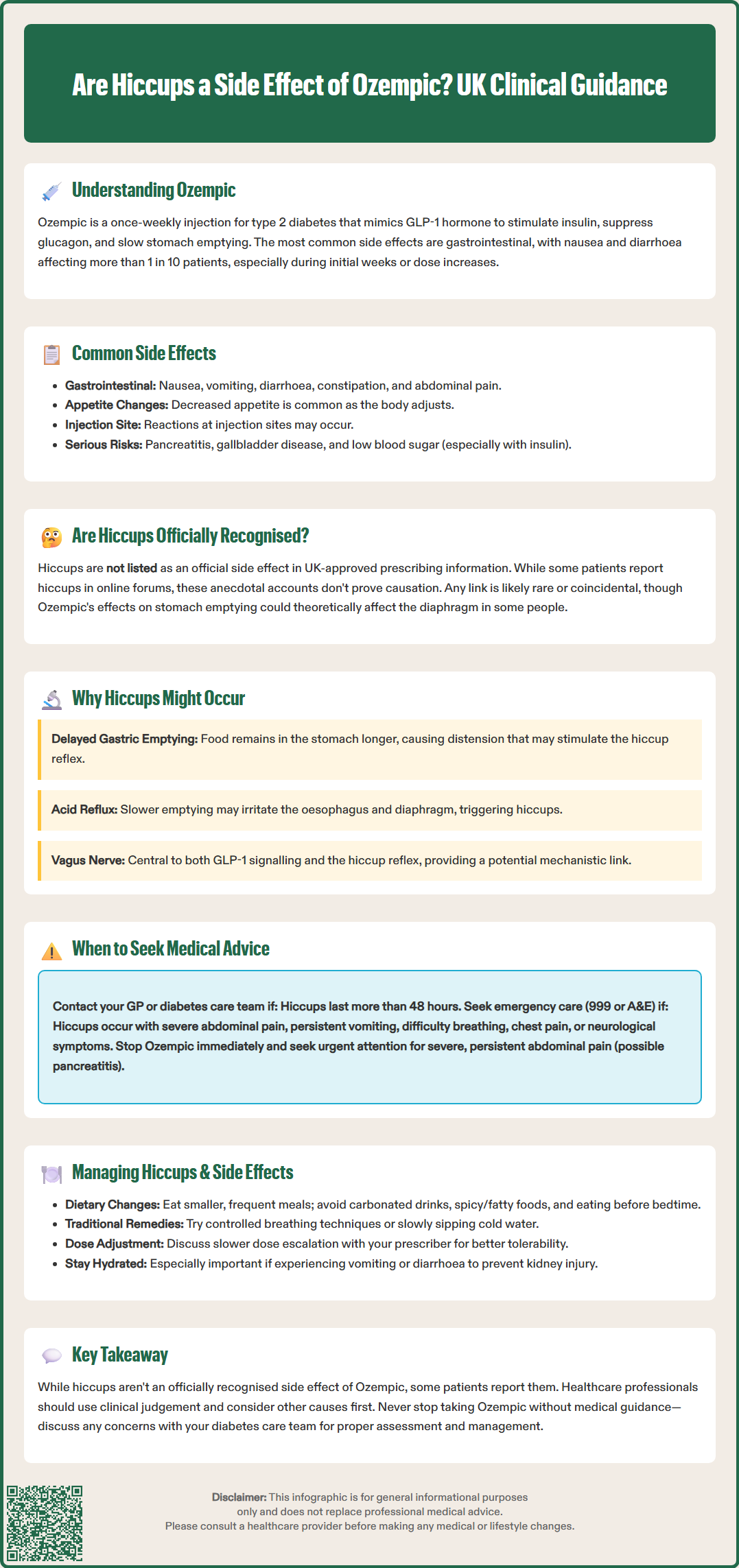
Hiccups are not listed as an official side effect in the UK-approved prescribing information for Ozempic. The MHRA-approved SmPC does not include hiccups (singultus) amongst the documented adverse reactions reported during clinical trials or post-marketing surveillance. This means that hiccups have not been identified as occurring with sufficient frequency or clear causality to warrant inclusion in the formal safety profile of semaglutide.
However, anecdotal reports from patients taking Ozempic have occasionally mentioned experiencing hiccups, particularly in online patient forums and social media discussions. It is important to recognise that such reports do not establish a definitive causal relationship. Hiccups are a common phenomenon in the general population and can occur for numerous reasons unrelated to medication use, including eating too quickly, consuming carbonated beverages, sudden temperature changes, or emotional stress.
The absence of hiccups from official documentation suggests that if there is any association with Ozempic, it is likely to be rare, indirect, or coincidental. Given that Ozempic significantly affects gastrointestinal motility and gastric emptying—both of which can influence diaphragmatic function and oesophageal pressure—there is a theoretical mechanism by which the medication might contribute to hiccups in susceptible individuals. Nevertheless, without robust clinical evidence, healthcare professionals should approach patient reports of hiccups with appropriate clinical judgement, considering alternative causes whilst acknowledging the patient's experience.
Patients experiencing persistent or troublesome hiccups whilst taking Ozempic should discuss this with their GP or diabetes specialist nurse, who can assess whether the symptom warrants investigation or management, and whether it might be related to the medication or another underlying cause.
To understand why hiccups might theoretically occur with Ozempic, it is helpful to examine the medication's mechanism of action on the gastrointestinal system. As a GLP-1 receptor agonist, semaglutide significantly slows gastric emptying, meaning food remains in the stomach for longer periods. This delayed emptying is one of the key mechanisms contributing to the medication's effects on glycaemic control and appetite, but it also underlies many of the gastrointestinal side effects patients experience.
Delayed gastric emptying could hypothetically lead to several consequences that might indirectly trigger hiccups:
Gastric distension: When the stomach empties more slowly, it may become distended, particularly after meals. This distension could potentially stimulate the phrenic nerve or vagus nerve, both of which play roles in the hiccup reflex arc.
Possible contribution to reflux symptoms: Slower gastric emptying may contribute to reflux symptoms in some people, which could irritate the oesophagus and diaphragm, potentially triggering hiccups.
Altered intra-abdominal pressure: Changes in gastric volume and pressure may affect diaphragmatic function, as the diaphragm sits directly above the stomach.
Additionally, nausea and bloating—both very common with Ozempic—may cause patients to swallow air more frequently (aerophagia) or alter their breathing patterns, which can precipitate hiccups. The vagus nerve, which is extensively involved in GLP-1 receptor signalling, also plays a central role in the hiccup reflex, providing another potential mechanistic link.
Whilst these theoretical mechanisms are plausible, it is important to emphasise that there is no official clinical evidence establishing hiccups as a direct consequence of Ozempic therapy. The gastrointestinal effects of the medication are well-documented in the SmPC and European Public Assessment Report (EPAR), but hiccups specifically have not been validated through controlled clinical studies.
Most episodes of hiccups are benign and self-limiting, resolving spontaneously within minutes to hours. However, persistent or intractable hiccups—defined as lasting more than 48 hours—can indicate an underlying medical problem and warrant clinical evaluation. Patients taking Ozempic who experience hiccups should consider seeking medical advice in the following circumstances:
Call 999 or go to A&E if hiccups are accompanied by:
Severe abdominal pain (which could indicate pancreatitis or gallbladder disease)
Persistent vomiting or inability to keep fluids down
Signs of dehydration (reduced urination, dizziness, dry mouth)
Difficulty breathing or chest pain
Neurological symptoms such as confusion, weakness, or visual changes
Call NHS 111 or contact your GP or diabetes care team if:
Hiccups persist for more than 48 hours
Hiccups are frequent, distressing, or interfering with eating, sleeping, or daily activities
You experience worsening gastrointestinal symptoms alongside hiccups
You have concerns about whether your symptoms are related to Ozempic
Your healthcare provider will take a thorough history and may perform an examination to exclude other causes of persistent hiccups, which can include gastro-oesophageal reflux disease (GORD), gastritis, central nervous system disorders, metabolic disturbances, or medication interactions. They will also assess whether your Ozempic dose is appropriate or whether dose adjustment might be beneficial.
If you experience severe, persistent abdominal pain with or without vomiting, which could indicate pancreatitis, you should stop taking Ozempic immediately and seek urgent medical attention, as advised in the SmPC. For other side effects, do not stop Ozempic without medical guidance, as this could lead to deterioration in glycaemic control. If hiccups or other side effects are problematic, your healthcare team can discuss management strategies or alternative treatment options whilst maintaining optimal diabetes management.
It's important to maintain adequate hydration, especially if experiencing gastrointestinal side effects, as severe vomiting or diarrhoea can lead to dehydration and potentially acute kidney injury.
If you experience hiccups whilst taking Ozempic, several practical strategies may help alleviate the symptom, particularly if it is related to the medication's gastrointestinal effects:
Dietary and lifestyle modifications:
Eat smaller, more frequent meals rather than large portions, which can reduce gastric distension
Eat slowly and chew food thoroughly to minimise air swallowing
Avoid carbonated beverages, which can increase gastric gas and distension
Identify and avoid personal trigger foods, particularly those that are spicy, fatty, or acidic
Remain upright for at least two hours after eating to reduce reflux risk
Avoid eating close to bedtime
Traditional hiccup remedies that may provide relief include controlled breathing techniques or sipping cold water slowly. Whilst the evidence base for these interventions is limited, they are safe and may interrupt the hiccup reflex.
Managing broader gastrointestinal side effects of Ozempic can also reduce the likelihood of hiccups. The Ozempic SmPC and British National Formulary (BNF) emphasise the importance of gradual dose titration to improve tolerability. The standard titration schedule starts with 0.25 mg once weekly for 4 weeks, then 0.5 mg once weekly for at least 4 weeks, before considering further increases if needed. If gastrointestinal symptoms are troublesome, discuss with your prescriber whether:
Slowing the rate of dose escalation might be appropriate
Anti-emetic medication could help manage nausea
Dietary advice from a dietitian might optimise symptom control
For constipation, ensure adequate fluid intake, increase dietary fibre gradually, and maintain physical activity. Short-term over-the-counter laxatives may be appropriate if needed, following NHS advice.
For persistent or intractable hiccups, your GP may consider pharmacological interventions such as proton pump inhibitors (if reflux is suspected). In rare cases, medications like baclofen or gabapentin might be considered for intractable hiccups, though these would be off-label uses requiring specialist input and careful assessment.
Maintaining open communication with your diabetes care team ensures that side effects are managed effectively whilst preserving the glycaemic benefits of Ozempic therapy. If you suspect you have experienced a side effect from Ozempic, you can report it directly to the MHRA through the Yellow Card scheme at https://yellowcard.mhra.gov.uk/, contributing to ongoing medication safety surveillance.
No, hiccups are not listed as an official side effect in UK prescribing information for Ozempic. Whilst some patients report hiccups anecdotally, there is no established clinical evidence linking semaglutide directly to this symptom.
Ozempic slows gastric emptying, which could lead to gastric distension, reflux, or altered vagus nerve signalling—all of which may theoretically trigger hiccups in susceptible individuals. However, this remains unproven in clinical studies.
Seek medical advice if hiccups persist for more than 48 hours, interfere with daily activities, or occur alongside severe abdominal pain, persistent vomiting, breathing difficulties, or signs of dehydration. These may indicate serious complications requiring urgent assessment.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.