Many people wonder about the best time to take GLP-1 probiotics to maximise potential benefits. These dietary supplements contain bacterial strains that may influence glucagon-like peptide-1 (GLP-1) production in the gut, though they differ fundamentally from prescription GLP-1 medications. Whilst research remains preliminary, understanding optimal timing, whether to take them with food, and what to expect can help you use these supplements safely. This article examines the evidence around GLP-1 probiotics, practical guidance on timing and administration, and important safety considerations for UK patients.
Quick Answer: The best time to take GLP-1 probiotics is typically with meals or just before eating, as food provides a buffering effect that helps bacterial strains survive stomach acid and reach the intestines.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereThe term 'GLP-1 probiotics' refers to dietary supplements marketed to potentially influence glucagon-like peptide-1 (GLP-1) production in the gut. These are not a formally recognised therapeutic class. GLP-1 is an incretin hormone naturally secreted by enteroendocrine L-cells in the intestinal lining, primarily in response to nutrient intake. This hormone plays a crucial role in glucose homeostasis by stimulating insulin secretion, suppressing glucagon release, slowing gastric emptying, and promoting satiety.
The proposed mechanism centres on the gut microbiome's influence on metabolic health. Specific strains within the Lactobacillus and Bifidobacterium genera may modulate the gut environment through several pathways. These include producing short-chain fatty acids (SCFAs) such as butyrate and propionate, which can stimulate L-cell activity and enhance GLP-1 secretion. Additionally, certain bacterial strains may influence bile acid metabolism and reduce low-grade inflammation, both of which affect incretin hormone production.
It is important to note that GLP-1 probiotics are not pharmaceutical GLP-1 receptor agonists (such as semaglutide or liraglutide) prescribed for type 2 diabetes or weight management. Whilst prescription GLP-1 medications are rigorously tested and regulated by the MHRA, probiotic supplements fall under food supplement regulations with less stringent evidence requirements. In the UK, supplements cannot legally make claims about treating or preventing disease or promoting weight loss.
Importantly, probiotics should never be used as a substitute for prescribed GLP-1 receptor agonists or other diabetes/weight management therapies. Always consult your GP or diabetes team before making changes to your treatment plan.
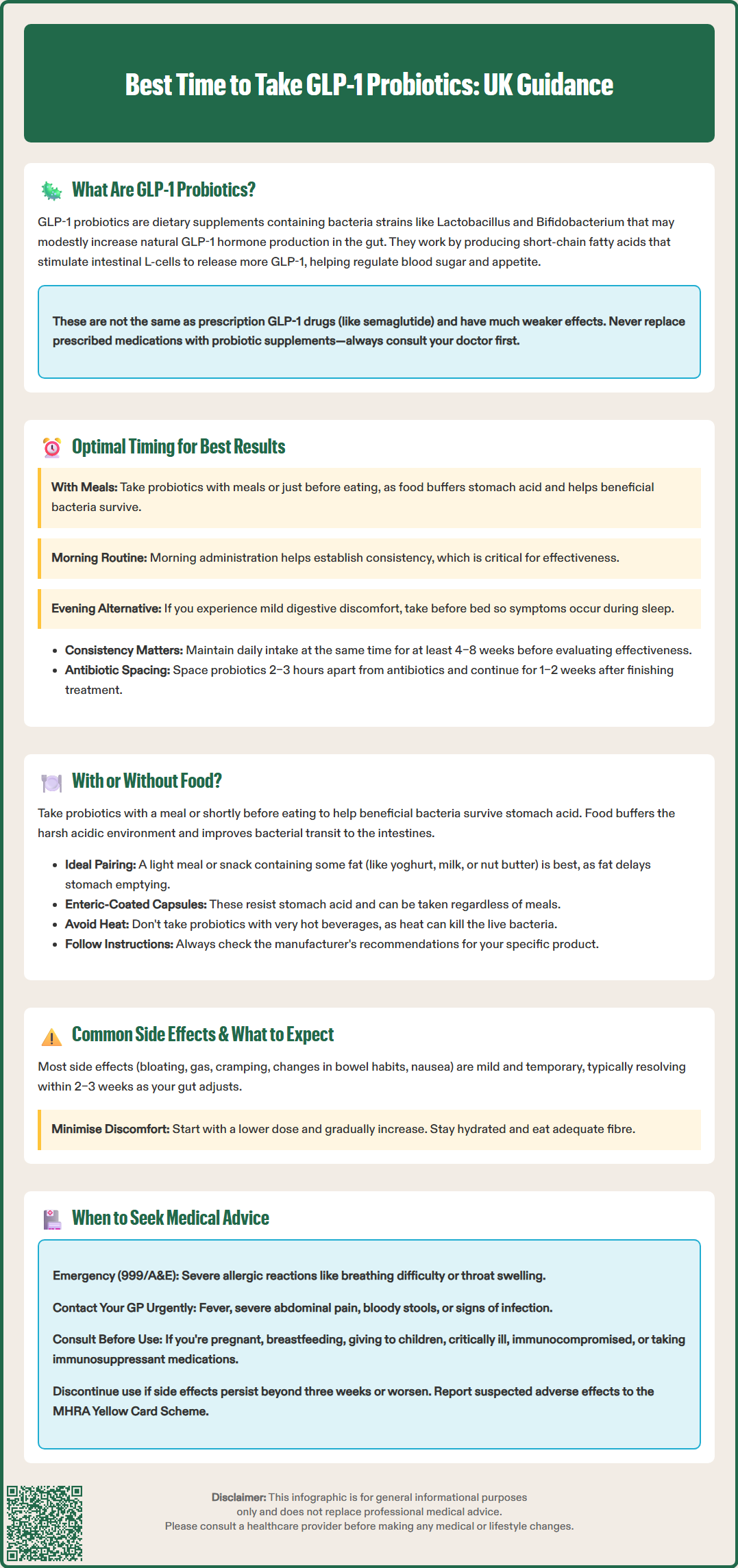
The optimal timing for taking GLP-1 probiotics depends on several factors, including the specific bacterial strains, formulation characteristics, and individual digestive patterns. Whilst there is no universally established 'best' time supported by extensive clinical evidence, general probiotic principles offer practical guidance.
Taking probiotics with meals or just before eating is often beneficial for many Lactobacillus and Bifidobacterium strains. Although gastric acid production increases during meals, food provides a buffering effect that can create a more hospitable environment for bacterial transit. A light meal containing some fat may particularly improve probiotic survival by slowing gastric emptying and providing additional buffering.
Some individuals prefer morning administration to establish a consistent routine, which enhances adherence—a critical factor for probiotic efficacy. Regular intake is important because most probiotics exert transient effects rather than permanently colonising the gut.
Alternatively, evening administration before bed may suit those who experience mild digestive discomfort from probiotics, as any transient symptoms occur during sleep.
Consistency is paramount—regular daily intake at the same time supports ongoing probiotic activity. For many gastrointestinal conditions, probiotic benefits typically emerge after 4–8 weeks of continuous use, though evidence specifically for metabolic outcomes remains limited. Individual response varies considerably based on baseline microbiome composition, diet, medications, and health status. Patients should maintain their chosen schedule for at least one month before assessing effectiveness.
If taking multiple supplements or medications, spacing probiotics at least 2-3 hours apart from antibiotics is advisable to prevent bacterial destruction. Consider continuing probiotics for 1-2 weeks after completing an antibiotic course, as tolerated. Always follow the manufacturer's specific instructions, as these are based on stability testing for that particular product.
The question of whether to take GLP-1 probiotics with or without food lacks definitive evidence specific to GLP-1-promoting strains, but general probiotic research provides useful guidance. The decision hinges on gastric acid exposure and formulation type.
Probiotic bacteria must survive the harsh acidic environment of the stomach (pH 1.5–3.5) to reach the intestines where they exert beneficial effects. While gastric acid production increases during and after meals, food also provides a buffering effect that raises the luminal pH, creating a more hospitable environment for bacterial transit. Research suggests that taking probiotics with a meal or shortly before eating may optimise survival for many strains, particularly when the meal contains some fat, which further delays gastric emptying and extends buffering effects.
Formulation matters considerably. Enteric-coated capsules are specifically designed to resist gastric acid and dissolve in the higher pH environment of the small intestine, making timing relative to meals less critical. Standard capsules or powders may benefit more from food-associated buffering. Always follow manufacturer instructions, as specific strains and delivery systems may have tailored recommendations based on stability testing.
For GLP-1-focused probiotics specifically, some suggest taking them before meals might theoretically align with enhancing postprandial GLP-1 secretion, though this remains speculative and is not supported by clinical outcome data. Some formulations combine probiotics with prebiotics (fermentable fibres that feed beneficial bacteria), which are best taken with food to minimise digestive discomfort.
Practical recommendations include starting with the manufacturer's guidance, taking probiotics with a light meal or snack containing some fat (such as yoghurt, milk, or a small amount of nut butter), and monitoring individual tolerance. If gastrointestinal symptoms develop, adjusting timing or taking with more substantial food may help. Avoid taking probiotics with very hot beverages, as heat can destroy live bacteria.
GLP-1 probiotics are generally well-tolerated, with most adverse effects being mild and transient. Understanding potential side effects helps patients distinguish normal adjustment responses from concerning symptoms requiring medical attention.
Common gastrointestinal effects may occur, particularly during the first 1–2 weeks as the gut microbiome adjusts. These include:
Bloating and gas: Increased bacterial fermentation produces gases, causing abdominal distension and flatulence
Mild abdominal discomfort or cramping: Usually resolves as the microbiome stabilises
Changes in bowel habits: Temporary loose stools or, less commonly, constipation
Nausea: Occasionally reported, particularly if taken on an empty stomach
These symptoms typically diminish within 2–3 weeks of consistent use. Starting with a lower dose and gradually increasing can minimise discomfort. Staying well-hydrated and maintaining adequate dietary fibre supports microbiome adaptation.
Rare but serious concerns warrant immediate medical attention. Individuals who are immunocompromised, have central venous catheters, or suffer from severe intestinal barrier dysfunction face a theoretical risk of probiotic-related bacteraemia or fungaemia. Call 999 or attend A&E if you experience severe allergic reactions (breathing difficulty, throat/tongue swelling). Contact your GP urgently if you experience fever, severe abdominal pain, bloody stools, or signs of systemic infection.
Allergic reactions to probiotic ingredients (including dairy-derived components or additives) are uncommon but possible. Symptoms include rash, itching, or difficulty breathing.
Important safety considerations: Seek medical advice before using probiotics if you are pregnant, breastfeeding, considering use in infants/children, or are critically ill/hospitalised. Theoretical interactions with immunosuppressant medications may occur; patients on such treatments should consult their specialist. There is currently no official link between standard probiotic use and serious adverse outcomes in healthy individuals, but long-term safety data for specific GLP-1-promoting formulations remain limited. If side effects persist beyond three weeks or worsen over time, discontinue use and consult your GP or a registered dietitian for personalised advice.
Report any suspected side effects to the MHRA Yellow Card Scheme at yellowcard.mhra.gov.uk.
No, GLP-1 probiotics are dietary supplements that may modestly influence gut hormone production, whilst prescription GLP-1 receptor agonists are rigorously tested pharmaceutical treatments for type 2 diabetes and weight management. Never substitute probiotics for prescribed medications without consulting your GP or diabetes team.
Probiotic benefits typically emerge after 4–8 weeks of consistent daily use, though evidence for metabolic outcomes remains limited. Individual response varies considerably based on baseline gut health, diet, and other factors.
Space probiotics at least 2–3 hours apart from antibiotics to prevent bacterial destruction. Consider continuing probiotics for 1–2 weeks after completing your antibiotic course, and consult your GP if you have concerns about interactions.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.