Can weight loss injections cause diarrhoea? Yes, diarrhoea is a recognised adverse effect of GLP-1 receptor agonist weight loss injections such as semaglutide (Wegovy) and liraglutide (Saxenda). Clinical trials report diarrhoea in approximately 9–20% of patients, typically during initial treatment or dose escalation. These medications affect gastrointestinal function by slowing gastric emptying and modulating intestinal motility. Whilst most cases are mild to moderate and self-limiting, understanding the mechanisms, management strategies, and when to seek medical advice is essential for patients considering or currently using these treatments for weight management in the UK.
Quick Answer: Weight loss injections, particularly GLP-1 receptor agonists such as semaglutide and liraglutide, can cause diarrhoea in approximately 9–20% of patients, typically during initial treatment or dose escalation.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWeight loss injections, primarily glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have become increasingly prescribed for weight management in the UK. These medications were originally developed for type 2 diabetes management but have gained specific licensing for obesity treatment when used alongside lifestyle modifications. It's important to note that while Wegovy and Saxenda are licensed for weight management, Ozempic (also semaglutide) is only licensed for type 2 diabetes treatment in the UK and is not approved for weight loss on the NHS.
Diarrhoea is indeed a recognised adverse effect of weight loss injections, occurring in a substantial proportion of patients. The gastrointestinal system is particularly affected because GLP-1 receptors are distributed throughout the digestive tract. When these receptors are activated by medication, they influence various aspects of gut function.
Other common gastrointestinal side effects associated with these injections include:
Nausea (the most frequently reported symptom)
Vomiting
Constipation
Abdominal pain or discomfort
Bloating and flatulence
Reduced appetite
The severity and duration of these symptoms vary considerably between individuals. Most gastrointestinal side effects, including diarrhoea, tend to be most pronounced during the initial weeks of treatment or following dose escalation. Understanding these effects and implementing appropriate management strategies can significantly improve treatment tolerance and adherence, ultimately supporting successful weight loss outcomes.
Access to these medications in the UK is governed by specific NICE criteria, including BMI thresholds and the presence of weight-related comorbidities, and they must be prescribed within appropriate specialist services.
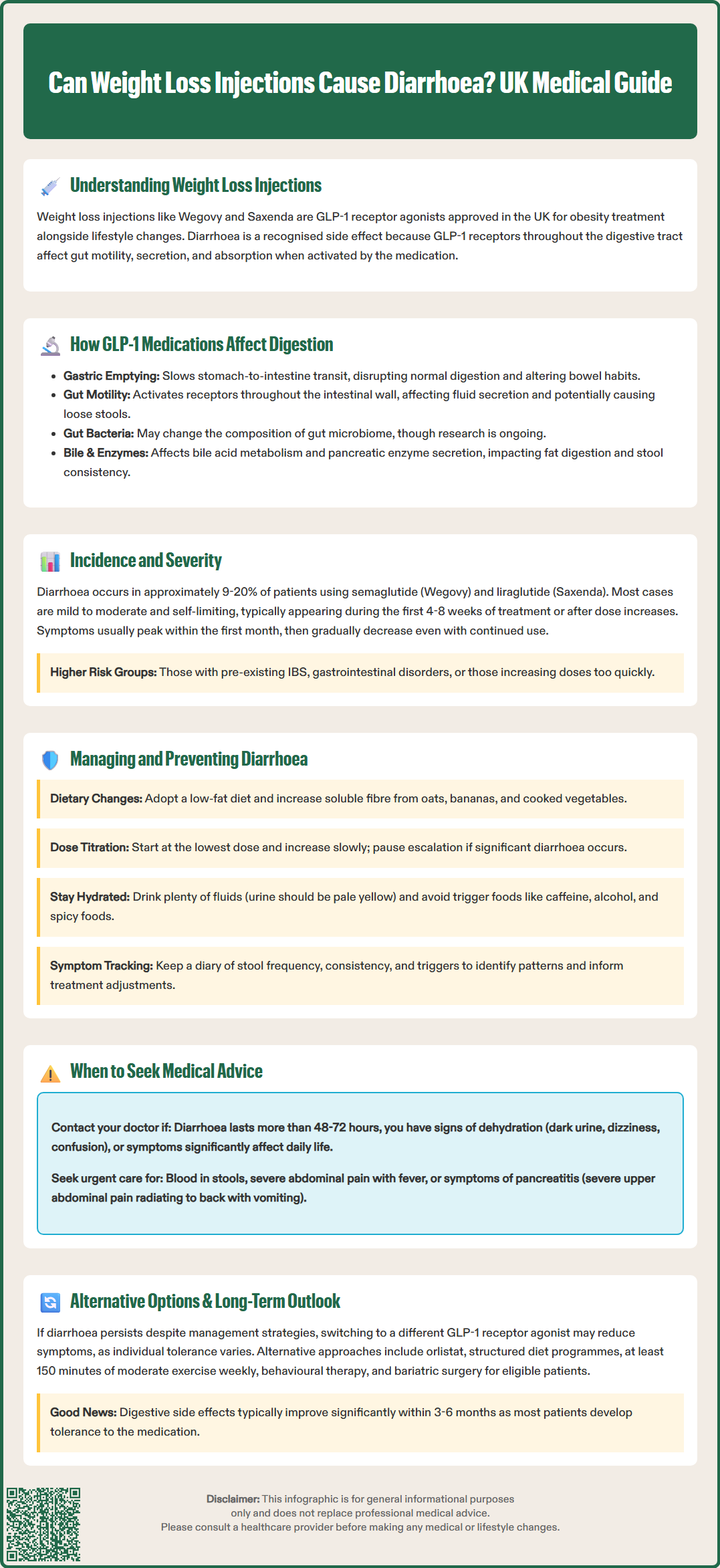
GLP-1 receptor agonists exert their effects through multiple physiological mechanisms that influence bowel function. The primary mechanism for weight loss is central appetite suppression through direct action on the brain's appetite-regulating centres. Additionally, these medications cause delayed gastric emptying, particularly in the early stages of treatment, which contributes to feelings of fullness but tends to attenuate over time with continued use.
The pharmacological action extends throughout the gastrointestinal tract. GLP-1 receptors are present on enteric neurons and smooth muscle cells within the intestinal wall. When activated, they modulate intestinal motility patterns, which can affect transit through different segments of the bowel. This altered gut motility can contribute to changes in bowel habits, including diarrhoea in some individuals.
Research has observed changes in gut microbiota composition with GLP-1 receptor agonist therapy, though the clinical significance remains under investigation and these effects should be considered preliminary rather than established mechanisms for digestive symptoms.
GLP-1 receptor agonists also influence bile acid metabolism, which may contribute to their effects on glucose metabolism and potentially to some gastrointestinal symptoms. Importantly, these medications are associated with an increased risk of gallbladder disease, including gallstones, which can present with upper abdominal pain and other digestive symptoms.
The multifaceted impact on digestive physiology explains why gastrointestinal side effects are so prevalent with this medication class, though the specific mechanisms behind diarrhoea may vary between individuals and are not fully understood.
Clinical trial data provide substantial evidence regarding the incidence of diarrhoea with weight loss injections. In pivotal STEP trials for semaglutide (Wegovy), diarrhoea was reported in approximately 20-30% of participants, making it one of the most common adverse effects after nausea. For liraglutide (Saxenda), similar rates have been documented, with diarrhoea affecting roughly 20% of users during clinical studies. These figures significantly exceed the incidence observed in placebo groups, confirming a clear association between the medication and this gastrointestinal symptom.
The severity of diarrhoea varies considerably among patients. Most cases are classified as mild to moderate according to clinical trial criteria, without significant systemic symptoms. These episodes are generally self-limiting and improve as the body adapts to the medication. A smaller percentage of patients experience more severe diarrhoea that may necessitate dose reduction or treatment discontinuation, as documented in the medicines' Summary of Product Characteristics (SmPCs).
Timing patterns are clinically significant. Diarrhoea most commonly emerges during the initial 4-8 weeks of treatment or following dose escalation. This temporal relationship reflects the body's adjustment period to the medication's effects on gastrointestinal function. Symptoms typically peak within the first month and gradually diminish over subsequent weeks, even with continued treatment.
Certain patient factors may influence the risk of developing diarrhoea, including:
Pre-existing irritable bowel syndrome
History of other gastrointestinal disorders
Concurrent medications affecting gut motility
Rate of dose escalation
Clinical experience suggests that while diarrhoea is common, it rarely leads to serious complications when appropriately monitored and managed according to UK clinical guidance.
Effective management of diarrhoea associated with weight loss injections involves both preventative strategies and symptomatic treatment approaches. Dietary modifications represent a first-line intervention and can help reduce symptom severity. Patients may benefit from eating smaller, more frequent meals and identifying personal trigger foods that worsen symptoms. Some find that temporarily reducing fatty or spicy foods, caffeine, alcohol, and artificial sweeteners can be helpful during the adaptation period.
Gradual dose titration is crucial for minimising gastrointestinal side effects. UK prescribing guidelines recommend starting at the lowest available dose and increasing slowly according to the specific schedule in each product's SmPC. This approach allows the digestive system to adapt progressively to the medication's effects. Patients who experience significant diarrhoea may benefit from temporarily maintaining their current dose rather than escalating, or even reducing to the previous dose level until symptoms resolve, under clinician guidance.
Practical management strategies include:
Maintaining adequate hydration: Drinking regular small amounts of fluid throughout the day, with oral rehydration solutions if diarrhoea is persistent
Avoiding identified trigger foods: Personalising dietary adjustments based on individual responses
Eating smaller, frequent meals: Reducing the burden on the digestive system
Keeping a symptom diary: Documenting stool frequency, consistency, and associated factors to identify patterns
Pharmacological interventions may be appropriate for persistent symptoms. Loperamide (available over-the-counter) can be used short-term for symptomatic relief, though regular use should be discussed with a healthcare provider. For persistent symptoms, patients should consult their prescriber or pharmacist for individualised advice.
Patients should be aware that gastrointestinal symptoms often improve with time, and that treatment benefits should be weighed against side effects during follow-up appointments. NICE guidance includes specific continuation criteria, such as achieving at least 5% weight loss at 12 weeks on the maintenance dose of liraglutide (Saxenda).
Whilst mild diarrhoea is an expected side effect of weight loss injections, certain presentations warrant prompt medical evaluation. Patients should contact their GP or prescribing clinician if they experience:
Severe or persistent diarrhoea lasting more than 48-72 hours despite conservative management
Signs of dehydration, including reduced urine output, dark-coloured urine, dizziness, confusion, or persistent thirst
Blood in stools or black, tarry stools (melaena)
Severe abdominal pain, particularly if localised or accompanied by fever
Unintentional weight loss beyond expected therapeutic effects
Inability to maintain adequate oral fluid intake due to concurrent vomiting
Urgent medical attention is required if patients develop symptoms suggestive of serious complications, including acute pancreatitis (severe upper abdominal pain radiating to the back, often with vomiting) or gallbladder disease (pain in the right upper abdomen, fever, or yellowing of the skin/eyes). These are recognised risks with GLP-1 receptor agonists, and early recognition is essential.
Patients should also seek medical review if diarrhoea significantly impacts quality of life or daily functioning, even if not medically severe. Treatment adjustments may be necessary, including dose reduction, temporary treatment interruption, or switching to an alternative weight management strategy. The prescribing clinician can assess whether the benefits of continuing the injection outweigh the adverse effects.
Regular monitoring appointments are essential for all patients receiving weight loss injections, with frequency determined by local service protocols and NICE guidance. During these consultations, healthcare providers assess treatment efficacy, side effect profile, and overall tolerability. Patients should prepare for these appointments by documenting their symptoms to facilitate informed decision-making about ongoing management.
Patients are encouraged to report suspected side effects to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk), which helps monitor the safety of medicines in the UK.
For patients who experience intolerable diarrhoea despite management strategies, several alternative approaches to weight management should be considered. Under clinician guidance, switching between different GLP-1 receptor agonists may be an option, as individual responses vary between medications within this class. However, there is no definitive evidence predicting which patients will respond better to specific agents.
Orlistat, a lipase inhibitor that reduces fat absorption, represents an alternative pharmacological option with a different mechanism of action, though it also carries gastrointestinal side effects including oily or fatty stools. Newer medications such as tirzepatide (a dual GIP/GLP-1 receptor agonist) have shown promising efficacy in clinical trials, though UK availability for weight management is subject to regulatory approval and NICE assessment.
Non-pharmacological interventions remain fundamental to successful weight management and may be sufficient for some individuals. NICE recommends a multicomponent approach including:
Structured dietary programmes with professional support
Regular physical activity (minimum 150 minutes moderate-intensity weekly)
Behavioural therapy addressing eating patterns and psychological factors
Consideration of bariatric surgery for those meeting eligibility criteria (typically BMI ≥40 kg/m² or ≥35 kg/m² with comorbidities)
Long-term outlook for gastrointestinal symptoms is generally favourable. Data from the STEP clinical trials demonstrate that diarrhoea and other digestive side effects typically diminish significantly after the first 3-6 months of treatment, even with continued medication use. Most patients who persist with therapy develop tolerance to these effects. However, symptoms may recur temporarily with dose increases or following treatment interruptions.
Emerging research continues to explore strategies for minimising gastrointestinal side effects whilst maintaining therapeutic efficacy. Future developments may enable more personalised approaches to weight loss injection therapy, improving both tolerability and outcomes for patients requiring pharmacological support for obesity management within the UK healthcare system.
Clinical trials show diarrhoea occurs in approximately 9% of patients taking semaglutide (Wegovy) and 10–20% of those taking liraglutide (Saxenda). Most cases are mild to moderate and improve within the first few months of treatment.
Diarrhoea most commonly occurs during the first 4–8 weeks of treatment or following dose increases, typically peaking within the first month. Symptoms usually diminish significantly after 3–6 months as the body adapts to the medication.
Contact your GP or prescribing clinician if diarrhoea persists beyond 48–72 hours, if you develop signs of dehydration, notice blood in stools, or experience severe abdominal pain. Your healthcare provider may recommend dose adjustment or temporary treatment interruption.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.