Weight loss injections, particularly GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), are increasingly prescribed for obesity management in the UK. Whilst concerns about potential liver problems naturally arise with any medication, current evidence suggests that serious hepatic complications are uncommon with approved weight loss injections. Interestingly, these medications may actually improve liver health in many patients by reducing hepatic fat accumulation associated with obesity. Understanding the relationship between weight loss injections and liver function, recognising warning signs, and knowing when to seek medical advice are essential for safe treatment. This article examines the evidence, risk factors, and monitoring strategies to help patients and healthcare professionals make informed decisions.
Quick Answer: Serious liver problems are uncommon with approved weight loss injections, and these medications may actually improve liver health by reducing hepatic fat in patients with obesity.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWeight loss injections, particularly glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have become increasingly prescribed for obesity management in the UK. These medications work by mimicking natural hormones that regulate appetite and blood glucose levels, leading to reduced food intake and subsequent weight loss. As with any pharmacological intervention, understanding their potential effects on vital organs, particularly the liver, is essential for both patients and healthcare professionals.
The liver plays a central role in drug metabolism, processing many medications that enter the body, though renal and other elimination pathways are also important for certain drugs. The liver is responsible for breaking down pharmaceutical compounds, converting them into forms that can be utilised or eliminated. This metabolic function means the liver is potentially vulnerable to drug-induced injury, though such occurrences vary significantly depending on the medication, dosage, duration of treatment, and individual patient factors.
The relationship between weight loss injections and liver health is complex and multifaceted. Interestingly, obesity itself is a major risk factor for non-alcoholic fatty liver disease (NAFLD), which affects approximately one quarter of the UK population according to the British Liver Trust. Weight loss achieved through any means—including these injections—can actually improve liver health by reducing hepatic fat accumulation. However, questions remain about whether the medications themselves might pose direct hepatotoxic risks.
It's also worth noting that GLP-1 receptor agonists and rapid weight loss can increase the risk of gallstone formation, which may present with symptoms that mimic liver problems, including right upper quadrant pain and jaundice.
Current evidence from clinical trials and post-marketing surveillance provides reassurance that serious liver problems are uncommon with approved weight loss injections. The Medicines and Healthcare products Regulatory Agency (MHRA) continues to monitor safety data, and healthcare professionals may consider baseline liver function and ongoing monitoring based on clinical judgement and individual patient risk factors.
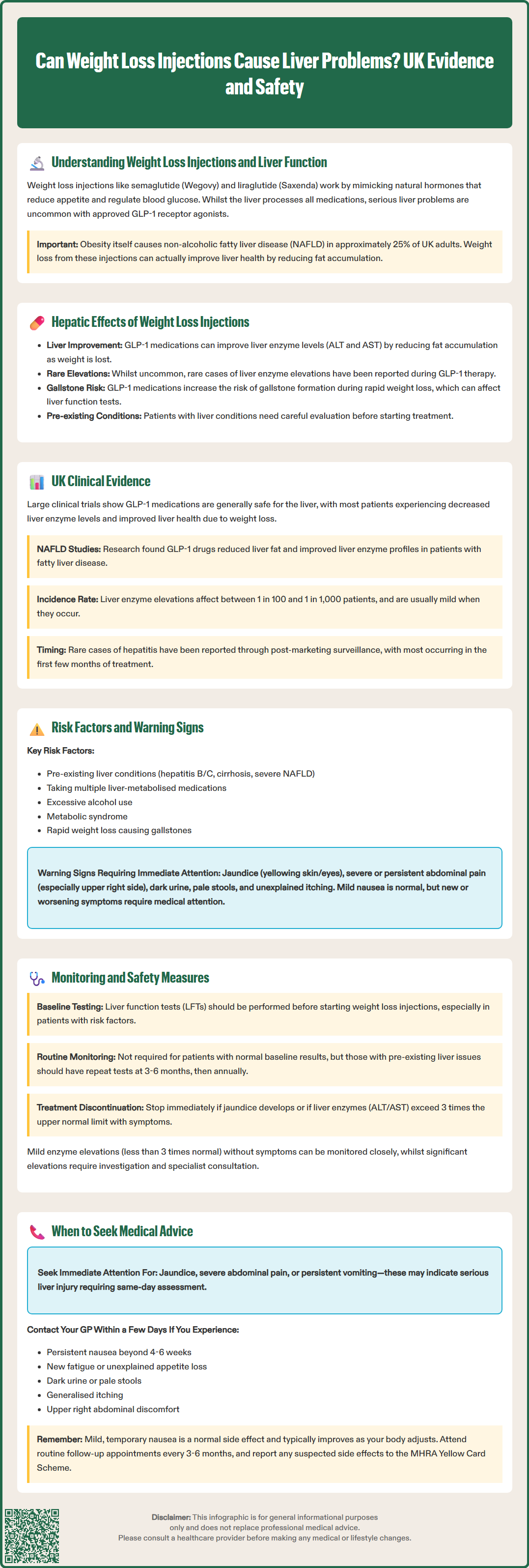
GLP-1 receptor agonists represent the most commonly prescribed weight loss injections in the UK. Semaglutide (Wegovy) and liraglutide (Saxenda) are licensed specifically for weight management, whilst other GLP-1 agonists like dulaglutide are primarily used for type 2 diabetes. Tirzepatide (Mounjaro) is currently licensed in the UK for type 2 diabetes management, not for weight loss. These medications work by activating GLP-1 receptors in the pancreas, brain, and gastrointestinal tract, leading to increased insulin secretion, reduced glucagon secretion, delayed gastric emptying, and reduced appetite. Importantly, clinical trial data has generally shown that GLP-1 agonists may actually improve liver enzyme levels in patients with obesity and NAFLD, rather than causing harm.
The STEP (Semaglutide Treatment Effect in People with obesity) trials demonstrated that weight loss achieved with semaglutide can lead to reductions in alanine aminotransferase (ALT) and aspartate aminotransferase (AST)—liver enzymes that, when elevated, indicate hepatic inflammation or damage. This improvement is thought to result from reduced hepatic steatosis (fat accumulation) as patients lose weight. However, isolated case reports have documented rare instances of liver enzyme elevations during GLP-1 therapy, though causality is often difficult to establish given the multiple factors affecting liver health in obese patients.
It's important to note that cholelithiasis (gallstones) is a known adverse effect of GLP-1 receptor agonists and rapid weight loss, which can present with abnormal liver function tests.
Other injectable weight loss medications are less commonly used in the UK but warrant mention. Setmelanotide, a melanocortin-4 receptor agonist used for rare genetic obesity disorders, has limited clinical experience in patients with hepatic impairment. Historical weight loss injections, such as human chorionic gonadotropin (hCG), lack robust evidence for efficacy and are not licensed for weight management in the UK.
The hepatic safety profile of approved weight loss injections appears favourable overall, with potential benefits outweighing risks for most patients. Nevertheless, individual responses vary, and pre-existing liver conditions require careful consideration before initiating treatment.
Clinical trial evidence from large-scale studies of GLP-1 receptor agonists provides the most robust data on hepatic safety. The STEP trials, published in leading medical journals including the New England Journal of Medicine, reported that liver enzyme abnormalities were uncommon and generally mild when they occurred. In fact, mean ALT and AST levels decreased from baseline in treatment groups, reflecting improvements in liver health associated with weight loss.
A systematic review examining GLP-1 agonists in patients with NAFLD found that these medications led to significant reductions in liver fat content and improvements in liver enzyme profiles. The evidence suggests that for many patients, particularly those with obesity-related liver disease, GLP-1-based weight loss injections may be hepatoprotective rather than harmful. However, it is important to note that most clinical trials exclude patients with severe liver disease, limiting our understanding of safety in this population.
Post-marketing surveillance and case reports have documented rare instances of hepatic adverse events. The MHRA's Yellow Card scheme has received occasional reports of liver enzyme elevations, hepatitis, and cholestasis in patients receiving GLP-1 agonists, though these remain uncommon relative to the number of prescriptions issued. Establishing causality is challenging, as many patients have multiple risk factors for liver disease, including obesity, diabetes, and concurrent medications. Some cases of abnormal liver function tests may also be related to gallbladder disease, which is a known risk with GLP-1 receptor agonists and rapid weight loss.
There is no established causal relationship between approved weight loss injections and serious liver failure or chronic liver disease when used as directed. The European Medicines Agency (EMA) and MHRA continue to classify hepatic adverse events as uncommon or rare, and product information for semaglutide and liraglutide does not list liver toxicity as a common or expected side effect. Nonetheless, vigilance remains appropriate, particularly during the first months of treatment when most drug-induced liver injuries typically manifest.
If you suspect you have experienced a side effect from a weight loss injection, you can report this through the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Pre-existing liver conditions represent the most significant risk factor for potential hepatic complications during weight loss injection therapy. Patients with chronic hepatitis B or C, cirrhosis, or severe NAFLD may have reduced hepatic reserve and altered drug metabolism. Whilst mild-to-moderate NAFLD is not a contraindication—and may actually improve with treatment—advanced liver disease requires careful risk-benefit assessment and specialist input before initiating GLP-1 therapy.
Other risk factors include:
Concurrent hepatotoxic medications: Patients taking multiple drugs metabolised by the liver, including certain antibiotics, paracetamol in high doses, or multiple medications simultaneously may face increased risk. While statins are sometimes mentioned in this context, significant statin-related liver injury is rare
Alcohol consumption: Excessive alcohol intake compounds hepatic stress and should be addressed before starting treatment
Metabolic syndrome components: Diabetes, hypertension, and dyslipidaemia—whilst often indications for weight loss therapy—can independently affect liver health
Genetic factors: Rare genetic variations affecting drug metabolism may predispose certain individuals to adverse hepatic reactions
Warning signs of liver problems that patients should recognise include:
Persistent nausea or vomiting (beyond the initial adjustment period typical with GLP-1 agonists)
Unusual fatigue or weakness
Loss of appetite
Abdominal pain, particularly in the upper right quadrant (which may also indicate gallbladder problems)
Dark urine or pale stools
Yellowing of the skin or whites of the eyes (jaundice)
Unexplained itching
It is important to note that many of these symptoms are non-specific and may have other causes. Mild nausea, for instance, is a common and expected side effect of GLP-1 agonists that typically improves within weeks. However, new or worsening symptoms, particularly jaundice or severe abdominal pain, warrant prompt medical evaluation. Patients should not discontinue prescribed medications without consulting their healthcare professional, as abrupt cessation may have other health implications.
Baseline assessment before initiating weight loss injections should include a comprehensive medical history and physical examination. Based on clinical judgement and individual risk factors, healthcare professionals may consider baseline blood tests, including liver function tests (LFTs), particularly in patients with risk factors for liver disease. Standard LFTs measure ALT, AST, alkaline phosphatase (ALP), gamma-glutamyl transferase (GGT), bilirubin, and albumin, providing a snapshot of hepatic function.
For patients with normal baseline liver function and no risk factors, routine monitoring of LFTs during GLP-1 therapy is not mandated by current UK guidelines or product information. However, clinical judgement should guide individualised monitoring strategies. Patients with pre-existing liver enzyme elevations or known liver disease may benefit from repeat LFTs after starting treatment, with frequency determined by the clinician based on individual risk assessment.
According to the Summary of Product Characteristics (SmPC), semaglutide requires no dose adjustment for patients with hepatic impairment, though there is limited experience in severe hepatic impairment. Liraglutide is not recommended for use in patients with severe hepatic impairment. Neither medication requires routine liver monitoring as per their SmPCs, reflecting the generally favourable safety profile observed in clinical trials. Nevertheless, healthcare professionals should remain vigilant for signs of liver dysfunction, particularly during dose escalation phases when side effects are most likely to emerge.
Additional safety measures include:
Patient education: Ensuring individuals understand potential warning signs and know when to seek medical advice
Medication review: Assessing all concurrent medications for potential drug interactions or cumulative hepatotoxic effects
Lifestyle counselling: Addressing alcohol consumption, promoting balanced nutrition, and encouraging physical activity to support overall liver health
Gradual dose titration: Following recommended dose escalation schedules to minimise side effects and allow monitoring of tolerance
For patients who develop elevated liver enzymes during treatment, the approach depends on severity. Mild elevations (less than three times the upper limit of normal) without symptoms may be monitored closely with repeat testing. Alternative causes, including gallstones, alcohol consumption, and viral hepatitis, should be considered. More significant elevations warrant investigation and may necessitate treatment discontinuation pending specialist hepatology input.
According to NICE guidance, GLP-1 receptor agonists should be discontinued if a patient does not achieve at least 5% weight loss after the specified period at the maintenance dose.
Immediate medical attention is required if patients experience symptoms suggestive of acute liver injury, particularly jaundice, severe abdominal pain, or persistent vomiting. These symptoms warrant same-day assessment, either through urgent GP appointment, NHS 111, or attendance at A&E. Call 999 if severely unwell. Jaundice, in particular, indicates significant hepatic dysfunction or biliary obstruction and requires prompt investigation regardless of its cause.
Patients should contact their GP within a few days if they experience:
Persistent nausea or vomiting lasting beyond the expected adjustment period (typically 4-6 weeks)
New or worsening fatigue that interferes with daily activities
Unexplained loss of appetite
Dark urine or pale stools
Generalised itching without obvious skin cause
Abdominal discomfort, particularly in the upper right side
It is worth emphasising that mild, transient nausea is an expected side effect of GLP-1 receptor agonists and does not typically indicate liver problems. This symptom usually improves as the body adjusts to the medication. However, if nausea is severe, persistent, or accompanied by other concerning features, medical review is appropriate.
Routine follow-up with the prescribing healthcare professional is essential for all patients receiving weight loss injections. These appointments provide opportunities to assess treatment response, monitor for adverse effects, and conduct any indicated blood tests. Follow-up should align with the recommendations in the SmPC and NICE guidance, which include assessment of treatment effectiveness and continuation criteria (e.g., achieving at least 5% weight loss after the specified period at the maintenance dose).
For individuals with pre-existing liver disease, closer liaison with hepatology services may be appropriate. Specialist input can help optimise the risk-benefit balance and establish appropriate monitoring protocols. The decision to initiate or continue weight loss injections in patients with significant liver disease should be made collaboratively between the patient, their GP, and specialist services.
Finally, patients should inform all healthcare professionals about their use of weight loss injections, as this information is relevant when interpreting symptoms, blood tests, or prescribing additional medications. If you suspect you have experienced a side effect from a weight loss injection, you can report this through the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk). Open communication ensures coordinated care and optimal safety monitoring throughout the treatment journey.
Mild-to-moderate non-alcoholic fatty liver disease (NAFLD) is not a contraindication to GLP-1 weight loss injections, and these medications may actually improve liver health by reducing hepatic fat accumulation. However, patients with advanced liver disease or cirrhosis require specialist assessment before starting treatment.
Warning signs include jaundice (yellowing of skin or eyes), severe abdominal pain (particularly upper right side), dark urine, pale stools, persistent vomiting, and unexplained itching. These symptoms warrant prompt medical evaluation, though mild nausea is a common and expected side effect that typically improves within weeks.
Routine liver function monitoring is not mandated for patients with normal baseline results and no risk factors. However, baseline tests are recommended for those with risk factors, and patients with pre-existing liver enzyme elevations may benefit from repeat testing at 3–6 months, then annually or as clinically indicated.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.