
Many people with type 2 diabetes and obesity wonder whether metformin and Wegovy can be taken together safely. The short answer is yes—these medications work through different mechanisms and are pharmacologically compatible. Metformin, a biguanide that reduces hepatic glucose production and improves insulin sensitivity, has been a cornerstone of diabetes management for decades. Wegovy (semaglutide 2.4mg), a GLP-1 receptor agonist licensed for weight management, addresses appetite regulation and glucose homeostasis. This article explores the evidence for combining these treatments, potential benefits, safety considerations, and guidance on accessing this combination therapy within the UK healthcare system.
Quick Answer: Metformin and Wegovy can be taken together safely, as they work through complementary mechanisms without significant drug interactions.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMetformin and Wegovy (semaglutide) are two distinct medications used in the management of type 2 diabetes and weight control, each working through different mechanisms to achieve therapeutic benefits.
Metformin is a biguanide medication that has been the first-line treatment for type 2 diabetes for decades. It primarily works by reducing hepatic glucose production in the liver, improving insulin sensitivity in peripheral tissues, and decreasing intestinal absorption of glucose. Metformin does not stimulate insulin secretion, which means it carries a very low risk of causing hypoglycaemia when used alone. Metformin has shown potential cardiovascular benefits, particularly in the UKPDS study, though subsequent evidence has been mixed. It is generally well-tolerated and remains a cornerstone of diabetes management according to NICE guideline NG28.
Wegovy (semaglutide 2.4mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed specifically for weight management in adults with obesity or overweight with weight-related comorbidities. In the UK, NICE Technology Appraisal 875 restricts NHS access to specialist weight management services, typically for people with BMI ≥35 kg/m² with at least one weight-related comorbidity (with adjusted thresholds for certain ethnic groups). Semaglutide mimics the action of the naturally occurring hormone GLP-1, which is released after eating. It works by stimulating insulin secretion in a glucose-dependent manner, suppressing glucagon release, slowing gastric emptying, and—crucially for weight loss—reducing appetite through effects on brain centres that regulate hunger. The medication is administered once weekly via subcutaneous injection.
Whilst metformin primarily targets insulin resistance and hepatic glucose output, Wegovy addresses multiple pathways including appetite regulation and glucose homeostasis. Understanding these complementary mechanisms is essential when considering whether these medications can be used together safely and effectively.
Yes, metformin and Wegovy can be taken together, and this combination is pharmacologically compatible. There is no contraindication to using these medications concurrently, and clinical trials of semaglutide have included participants already taking metformin.
The MHRA (Medicines and Healthcare products Regulatory Agency) has approved both medications for use in the UK, and studies have demonstrated that the combination is generally safe and well-tolerated. The medications work through different mechanisms—metformin primarily addressing insulin resistance and hepatic glucose production, whilst Wegovy targets appetite regulation and incretin pathways—meaning they complement rather than interfere with each other's actions.
Important considerations when taking both medications include understanding that they do not have significant drug-drug interactions at the pharmacokinetic level. Metformin is not metabolised by the liver and is excreted unchanged by the kidneys, whilst semaglutide is broken down by protein degradation pathways. This means neither medication significantly affects the blood levels or effectiveness of the other.
However, Wegovy does delay gastric emptying, which may affect the absorption of some oral medications. If you are taking medicines with a narrow therapeutic index (such as warfarin), additional monitoring (e.g., INR) may be required when starting or adjusting Wegovy.
It's important to note that Wegovy should not be used concomitantly with other GLP-1 receptor agonists (such as Ozempic, which contains the same active ingredient at lower doses but is licensed for diabetes rather than weight management).
It is essential that any combination therapy is prescribed and monitored by a healthcare professional. Your GP or specialist will assess your individual circumstances, including your current health status, other medications you may be taking, kidney function (particularly important for metformin), and treatment goals. Self-medicating or combining these medications without medical supervision is not advisable, as proper dosing, monitoring, and adjustment are crucial for both safety and effectiveness.
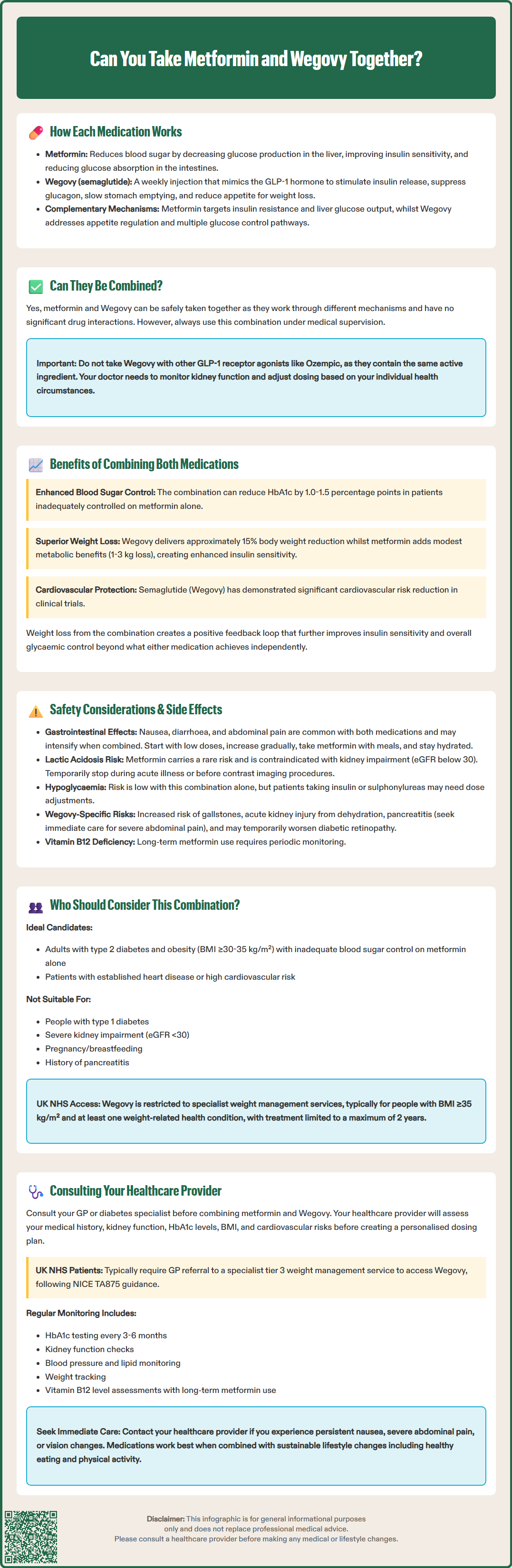
Combining metformin and Wegovy may offer additive benefits for patients with type 2 diabetes and obesity, addressing multiple aspects of metabolic health simultaneously.
Enhanced glycaemic control is a primary advantage of this combination. Metformin's action on hepatic glucose production and insulin sensitivity, combined with Wegovy's glucose-dependent insulin secretion and glucagon suppression, can lead to improved HbA1c levels compared to either medication alone. Clinical evidence from trials such as the SUSTAIN programme suggests that GLP-1 receptor agonists like semaglutide, when added to metformin therapy, can reduce HbA1c by approximately 1.0–1.5 percentage points in patients with inadequate control on metformin monotherapy, though results vary depending on baseline HbA1c and individual factors.
Superior weight loss outcomes represent another significant benefit. Whilst metformin may produce modest weight loss (typically 1–3 kg), Wegovy has demonstrated substantial weight reduction in clinical trials. The STEP 1 trial showed that semaglutide 2.4mg produced average weight loss of approximately 15% of body weight after 68 weeks. When combined with metformin's metabolic benefits, patients may experience more comprehensive improvements in body composition and metabolic parameters. This weight loss can further enhance insulin sensitivity, creating a positive feedback loop for glycaemic control.
Cardiovascular risk reduction is an important consideration. Metformin showed cardiovascular benefits in the UKPDS study, though subsequent evidence has been mixed. Semaglutide has demonstrated significant reductions in major adverse cardiovascular events in the SUSTAIN-6 trial (for the diabetes formulation) and more recently in the SELECT trial (for the 2.4mg dose in people with overweight/obesity). While the combination may offer benefits, it's important to note that additive cardioprotective effects of the combination have not been specifically studied in dedicated trials.
Complementary mechanisms mean that patients benefit from multiple therapeutic pathways being addressed simultaneously—insulin resistance, hepatic glucose output, appetite regulation, and incretin effects—providing a more comprehensive approach to metabolic disease management than either medication alone.
Whilst the combination of metformin and Wegovy is generally considered safe, patients should be aware of potential side effects and safety considerations associated with each medication and their combined use.
Gastrointestinal side effects are the most common concern with both medications. Metformin frequently causes nausea, diarrhoea, abdominal discomfort, and metallic taste, particularly when initiating therapy. Wegovy similarly causes gastrointestinal symptoms including nausea, vomiting, diarrhoea, constipation, and abdominal pain in a significant proportion of users. When taken together, these effects may be additive, potentially causing more pronounced digestive symptoms. Starting with lower doses and gradual titration, as recommended in the prescribing information, can help minimise these effects. Taking metformin with meals and ensuring adequate hydration may also reduce gastrointestinal discomfort.
Lactic acidosis is a rare but serious complication associated with metformin. According to UK guidance, metformin is contraindicated in patients with eGFR below 30 mL/min/1.73m², should not be initiated in those with eGFR 30-44 mL/min/1.73m², and requires dose review/reduction for eGFR 30-59 mL/min/1.73m². Metformin should be temporarily discontinued during acute illness ('sick day rules') and around procedures involving iodinated contrast media. Conditions that may precipitate lactic acidosis—such as dehydration, severe infection, or excessive alcohol intake—require careful monitoring.
Hypoglycaemia risk is generally low with this combination, as neither metformin nor Wegovy typically causes low blood sugar when used without other glucose-lowering medications. However, if you are also taking insulin or sulfonylureas, the risk increases and dose adjustments may be necessary.
Additional Wegovy safety considerations include:
Diabetic retinopathy complications: Particularly in patients with pre-existing retinopathy, rapid improvement in glucose control may temporarily worsen retinopathy
Gallbladder disease: Increased risk of gallstones and related complications
Acute kidney injury: Risk from severe gastrointestinal side effects leading to dehydration
Pancreatitis: Though uncommon, patients should seek immediate medical attention for severe, persistent abdominal pain
Long-term metformin use may lead to vitamin B12 deficiency, so periodic monitoring is advisable. The risk of thyroid C-cell tumours observed in rodent studies with GLP-1 agonists has not been confirmed in humans, but remains a precaution in the UK SmPC for Wegovy.
The combination of metformin and Wegovy may be particularly appropriate for specific patient populations who meet certain clinical criteria and treatment goals.
Adults with type 2 diabetes and obesity represent the primary group who may benefit from this combination. In the UK NHS, access to Wegovy is restricted by NICE Technology Appraisal 875 to specialist weight management services, typically for people with:
BMI ≥35 kg/m² with at least one weight-related comorbidity (lower thresholds may apply for people from certain ethnic backgrounds)
BMI ≥30 kg/m² who have been referred to specialist tier 3 services and meet specific criteria
Treatment is typically limited to a maximum of 2 years
For diabetes management, NICE guideline NG28 provides criteria for when GLP-1 receptor agonists may be appropriate (though this typically refers to Ozempic rather than Wegovy):
Inadequate glycaemic control on metformin and other oral therapies
BMI ≥35 kg/m² (adjusted for ethnicity) where weight loss would benefit obesity-related comorbidities, or
BMI <35 kg/m² where insulin would have significant occupational implications or weight loss would benefit other obesity-related comorbidities
Patients with established cardiovascular disease or high cardiovascular risk may particularly benefit, given the cardioprotective effects demonstrated by semaglutide in clinical trials. Those with a history of myocardial infarction, stroke, or peripheral arterial disease should discuss this option with their healthcare provider.
Individuals who have not achieved targets with lifestyle modification and metformin monotherapy are appropriate candidates for treatment intensification.
Contraindications and cautions must be considered. This combination is not suitable for:
Patients with type 1 diabetes or diabetic ketoacidosis
Those with severe renal impairment (eGFR <30 mL/min/1.73m² for metformin)
Pregnant or breastfeeding women
Those with a history of pancreatitis (relative contraindication for Wegovy)
A personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 is listed as a precaution in the UK SmPC for Wegovy, rather than a formal contraindication.
Age, frailty, and individual treatment goals should also inform decision-making, with less stringent glycaemic targets often appropriate for older adults or those with limited life expectancy.
Professional medical guidance is essential before starting, combining, or adjusting any diabetes or weight management medications. Self-medicating or making changes without supervision can lead to adverse outcomes and suboptimal disease control.
When to contact your GP or diabetes specialist:
You are currently taking metformin and wish to discuss additional weight management options
Your blood glucose control remains inadequate despite metformin therapy
You experience persistent or severe side effects from either medication
You develop symptoms such as persistent nausea, vomiting, abdominal pain (especially if severe or radiating to the back, which could indicate pancreatitis), or unexplained weight loss
You notice changes in vision, particularly if you have pre-existing diabetic retinopathy
You have concerns about drug interactions with other medications you are taking
Your circumstances change (e.g., pregnancy, kidney problems, or new medical conditions)
What to expect during your consultation:
Your healthcare provider will conduct a comprehensive assessment including review of your medical history, current medications, kidney function tests, HbA1c levels, BMI, and cardiovascular risk factors. They will discuss your treatment goals, lifestyle factors, and any barriers to medication adherence. If the combination is deemed appropriate, they will provide guidance on dosing schedules, titration plans, and monitoring requirements.
For Wegovy in the UK NHS, your GP would typically need to refer you to a specialist tier 3 weight management service, as per NICE TA875 guidance.
Ongoing monitoring is crucial when taking both medications. This typically includes:
Regular HbA1c testing (every 3–6 months)
Periodic kidney function assessment
Blood pressure and lipid monitoring
Weight and BMI tracking
Assessment for side effects and treatment response
Vitamin B12 levels with long-term metformin use
Eye examinations, particularly if you have diabetic retinopathy
Patient responsibilities include adhering to prescribed doses, attending monitoring appointments, reporting side effects promptly, and maintaining lifestyle modifications including healthy eating and physical activity. Remember that medications are most effective when combined with sustainable lifestyle changes.
Your healthcare team—including your GP, practice nurse, diabetes specialist nurse, and dietitian—are valuable resources for ongoing support and guidance throughout your treatment journey.
Yes, metformin and Wegovy can be safely combined under medical supervision. Clinical trials have included participants taking both medications, and they work through complementary mechanisms without significant drug interactions, though gastrointestinal side effects may be more pronounced.
According to NICE TA875, NHS access to Wegovy is restricted to specialist weight management services, typically for adults with BMI ≥35 kg/m² and at least one weight-related comorbidity (with adjusted thresholds for certain ethnic groups). Treatment is usually limited to a maximum of 2 years.
The most common side effects are gastrointestinal symptoms including nausea, diarrhoea, vomiting, and abdominal discomfort, which may be additive when both medications are used together. Gradual dose titration and taking metformin with meals can help minimise these effects.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.