
Many people in the UK with high cholesterol wonder whether weight loss injections are safe and appropriate for them. Glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda) are increasingly prescribed for weight management, often in patients who also have elevated cholesterol levels. High cholesterol, or hypercholesterolaemia, frequently coexists with obesity, creating a complex metabolic picture. Understanding the safety, interactions, and benefits of using weight loss injections alongside cholesterol management is essential for informed decision-making. This article explores the evidence, safety considerations, and monitoring requirements for patients considering these treatments whilst managing high cholesterol.
Quick Answer: Yes, weight loss injections such as semaglutide and liraglutide can generally be taken safely by patients with high cholesterol, and may even improve lipid profiles alongside weight reduction.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWeight loss injections, particularly glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have become increasingly prescribed for weight management in the UK. These prescription-only medications work by mimicking natural hormones that regulate appetite and blood glucose levels, leading to reduced food intake and subsequent weight loss. While the MHRA has approved these treatments for adults with a body mass index (BMI) of 30 kg/m² or above, or 27 kg/m² with weight-related comorbidities, it's important to note that NICE guidance (TA875) specifies narrower criteria for NHS access, particularly for semaglutide, which is typically only available through specialist weight management services.
High cholesterol, medically termed hypercholesterolaemia, is a common condition affecting millions of people in the UK. It occurs when there are elevated levels of lipids in the blood, particularly low-density lipoprotein (LDL) cholesterol, which can contribute to cardiovascular disease. Many individuals with obesity also have dyslipidaemia, creating a complex metabolic picture that requires careful management.
The relationship between obesity and high cholesterol is well-established, with excess weight often contributing to unfavourable lipid profiles. This creates a clinical scenario where patients may benefit from both weight reduction and cholesterol management. Understanding whether weight loss injections can be safely used alongside high cholesterol—or whilst taking cholesterol-lowering medications—is therefore a relevant question for many patients and healthcare professionals. It's important to emphasise that GLP-1 receptor agonists are not licensed specifically as lipid-lowering therapies, though they may have beneficial effects on cholesterol as part of their overall metabolic impact.
Key considerations include:
The safety profile of weight loss injections in patients with dyslipidaemia
Potential interactions with lipid-lowering medications
The impact of weight loss itself on cholesterol levels
Individual cardiovascular risk assessment
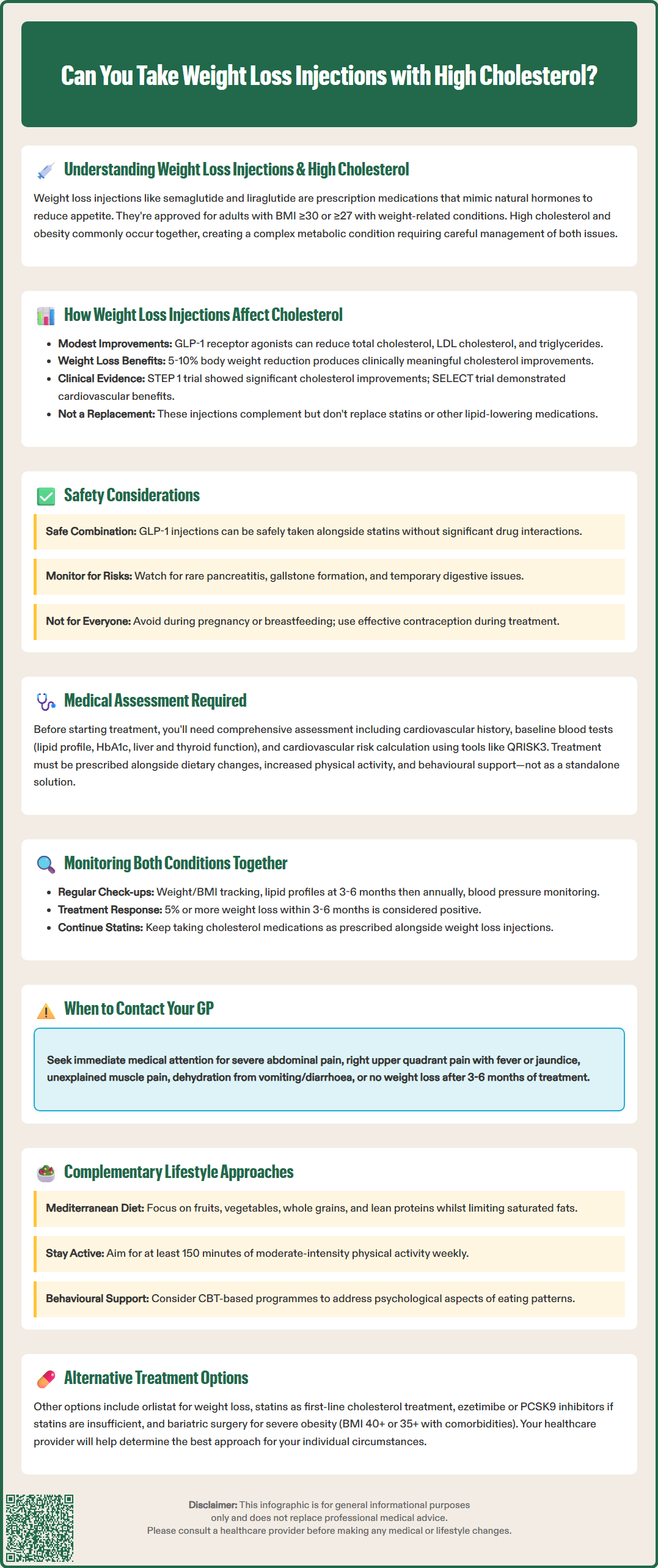
Clinical evidence suggests that GLP-1 receptor agonists may have beneficial effects on lipid profiles beyond their primary weight loss action. Research trials, including those supporting NICE guidance, have demonstrated that these medications may lead to modest improvements in cholesterol levels, particularly reductions in total cholesterol, LDL cholesterol, and triglycerides. These effects appear to result from both the direct pharmacological action of the medication and the indirect benefits of weight loss itself.
The mechanism by which GLP-1 receptor agonists influence lipid metabolism is likely multifaceted, though not fully established. These medications are thought to improve insulin sensitivity and reduce hepatic glucose production, which may indirectly affect lipid metabolism. Additionally, weight loss achieved through any means typically results in improved lipid profiles, with studies showing that a 5-10% reduction in body weight can lead to clinically meaningful improvements in cholesterol levels.
Semaglutide, one of the most widely prescribed weight loss injections, has been studied extensively in clinical trials. The STEP (Semaglutide Treatment Effect in People with obesity) trials, particularly STEP 1, demonstrated not only significant weight loss but also improvements in cardiometabolic risk factors, including lipid parameters. Participants experienced average reductions in total cholesterol and LDL cholesterol, alongside improvements in blood pressure and glycaemic control. More recently, the SELECT trial has provided evidence for cardiovascular outcome benefits in people with established cardiovascular disease.
It is important to note that whilst these improvements are encouraging, weight loss injections are not primarily prescribed as lipid-lowering agents. Patients with high cholesterol typically require specific lipid-modifying therapy, most commonly statins, as recommended by NICE guidelines (NG238). The lipid benefits of GLP-1 receptor agonists should be viewed as complementary rather than alternative to established cholesterol management strategies.
For most patients, having high cholesterol does not preclude the use of weight loss injections. In fact, the presence of dyslipidaemia alongside obesity may strengthen the clinical indication for these treatments, as both conditions contribute to cardiovascular risk. The MHRA-approved product information for semaglutide and liraglutide does not list high cholesterol as a contraindication, and these medications have been safely used in clinical trials involving participants with various cardiovascular risk factors.
Important safety considerations include:
Cardiovascular history: Patients with established cardiovascular disease require careful assessment, though recent evidence suggests GLP-1 receptor agonists may offer cardiovascular benefits
Medication interactions: No clinically significant interactions are expected between GLP-1 receptor agonists and statins or other lipid-lowering medications, though delayed gastric emptying could theoretically affect absorption of oral medications
Pancreatitis risk: Whilst rare, acute pancreatitis has been reported with GLP-1 receptor agonists; patients with hypertriglyceridaemia (very high triglycerides) may have an elevated baseline risk
Gallbladder disease: GLP-1 receptor agonists are associated with increased risk of gallstones and cholecystitis; patients should seek medical attention for right upper quadrant pain, fever, or jaundice
Gastrointestinal effects: Common side effects include nausea, vomiting, and diarrhoea, which typically diminish over time
Pregnancy and breastfeeding: These medications are not recommended during pregnancy or breastfeeding; effective contraception should be used during treatment, and preconception planning is advised
Hypoglycaemia risk: Patients also taking insulin or sulfonylureas may have an increased risk of low blood glucose and may need dose adjustments of these medications
Patients taking both weight loss injections and statins should be aware that the gastrointestinal side effects of GLP-1 receptor agonists are unrelated to statin therapy and do not indicate an interaction. However, if severe gastrointestinal symptoms occur, this may affect the absorption of oral medications, and patients should consult their GP or prescriber.
Certain conditions require additional caution. Patients with a history of pancreatitis, gallbladder disease, severe gastrointestinal disease, or diabetic retinopathy (for those with diabetes) need individualised risk-benefit assessment. Additionally, those with familial hypercholesterolaemia or very high cardiovascular risk require specialist input to ensure comprehensive management of all risk factors.
Before initiating weight loss injections, a comprehensive medical assessment is essential, particularly for patients with high cholesterol or other cardiovascular risk factors. NICE recommends that weight management medications should only be prescribed as part of a holistic approach that includes dietary modification, increased physical activity, and behavioural support.
The pre-treatment assessment should include a detailed medical history covering cardiovascular disease, diabetes, thyroid disorders, gallbladder disease, pancreatitis, and previous weight loss attempts. A family history of premature cardiovascular disease or familial hypercholesterolaemia is particularly relevant. Healthcare professionals should document current medications, as this helps identify potential issues and ensures appropriate monitoring. For women of childbearing potential, pregnancy testing and contraception counselling are important considerations.
Essential baseline investigations typically include:
Lipid profile: Total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides to establish baseline values
HbA1c or fasting glucose: To screen for diabetes or prediabetes
Liver function tests: As baseline measurement, particularly if considering long-term treatment
Thyroid function tests: To exclude thyroid disorders that may affect weight
Blood pressure measurement: To assess overall cardiovascular risk
Renal function: Particularly important for patients on multiple medications
Pregnancy test: Where appropriate, before starting treatment
Cardiovascular risk assessment using tools such as QRISK3 helps determine the overall 10-year risk of cardiovascular disease. This calculation incorporates cholesterol levels, blood pressure, smoking status, and other factors to guide treatment decisions. Patients with high cardiovascular risk may benefit most from weight loss interventions, but they also require optimisation of all modifiable risk factors, including cholesterol management with statins where indicated.
The assessment should also explore realistic expectations, potential side effects, and the commitment required for successful treatment. Weight loss injections are not a quick fix but rather a tool to support sustained lifestyle changes. Patients should understand that treatment typically continues for a defined period (up to 2 years for semaglutide under NICE guidance), with specific stopping rules based on weight loss response. For liraglutide, treatment should be discontinued if at least 5% weight loss has not been achieved after 12 weeks at the maintenance dose.
Effective management of patients taking weight loss injections whilst having high cholesterol requires coordinated monitoring of both conditions. NICE guidance recommends reviewing patients at regular intervals to assess treatment response, tolerability, and the need for dose adjustments or additional interventions.
During the initial months of treatment with GLP-1 receptor agonists, patients typically attend regular reviews as per local specialist service protocol to monitor weight loss progress and manage side effects. The dose is usually titrated gradually to minimise gastrointestinal symptoms whilst achieving therapeutic effect. A weight loss of 5% or more within 3-6 months is generally considered a positive response, though individual targets should be personalised.
Ongoing monitoring should include:
Weight and BMI tracking: Regular measurements to assess treatment efficacy
Lipid profile reassessment: Typically at 3-6 months and then annually, or as clinically indicated
Blood pressure monitoring: As weight loss often improves hypertension
HbA1c monitoring: For patients with diabetes or prediabetes
Assessment of side effects: Particularly gastrointestinal symptoms, which may require dose adjustment
Review of cardiovascular risk factors: Holistic assessment of smoking, diet, and physical activity
For patients taking statins alongside weight loss injections, it is important to continue lipid-lowering therapy as prescribed. Weight loss alone may not achieve target cholesterol levels, particularly in those with significantly elevated LDL cholesterol or high cardiovascular risk. Some patients may find that as they lose weight and improve their metabolic health, statin doses can be reviewed, though any changes should be made under medical supervision.
When to contact your GP:
Severe or persistent abdominal pain (potential pancreatitis)
Right upper quadrant pain, fever, or jaundice (potential gallbladder disease)
Unexplained muscle pain or weakness (if taking statins)
Signs of dehydration from vomiting or diarrhoea
No weight loss after 3-6 months of treatment
Any concerns about medication side effects
Regular follow-up allows healthcare professionals to optimise both weight management and cholesterol control, adjusting treatment strategies based on individual response and emerging evidence. Patients should be encouraged to report any suspected side effects via the MHRA Yellow Card scheme.
Whilst weight loss injections can be effective for appropriate patients, they represent just one component of comprehensive weight and cholesterol management. NICE emphasises that pharmacological interventions should complement, not replace, lifestyle modifications that form the foundation of treatment for both obesity and dyslipidaemia.
Dietary approaches are particularly important for managing both conditions simultaneously. A diet rich in fruits, vegetables, whole grains, and lean proteins, whilst limiting saturated fats, trans fats, and refined carbohydrates, benefits both weight and lipid profiles. The Mediterranean diet pattern has strong evidence for cardiovascular health and can support sustainable weight loss. Increasing soluble fibre intake through oats, beans, and vegetables can help reduce LDL cholesterol naturally. Patients should consider referral to a registered dietitian for personalised nutritional advice.
Physical activity plays a crucial role in both weight management and improving cholesterol levels. The UK Chief Medical Officers recommend adults aim for at least 150 minutes of moderate-intensity activity weekly. Exercise raises HDL ("good") cholesterol, lowers triglycerides, and contributes to weight loss and maintenance. Activities need not be strenuous; brisk walking, swimming, or cycling can all provide benefits. Patients with cardiovascular risk factors should discuss appropriate exercise levels with their healthcare provider.
Alternative pharmacological options for weight management include orlistat, which works by reducing fat absorption from the diet. Whilst it has a different mechanism to GLP-1 receptor agonists, it can be used in patients with high cholesterol and may be appropriate for those who cannot tolerate or access injectable treatments. NICE recommends reviewing orlistat treatment at 12 weeks and discontinuing if inadequate weight loss has been achieved. For cholesterol management, statins remain the first-line medication, with alternatives such as ezetimibe or PCSK9 inhibitors available for patients who cannot achieve targets with statins alone.
Behavioural support programmes, whether through NHS services, commercial providers, or digital platforms, enhance the effectiveness of any weight loss intervention. These programmes address the psychological and behavioural aspects of eating and activity patterns, supporting long-term change. Cognitive behavioural therapy techniques can help patients develop healthier relationships with food and overcome barriers to lifestyle change.
For some patients with severe obesity and multiple comorbidities, bariatric surgery may be considered. NICE recommends this for adults with a BMI of 40 kg/m² or above, or 35 kg/m² with significant comorbidities. For people with recent-onset type 2 diabetes, bariatric surgery may be considered at a lower BMI threshold of 30-34.9 kg/m². Bariatric procedures typically result in substantial improvements in both weight and metabolic parameters, including dramatic improvements in lipid profiles.
Ultimately, the most effective approach combines evidence-based medical treatments with sustained lifestyle modifications, tailored to individual circumstances, preferences, and clinical needs. Regular review and adjustment of the treatment plan ensures optimal management of both weight and cardiovascular risk factors over time.
No, there are no significant pharmacological interactions between GLP-1 receptor agonists such as semaglutide or liraglutide and statins. Patients can safely take both medications together under medical supervision.
Weight loss injections may lead to modest improvements in cholesterol levels, particularly reductions in total cholesterol, LDL cholesterol, and triglycerides, primarily through weight loss itself. However, they are not prescribed as primary lipid-lowering agents and should complement established cholesterol management strategies.
Patients require baseline lipid profiles, cardiovascular risk assessment, and regular monitoring including weight tracking, lipid profile reassessment at 3-6 months and annually, blood pressure monitoring, and assessment of side effects throughout treatment.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.