Can you use weight loss injections after gastric sleeve surgery? Many patients who undergo sleeve gastrectomy experience excellent initial results, yet some face weight regain or inadequate weight loss over time. GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda) are increasingly being considered as adjunctive therapy in post-bariatric patients. Whilst this represents off-label use requiring specialist supervision, emerging evidence suggests these medications may offer additional support for carefully selected individuals. Understanding the benefits, risks, and clinical considerations is essential for anyone contemplating this combined approach to weight management.
Quick Answer: Yes, weight loss injections such as GLP-1 receptor agonists can be used after gastric sleeve surgery, though this is off-label and requires specialist bariatric team supervision.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGastric sleeve surgery, also known as sleeve gastrectomy, is a bariatric procedure that removes approximately 75–80% of the stomach, leaving a narrow, tube-shaped stomach roughly the size of a banana. This restrictive surgery reduces stomach capacity, limits food intake, and alters gut hormones that regulate appetite and metabolism. The procedure is typically offered to individuals with a body mass index (BMI) of 40 kg/m² or above, or 35 kg/m² and above with obesity-related health conditions such as type 2 diabetes or hypertension, in line with NICE guidance (CG189). Lower BMI thresholds may apply for certain ethnic groups.
Weight loss injections refer primarily to glucagon-like peptide-1 (GLP-1) receptor agonists, such as semaglutide (Wegovy) and liraglutide (Saxenda). These medications mimic the action of the naturally occurring hormone GLP-1, which is released from the gut after eating. They work by:
Slowing gastric emptying, which prolongs feelings of fullness
Reducing appetite through effects on brain centres that regulate hunger
Improving insulin secretion and glucose metabolism
Potentially reducing food intake and affecting eating behaviours
These injections are administered subcutaneously, typically once weekly (semaglutide) or once daily (liraglutide), and have been approved by the MHRA for weight management in adults with a BMI ≥30 kg/m², or ≥27 kg/m² with weight-related comorbidities, as an adjunct to reduced-calorie diet and increased physical activity. Tirzepatide is another injectable medication now licensed in the UK for weight management.
NHS access to these medications follows NICE technology appraisals and local commissioning policies, typically requiring specialist weight management service oversight. Both gastric sleeve surgery and weight loss injections aim to achieve sustained weight reduction and improve metabolic health, though they operate through different mechanisms. Understanding how these approaches work individually is essential before considering their combined use in post-bariatric patients who experience weight regain or inadequate weight loss.
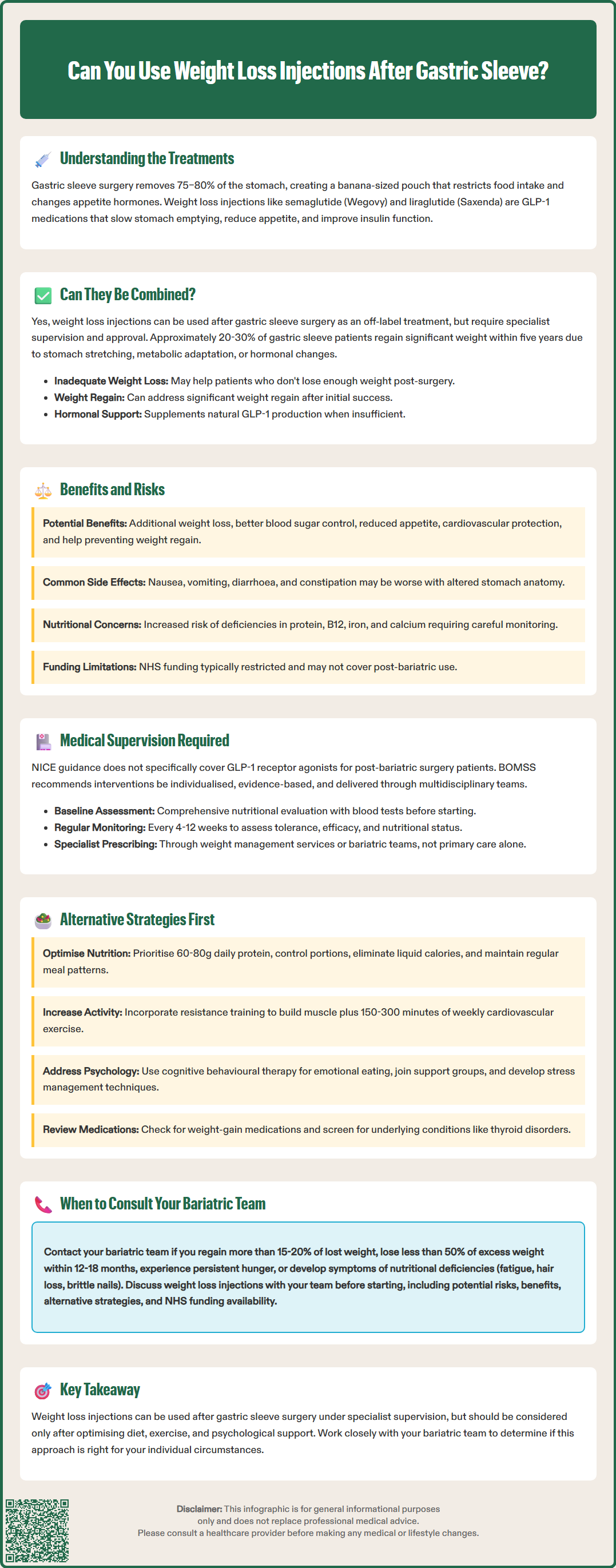
Yes, weight loss injections can be used after gastric sleeve surgery, and this approach is increasingly being considered in clinical practice for specific patient groups. There is no absolute contraindication to using GLP-1 receptor agonists following bariatric surgery, and emerging evidence suggests they may offer benefits for certain post-operative patients.
Patients who have undergone gastric sleeve surgery sometimes experience weight regain after the initial post-operative period, typically occurring 18–24 months after surgery. Studies indicate that approximately 20–30% of bariatric surgery patients regain a significant portion of their lost weight within five years. This can occur due to various factors including:
Stomach stretching over time, allowing increased food intake
Metabolic adaptation, where the body adjusts to lower calorie intake
Behavioural factors, such as return to previous eating patterns
Hormonal changes that may affect appetite regulation
For patients experiencing inadequate weight loss or significant weight regain after gastric sleeve, GLP-1 receptor agonists may provide additional support. Observational studies suggest these medications can produce additional weight loss in post-bariatric patients, with some cohorts showing approximately 5–10% further body weight reduction, though results vary considerably between individuals.
Interestingly, gastric sleeve surgery itself increases natural GLP-1 production, which contributes to its weight loss effects. However, some patients may not experience sufficient endogenous GLP-1 elevation. Supplementing with pharmaceutical GLP-1 analogues may augment these hormonal effects, potentially providing renewed appetite control and metabolic benefits, though the precise mechanisms in post-bariatric patients are not fully established.
Importantly, prescribing must still meet licensed indications and NICE/local commissioning criteria; availability after surgery varies by region and is not automatically funded. The decision to use these injections post-operatively should always be made in consultation with a bariatric team.
Potential benefits of using GLP-1 receptor agonists after gastric sleeve surgery include:
Enhanced weight loss: Observational studies suggest post-bariatric patients using GLP-1 receptor agonists may achieve additional weight reduction, typically around 5–10% of body weight, though individual responses vary considerably
Improved glycaemic control: Particularly beneficial for patients with type 2 diabetes or prediabetes, as GLP-1 agonists enhance insulin secretion and reduce blood glucose levels
Reduced appetite: These medications can help patients who struggle with persistent hunger despite surgical intervention
Cardiovascular benefits: Semaglutide has demonstrated cardiovascular risk reduction in people with established cardiovascular disease, which may benefit eligible post-bariatric patients with this specific risk profile
Maintenance of weight loss: May help prevent weight regain during the critical maintenance phase
Potential risks and considerations include:
Gastrointestinal side effects: Nausea, vomiting, diarrhoea, and constipation are common, particularly during dose escalation. These effects may be more pronounced in patients with altered gastric anatomy
Pancreatitis risk: Patients should be informed about symptoms of acute pancreatitis (severe abdominal pain, sometimes radiating to the back, with vomiting) and seek immediate medical attention if these occur
Gallbladder disease: Increased risk of gallstones and gallbladder-related problems, particularly with substantial weight loss
Dehydration and acute kidney injury: Reduced fluid intake combined with gastrointestinal side effects may increase risk of dehydration
Nutritional concerns: The combination of reduced stomach capacity and appetite suppression may increase the risk of nutritional deficiencies, particularly protein, vitamin B12, iron, and calcium
Hypoglycaemia risk: Especially in patients taking diabetes medications, careful monitoring and dose adjustment may be necessary
Diabetic retinopathy: Patients with diabetes should have appropriate eye screening, as rapid improvement in glucose control may temporarily worsen retinopathy
Medication absorption: GLP-1 receptor agonists may affect absorption of oral medications due to delayed gastric emptying
Pregnancy and contraception: These medications are not recommended during pregnancy or breastfeeding; effective contraception is advised for women of childbearing potential
Cost and access: NHS funding typically follows NICE technology appraisal criteria with specialist oversight and is usually limited to a maximum of 2 years
Patients must be carefully selected and monitored to maximise benefits whilst minimising potential adverse effects. Regular nutritional assessment and supplementation are essential components of safe combined therapy. Suspected side effects should be reported via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Currently, NICE guidance does not specifically address the use of GLP-1 receptor agonists in post-bariatric surgery patients, as this represents an evolving area of clinical practice. However, NICE technology appraisals for weight management medications provide the framework for NHS access:
Semaglutide 2.4 mg (Wegovy) – NICE TA875: For adults with BMI ≥35 kg/m² and at least one weight-related comorbidity, or ≥30 kg/m² with specific risk factors, in specialist weight management services, typically for up to 2 years
Liraglutide 3.0 mg (Saxenda) – NICE TA664: Similar criteria with specialist oversight and duration limits
Tirzepatide – Subject to current NICE guidance for weight management
The British Obesity and Metabolic Surgery Society (BOMSS) recommends that any pharmacological intervention after bariatric surgery should be:
Individualised based on patient circumstances, weight trajectory, and comorbidities
Evidence-based where possible, acknowledging the limited but growing research base
Delivered within a multidisciplinary framework involving bariatric surgeons, dietitians, psychologists, and specialist physicians
Accompanied by lifestyle modification support, including dietary counselling and physical activity guidance
Medical supervision requirements for post-bariatric patients using weight loss injections include:
Baseline assessment: Comprehensive evaluation of nutritional status, including blood tests for vitamins, minerals, protein levels, renal function, and HbA1c/glucose
Regular monitoring: Follow-up appointments every 4–12 weeks initially to assess tolerance, efficacy, and side effects
Nutritional surveillance: Ongoing monitoring of protein intake, hydration status, and micronutrient levels with appropriate supplementation
Medication review: Assessment of concurrent medications, particularly diabetes treatments that may require adjustment
Pregnancy status: Confirmation of effective contraception in women of childbearing potential
Diabetic eye screening: For patients with diabetes, particularly if rapid improvement in glucose control occurs
Psychological support: Evaluation of eating behaviours, body image concerns, and mental health
Prescribing should typically occur through specialist weight management services or bariatric teams rather than primary care alone, given the complexity of post-surgical patients. Documentation of informed consent, including discussion of the evidence base and commissioning context, is essential. Patients should be advised that NHS-funded treatment duration is typically limited to a maximum of 2 years, as per NICE guidance, and that discontinuation often results in weight regain.
Before considering weight loss injections, patients experiencing suboptimal results after gastric sleeve surgery should explore alternative evidence-based strategies:
Dietary optimisation remains fundamental:
Protein prioritisation: Consuming adequate protein (commonly ≥60g daily, individualised by a bariatric dietitian) to preserve lean muscle mass and promote satiety
Portion control: Using smaller plates and mindful eating techniques to prevent stomach stretching
Avoiding liquid calories: Eliminating sugary drinks, alcohol, and high-calorie smoothies that can bypass restriction
Regular meal patterns: Eating three small meals with planned snacks to maintain stable blood glucose and prevent grazing
Nutritional counselling: Working with a specialist bariatric dietitian to identify and address dietary challenges
Lifelong supplementation: Following BOMSS guidance on multivitamin/mineral, vitamin D/calcium, and B12 supplementation with periodic blood monitoring
Physical activity enhancement:
Resistance training: Building muscle mass to increase metabolic rate and improve body composition
Cardiovascular exercise: Aiming for 150–300 minutes of moderate-intensity activity weekly, as recommended by UK Chief Medical Officers
Behavioural activation: Increasing daily movement through lifestyle changes such as walking, gardening, or active commuting
Psychological interventions:
Cognitive behavioural therapy (CBT): Addressing emotional eating, body image concerns, and maladaptive eating patterns
Support groups: Participating in bariatric patient communities for peer support and accountability
Stress management: Developing healthy coping strategies to prevent stress-related eating
Medical review:
Medication assessment: Identifying drugs that may promote weight gain (certain antidepressants, antipsychotics, corticosteroids)
Endocrine evaluation: Screening for hypothyroidism, Cushing's syndrome, or polycystic ovary syndrome
Sleep assessment: Addressing obstructive sleep apnoea, which can impair weight loss
Anatomical assessment: Evaluating for sleeve dilation, reflux, or other structural changes that might warrant endoscopic or surgical revision
These foundational strategies should be optimised before adding pharmacological interventions, as they address modifiable factors that commonly contribute to post-bariatric weight regain.
Patients who have undergone gastric sleeve surgery should maintain regular long-term follow-up with their bariatric team, as recommended by NICE and BOMSS guidelines. However, specific circumstances warrant prompt consultation:
Contact your bariatric team if you experience:
Significant weight regain: Regaining more than 15–20% of lost weight or returning to within 5% of pre-operative weight (follow your team's specific guidance)
Inadequate initial weight loss: Losing less than 50% of excess weight within 12–18 months post-operatively
Persistent hunger: Experiencing constant or severe hunger despite appropriate portion sizes
Loss of restriction: Ability to consume significantly larger portions than in the early post-operative period
Nutritional deficiencies: Symptoms such as fatigue, hair loss, brittle nails, or neurological changes suggesting vitamin deficiencies
Gastrointestinal symptoms: New or worsening nausea, vomiting, reflux, or abdominal pain
Psychological difficulties: Depression, anxiety, eating disorders, or body image distress affecting quality of life
Comorbidity recurrence: Return of obesity-related conditions such as type 2 diabetes, hypertension, or sleep apnoea
Before starting weight loss injections, discuss with your bariatric team:
Your weight loss trajectory and realistic expectations
Potential benefits and risks specific to your medical history
Alternative strategies that may be appropriate
Funding and access pathways, as NHS provision varies by region
Monitoring requirements and long-term treatment plans
Emergency situations requiring immediate medical attention include:
Severe, persistent vomiting or inability to tolerate fluids
Signs of dehydration (dark urine, dizziness, rapid heartbeat)
Severe abdominal pain or suspected surgical complications
Symptoms of acute pancreatitis (severe epigastric pain radiating to the back, with vomiting)
Signs of gallbladder disease (right upper quadrant pain, fever, jaundice)
Symptoms of hypoglycaemia (confusion, sweating, tremor) if using diabetes medications
Your bariatric team can provide personalised guidance on whether weight loss injections are appropriate for your individual circumstances and can coordinate comprehensive care to support your long-term success. If you experience suspected side effects from weight loss injections, report them via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
There is no fixed timeframe, but weight loss injections are typically considered for patients who experience weight regain or inadequate weight loss 18–24 months post-operatively. Your bariatric team will assess your individual circumstances, weight trajectory, and nutritional status before recommending treatment.
NHS funding for GLP-1 receptor agonists after bariatric surgery is limited and varies by region, as this represents off-label use not specifically covered by NICE guidance. Individual funding requests may be considered on a case-by-case basis through specialist weight management services.
The main risks include gastrointestinal side effects (nausea, vomiting, diarrhoea), increased risk of nutritional deficiencies due to combined appetite suppression and reduced stomach capacity, and potential hypoglycaemia in patients taking certain diabetes medications. Regular monitoring by a bariatric team is essential to minimise these risks.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.