Diabetic retinopathy remains a leading cause of vision impairment amongst working-age adults in the UK, developing when persistently elevated blood glucose damages the delicate blood vessels of the retina. Mounjaro (tirzepatide), a dual GIP and GLP-1 receptor agonist, offers substantial glycaemic improvements for people with type 2 diabetes. Whilst improved glucose control reduces long-term retinopathy risk, rapid HbA1c reductions can occasionally cause temporary worsening of pre-existing eye disease. Understanding this relationship, maintaining regular NHS diabetic eye screening, and recognising warning signs are essential for preserving vision whilst benefiting from effective diabetes treatment.
Quick Answer: Mounjaro (tirzepatide) does not directly cause diabetic retinopathy, but rapid improvements in blood glucose control can temporarily worsen pre-existing retinopathy in some individuals.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereDiabetic retinopathy is a serious complication of diabetes that affects the blood vessels in the retina—the light-sensitive tissue at the back of the eye. It remains one of the leading causes of vision impairment in working-age adults in the UK. The condition develops when persistently elevated blood glucose levels damage the tiny blood vessels that nourish the retina, leading to leakage, swelling, and the formation of abnormal new blood vessels.
The progression of diabetic retinopathy typically occurs in stages. Non-proliferative diabetic retinopathy (NPDR) represents the early phase, characterised by microaneurysms, haemorrhages, and exudates within the retina. Many individuals experience no symptoms during this stage. As the condition advances to proliferative diabetic retinopathy (PDR), new fragile blood vessels grow on the retinal surface—a process called neovascularisation. These vessels are prone to bleeding into the vitreous cavity, causing sudden vision loss. Additionally, diabetic macular oedema (DMO) can occur at any stage when fluid accumulates in the macula, the central part of the retina responsible for sharp vision.
Several risk factors accelerate the development and progression of diabetic retinopathy:
Duration of diabetes: The longer someone has diabetes, the higher their risk
Poor glycaemic control: HbA1c levels consistently above target increase vascular damage
Hypertension: Elevated blood pressure compounds retinal vessel stress
Dyslipidaemia: Abnormal cholesterol levels contribute to vascular complications
Pregnancy: Gestational changes can accelerate retinopathy progression
Diabetic nephropathy: Kidney disease often correlates with retinopathy progression
Smoking: Independently worsens retinopathy risk and progression
Regular screening through the NHS Diabetic Eye Screening Programme is essential for early detection, as treatment is most effective when initiated before significant vision loss occurs. Most people with diabetes aged 12 years and over are invited for annual digital retinal photography, though some low-risk individuals may now be offered screening at 2-year intervals following NHS programme updates.
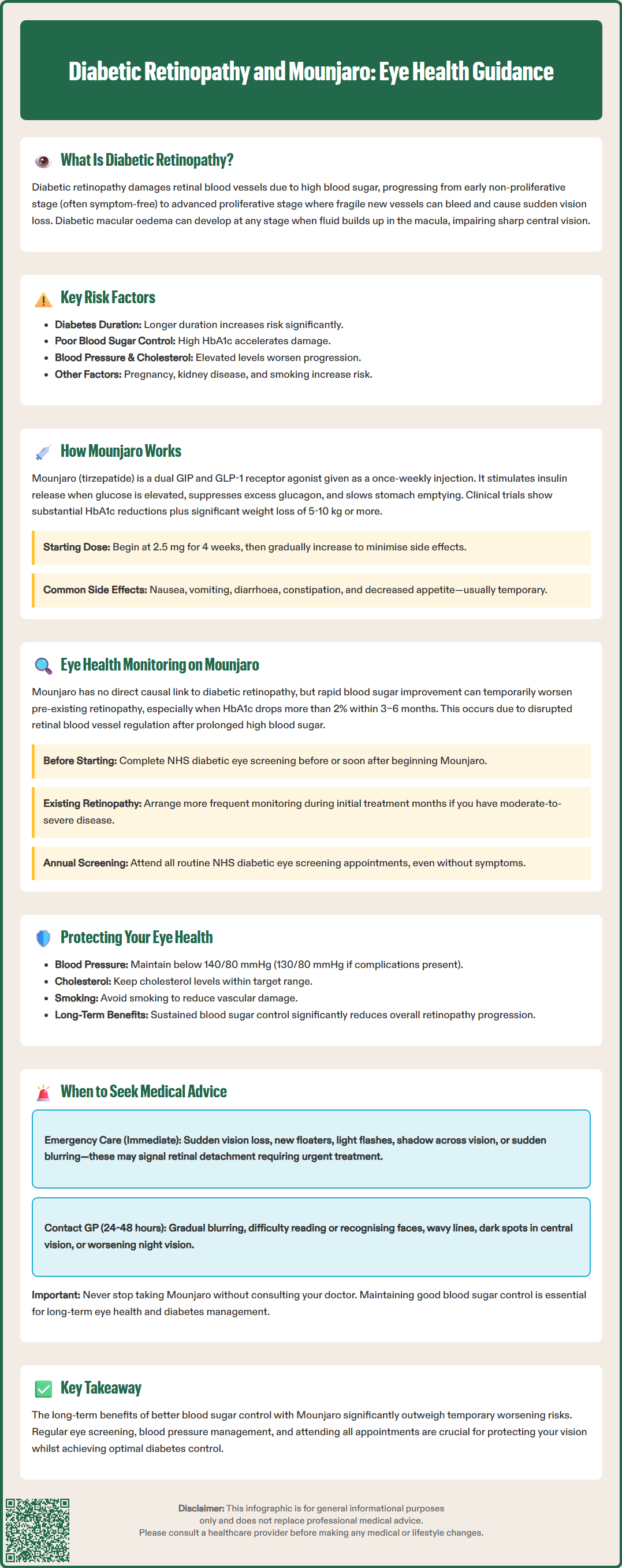
Mounjaro (tirzepatide) represents a novel class of medication for type 2 diabetes management, approved by the MHRA in the UK. It is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist. According to its Summary of Product Characteristics (SmPC), tirzepatide is licensed as an adjunct to diet and exercise to improve glycaemic control in adults with type 2 diabetes, either as monotherapy when metformin is inappropriate, or in combination with other diabetes medications.
The pharmacological action of tirzepatide involves several complementary mechanisms. By activating GLP-1 receptors, it stimulates glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriate glucagon release, and slows gastric emptying—all of which contribute to improved postprandial glucose control. The additional GIP receptor activation appears to augment insulin secretion further and may influence fat metabolism. Importantly, the glucose-dependent nature of insulin stimulation means the risk of hypoglycaemia is relatively low when tirzepatide is used alone, though the risk increases significantly when used with insulin or sulphonylureas.
Mounjaro is administered as a once-weekly subcutaneous injection, with doses ranging from 2.5 mg to 15 mg. Treatment begins with 2.5 mg for 4 weeks as an initiation dose to improve gastrointestinal tolerability; this starting dose is not intended for glycaemic control. Gradual titration then occurs every four weeks to minimise gastrointestinal side effects and optimise glycaemic response. Clinical trials (SURPASS programme) have demonstrated substantial HbA1c reductions alongside significant weight loss, averaging 5–10 kg or more depending on the dose.
Common adverse effects include:
Nausea and vomiting (usually transient)
Diarrhoea or constipation
Decreased appetite
Abdominal discomfort
Injection site reactions
Serious but rare adverse effects include pancreatitis, gallbladder disease, and acute kidney injury secondary to dehydration. Patients should be counselled about recognising symptoms of these conditions and seeking prompt medical attention if they occur.
Important precautions include:
Dose reduction of insulin or sulphonylureas may be needed when adding tirzepatide to prevent hypoglycaemia
Tirzepatide may reduce the absorption of oral medications including oral contraceptives; additional contraception is advised during initiation and dose escalation
Tirzepatide should not be used during pregnancy or breastfeeding and should be discontinued at least 2 months before a planned pregnancy
Suspected adverse reactions should be reported via the MHRA Yellow Card Scheme.
The relationship between GLP-1 receptor agonists and diabetic retinopathy has received considerable attention following observations in clinical trials. The Mounjaro SmPC includes a precaution regarding diabetic retinopathy monitoring. While there is no established direct causal link between Mounjaro and the development of diabetic retinopathy, rapid improvements in glycaemic control—regardless of the method—can paradoxically lead to temporary worsening of pre-existing retinopathy. This phenomenon, termed "early worsening," has been documented with intensive insulin therapy and other glucose-lowering interventions in landmark studies such as the Diabetes Control and Complications Trial (DCCT).
The proposed mechanism involves rapid normalisation of blood glucose after prolonged hyperglycaemia, which may disrupt retinal autoregulation and exacerbate vascular permeability. This risk appears highest in individuals with:
Pre-existing moderate to severe non-proliferative or proliferative diabetic retinopathy
Very poor baseline glycaemic control (HbA1c >10%)
Rapid HbA1c reduction (>2% within 3–6 months)
Practical strategies for eye health management include ensuring patients are up to date with their NHS diabetic eye screening before initiating Mounjaro or soon after starting treatment. For those with established retinopathy, more frequent ophthalmological monitoring may be warranted during the initial months of treatment, especially if significant HbA1c reductions are anticipated.
Patients should be educated about the importance of:
Attending all scheduled NHS diabetic eye screening appointments
Maintaining optimal blood pressure control (target <140/80 mmHg, or <130/80 mmHg if kidney, eye, or cerebrovascular disease is present, as per NICE guideline NG28)
Managing cardiovascular risk factors, including lipid control
Avoiding smoking, which independently worsens retinopathy
It is crucial to emphasise that the long-term benefits of improved glycaemic control far outweigh the transient risk of early worsening. Sustained glucose control reduces the overall progression of diabetic retinopathy and other microvascular complications over time.
Patients taking Mounjaro should be vigilant about any changes in their vision and understand when urgent medical assessment is required. Whilst most individuals tolerate the medication well without ocular complications, prompt recognition of warning signs can prevent irreversible vision loss.
Seek immediate medical attention (attend A&E or contact emergency services) if you experience:
Sudden loss of vision in one or both eyes
Sudden appearance of multiple new floaters (spots or cobwebs in vision)
Flashes of light in peripheral vision
A curtain or shadow moving across your field of vision
Sudden blurring that does not improve with blinking
These symptoms may indicate vitreous haemorrhage, retinal detachment, or severe macular oedema—all of which require urgent ophthalmological assessment and potential intervention. If unsure, contact NHS 111 for urgent advice.
Contact your GP or diabetes specialist nurse within 24–48 hours if you notice:
Gradual blurring of vision that persists
Difficulty reading or recognising faces
Distorted vision (straight lines appearing wavy)
Dark or empty areas in your central vision
Worsening night vision
Your healthcare team can arrange expedited ophthalmology referral if indicated. It is important to note that some degree of blurred vision can occur temporarily when blood glucose levels change rapidly, as fluctuations affect the lens of the eye. This typically resolves as glucose levels stabilise and should not be confused with retinopathy progression.
Continue routine care by attending your diabetic eye screening appointments even if you have no symptoms—diabetic retinopathy often progresses silently in its early stages. If you have established retinopathy, your screening interval may be shortened to six months or less. Never discontinue Mounjaro without consulting your prescriber, as the benefits of sustained glycaemic control are essential for long-term eye health and overall diabetes management. Open communication with your diabetes care team ensures any concerns are addressed promptly whilst maintaining optimal therapeutic outcomes.
Mounjaro does not directly cause diabetic retinopathy. However, rapid improvements in blood glucose control with any diabetes treatment can temporarily worsen pre-existing retinopathy in some individuals, particularly those with moderate to severe disease at baseline.
Yes, you should be up to date with your NHS diabetic eye screening before starting Mounjaro or soon after initiation. If you have established retinopathy, your healthcare team may recommend more frequent ophthalmological monitoring during the initial months of treatment.
Seek immediate medical attention for sudden vision loss, multiple new floaters, flashes of light, a shadow or curtain across your vision, or sudden blurring that does not improve. These symptoms may indicate serious complications requiring urgent ophthalmological assessment.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.