Do you have to take GLP-1 for life? This is a common question for people prescribed glucagon-like peptide-1 (GLP-1) receptor agonists for type 2 diabetes or weight management. The answer depends on your individual circumstances, treatment response, and underlying condition. Whilst some patients may require long-term therapy, others can reduce or stop these medications under medical supervision, particularly if lifestyle changes are sustained. This article explores treatment duration, what happens when you stop, and alternative management strategies to help you make informed decisions with your healthcare team.
Quick Answer: GLP-1 treatment duration varies by individual—some patients require long-term therapy whilst others can reduce or stop under medical supervision, depending on treatment response and lifestyle changes.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
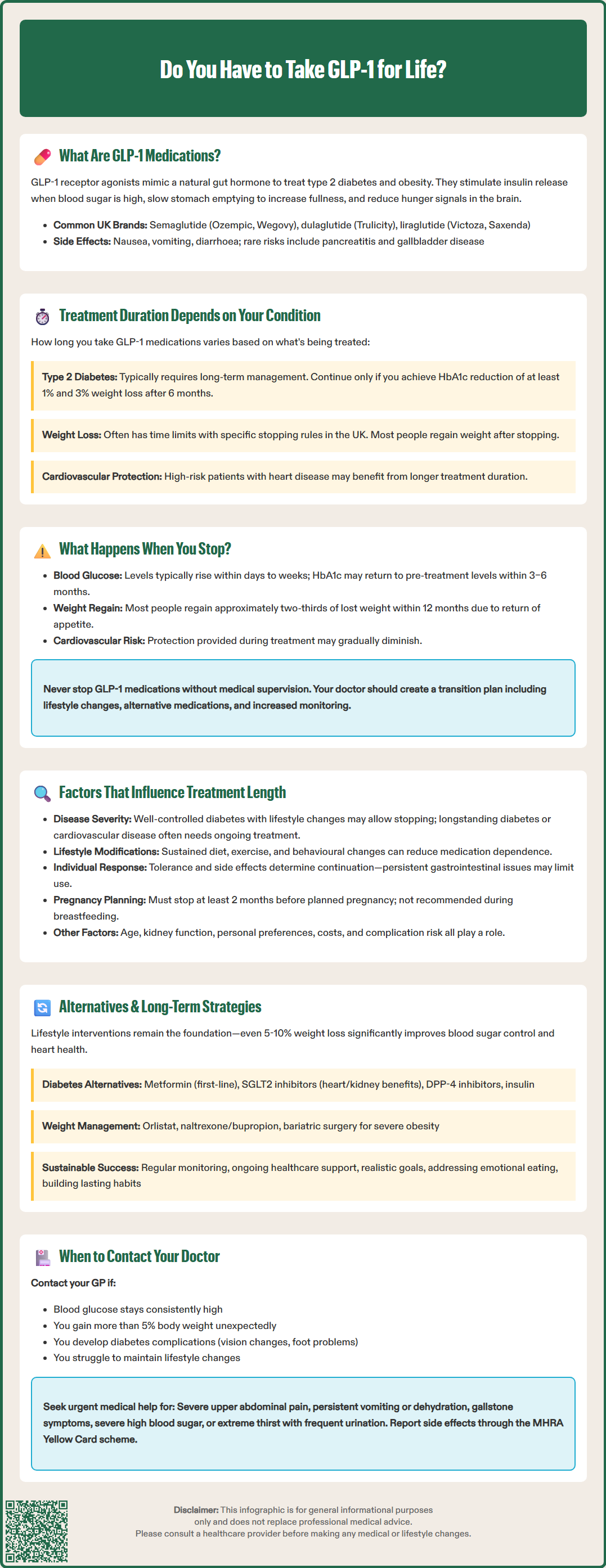
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily used to manage type 2 diabetes and, more recently, obesity. These medicines mimic the action of naturally occurring GLP-1, a hormone produced in the intestine that plays a crucial role in glucose regulation and appetite control.
The mechanism of action involves several physiological pathways. GLP-1 medications bind to GLP-1 receptors on pancreatic beta cells, stimulating insulin secretion in a glucose-dependent manner—meaning they only trigger insulin release when blood glucose levels are elevated. Simultaneously, they suppress glucagon secretion, the hormone that raises blood sugar. This dual action helps maintain more stable glycaemic control throughout the day.
Beyond glucose regulation, GLP-1 receptor agonists significantly affect appetite and satiety. They slow gastric emptying, prolonging the feeling of fullness after meals, and act on appetite centres in the brain to reduce hunger signals. This combination of effects explains why these medications are effective for both diabetes management and weight loss.
Common GLP-1 medications available in the UK include:
Semaglutide (Ozempic, Wegovy, Rybelsus [oral formulation])
Dulaglutide (Trulicity)
Liraglutide (Victoza, Saxenda)
Exenatide (Byetta, Bydureon) - availability may vary
Most GLP-1 receptor agonists are administered via subcutaneous injection, with dosing frequencies ranging from daily to once weekly, depending on the specific formulation. Oral semaglutide (Rybelsus) is the exception, taken as a daily tablet.
Importantly, these medications are not indicated for type 1 diabetes or diabetic ketoacidosis (DKA). Common side effects include gastrointestinal symptoms (nausea, vomiting, diarrhoea), while rarer risks include pancreatitis, gallbladder disease, and potential worsening of diabetic retinopathy in some patients. When used with insulin or sulfonylureas, they may increase hypoglycaemia risk.
The MHRA has approved various GLP-1 receptor agonists for different indications, with some licensed specifically for diabetes (e.g., Ozempic) and others for weight management (e.g., Wegovy, Saxenda). NICE provides guidance on their use within the NHS for both diabetes and weight management in specific patient populations.
The question of lifelong GLP-1 treatment does not have a universal answer—it depends on the underlying condition being treated and individual patient circumstances. For many people with type 2 diabetes or obesity, these are chronic conditions that may require ongoing management, but this does not automatically mean indefinite medication use.
For type 2 diabetes management, GLP-1 medications are typically considered part of a long-term treatment strategy. However, the duration of treatment varies considerably. According to NICE guidance (NG28), treatment should be reviewed at around 6 months and continued only if there is a clinically meaningful response (defined as an HbA1c reduction of at least 11 mmol/mol [1%] and weight loss of at least 3% of initial body weight). Some patients may achieve sufficient glycaemic control through lifestyle modifications and can reduce or discontinue GLP-1 therapy under medical supervision. Others with more advanced disease or multiple risk factors may benefit from continued treatment.
When prescribed for weight management, the situation is similarly nuanced but with specific NHS restrictions. Clinical trials demonstrate that most individuals regain weight after stopping GLP-1 medications, suggesting that ongoing treatment may be necessary to maintain weight loss. However, in the UK, medications like semaglutide 2.4mg (Wegovy) and liraglutide 3.0mg (Saxenda) are typically prescribed through specialist weight management services with specific stopping rules. For example, Wegovy treatment on the NHS is time-limited and should be discontinued if a 5% weight reduction is not achieved after 12 weeks on the maintenance dose.
Cardiovascular benefits have been demonstrated for specific GLP-1 medications (liraglutide, semaglutide, and dulaglutide) in defined high-risk populations. These benefits may influence treatment duration decisions for patients with established cardiovascular disease or multiple risk factors.
The decision to continue or stop GLP-1 therapy should be made collaboratively between patient and clinician, considering:
Achievement of treatment targets (HbA1c, weight loss)
Presence of side effects or tolerability issues
Individual risk factors and comorbidities
Patient preferences and quality of life
Cost-effectiveness and NHS resource allocation
Discontinuing GLP-1 receptor agonists typically leads to reversal of many therapeutic effects, though the timeline and extent vary between individuals. Understanding these changes is essential for informed decision-making about treatment duration.
Metabolic changes occur relatively quickly after cessation. The glucose-lowering effects diminish as the medication clears from the system—usually within days to weeks, depending on the specific drug's half-life. For people with type 2 diabetes, this often means blood glucose levels rise back towards pre-treatment values unless other interventions are in place. HbA1c levels typically increase over subsequent months, potentially returning to baseline within 3–6 months if no alternative management strategies are implemented.
Weight regain is one of the most consistent findings in clinical studies. Research indicates that most individuals regain a significant proportion of lost weight within the first year after stopping GLP-1 medications. The STEP 1 extension study of semaglutide cessation showed participants regained approximately two-thirds of their lost weight within 12 months. This occurs because the appetite-suppressing effects disappear, gastric emptying returns to normal, and metabolic adaptations that occurred during weight loss (such as reduced energy expenditure) persist.
Cardiovascular benefits associated with specific GLP-1 medications (liraglutide, semaglutide, dulaglutide) have been demonstrated during active treatment in high-risk populations. While there is no evidence suggesting immediate increased cardiovascular risk upon cessation, the return of elevated blood glucose and weight regain may gradually increase cardiovascular risk factors over time.
Patients should not abruptly stop GLP-1 medications without medical consultation. If discontinuation is planned, your GP or diabetes specialist can help develop a transition plan that may include:
Intensifying lifestyle modifications
Introducing or adjusting alternative medications
Reviewing and potentially reducing insulin or sulfonylurea doses to avoid hypoglycaemia
Increasing monitoring frequency
Setting realistic expectations about metabolic changes
Seek urgent medical help if you experience:
Severe hyperglycaemia (excessive thirst, frequent urination, fatigue)
Dehydration
Persistent vomiting
Severe abdominal pain
The appropriate duration of GLP-1 therapy is highly individualised and depends on multiple clinical and personal factors. Understanding these variables helps patients and clinicians make informed decisions about treatment continuation.
Disease severity and progression significantly influence treatment duration. Individuals with well-controlled type 2 diabetes who have made substantial lifestyle changes may successfully reduce or stop GLP-1 medications whilst maintaining glycaemic targets. Conversely, those with longstanding diabetes, insulin resistance, or multiple complications often require ongoing pharmacological support. The presence of cardiovascular disease is particularly relevant, as certain GLP-1 medications (semaglutide, liraglutide, and dulaglutide) have demonstrated cardiovascular benefits in specific high-risk populations that may justify continued use even if glucose control could be maintained through other means.
Lifestyle modification success is perhaps the most modifiable factor. Patients who achieve and sustain significant dietary improvements, regular physical activity, and behavioural changes may reduce their dependence on medication. However, maintaining these changes long-term is challenging, and realistic assessment of sustainability is crucial. Research consistently shows that combined pharmacological and lifestyle interventions produce superior outcomes to either approach alone.
Treatment response and side effects also guide duration decisions. Some individuals experience excellent efficacy with minimal adverse effects, making long-term treatment more acceptable. Others may struggle with persistent gastrointestinal symptoms (nausea, vomiting, diarrhoea) or other tolerability issues that limit treatment duration. Safety considerations such as a history of pancreatitis, gallbladder disease, or diabetic retinopathy may also influence continuation decisions, as these conditions require careful monitoring during GLP-1 therapy.
Additional considerations include:
Age and life expectancy: Treatment goals may differ for younger versus older patients
Comorbidities: Conditions such as chronic kidney disease may influence medication choices (e.g., exenatide should be avoided in severe renal impairment)
Pregnancy planning: GLP-1 medications should be stopped before conception (e.g., semaglutide at least 2 months before planned pregnancy) and are not recommended during breastfeeding
Personal preferences: Patient autonomy and quality of life considerations
Financial factors: Medication costs and NHS funding criteria
Risk of complications: Higher risk may justify longer treatment duration
For individuals considering stopping or reducing GLP-1 medications, multiple alternative approaches exist for managing type 2 diabetes and obesity. The optimal strategy typically involves a combination of interventions tailored to individual circumstances.
Lifestyle interventions remain the cornerstone of long-term management. Evidence-based approaches include structured weight management programmes, such as those recommended by NICE, which combine dietary modification, increased physical activity, and behavioural support. The NHS Diabetes Prevention Programme offers resources for individuals at risk of or living with type 2 diabetes. Achieving even modest sustained weight loss (5–10% of body weight) through lifestyle changes can significantly improve glycaemic control and reduce cardiovascular risk. However, maintaining weight loss without pharmacological support requires ongoing commitment and often benefits from continued professional support.
Alternative pharmacological options for type 2 diabetes include several medication classes with different mechanisms of action:
Metformin: First-line oral therapy that improves insulin sensitivity
SGLT2 inhibitors: Promote glucose excretion through urine and offer cardiovascular and renal benefits
DPP-4 inhibitors: Enhance natural GLP-1 activity with lower efficacy than GLP-1 receptor agonists
Insulin therapy: May be necessary for advanced diabetes or inadequate control with oral agents
For weight management, alternative medications include orlistat (a lipase inhibitor), naltrexone/bupropion (Mysimba), and tirzepatide (Mounjaro/Zepbound, a dual GIP/GLP-1 receptor agonist). These are typically prescribed through specialist weight management services with specific eligibility criteria. Bariatric surgery represents a highly effective intervention for severe obesity and often produces diabetes remission. In the UK, referral for bariatric surgery follows NICE guidelines with specific BMI thresholds and is typically accessed through Tier 3/4 specialist weight management services.
Long-term success strategies should include:
Regular monitoring of HbA1c, weight, and cardiovascular risk factors
Ongoing engagement with healthcare professionals (GP, practice nurse, dietitian)
Realistic goal-setting and expectation management
Addressing psychological factors, including emotional eating and motivation
Building sustainable habits rather than relying solely on willpower
When to contact your GP:
Blood glucose levels consistently above target range
Unexplained weight gain exceeding 5% of body weight
Development of diabetes complications (vision changes, foot problems, persistent infections)
Difficulty maintaining lifestyle modifications
Concerns about medication side effects or treatment decisions
Seek urgent medical help if you experience:
Severe upper abdominal pain (possible pancreatitis)
Persistent vomiting or dehydration
Symptoms of gallstones (pain, jaundice)
Severe hyperglycaemia
If you experience suspected side effects from any medication, report them to the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Ultimately, the decision about GLP-1 treatment duration should be made collaboratively, with regular review to ensure the management plan remains appropriate, effective, and aligned with individual goals and circumstances.
You can stop GLP-1 medications under medical supervision, but most people regain significant weight after cessation. Your GP or specialist can help develop a transition plan including lifestyle modifications and alternative treatments to maintain your progress.
Blood glucose levels typically rise within days to weeks after stopping GLP-1 medications, with HbA1c often returning towards baseline within 3–6 months unless alternative management strategies are implemented. Your healthcare team should adjust your treatment plan accordingly.
Yes, alternatives include sustained lifestyle modifications, other diabetes medications (metformin, SGLT2 inhibitors, DPP-4 inhibitors, insulin), structured weight management programmes, and in some cases bariatric surgery. The optimal approach is individualised and often combines multiple strategies.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.