Many people with type 2 diabetes wonder whether insulin and Ozempic (semaglutide) can be used together. The answer is yes—these medications can be prescribed in combination when blood glucose control cannot be achieved with either therapy alone. Ozempic, a GLP-1 receptor agonist, works through different mechanisms to insulin, addressing multiple aspects of type 2 diabetes simultaneously. However, combining these treatments increases the risk of hypoglycaemia and requires careful medical supervision. This article explains when combination therapy may be appropriate, how doses are adjusted, and essential safety considerations for anyone taking both medications under specialist guidance.
Quick Answer: Insulin and Ozempic can be prescribed together for type 2 diabetes when blood glucose control is inadequate with either medication alone, but this combination must be initiated and monitored by healthcare professionals.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereYes, insulin and Ozempic (semaglutide) can be prescribed together for adults with type 2 diabetes when blood glucose control cannot be achieved with either medication alone. Semaglutide is licensed for use with other glucose-lowering medicines including insulin (MHRA/EMC SmPC), and NICE guidelines (NG28) support GLP-1 receptor agonist use with insulin in specific circumstances.
Ozempic is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed for type 2 diabetes management only. It is not approved for type 1 diabetes or diabetic ketoacidosis (DKA) and does not replace insulin. Insulin remains the most effective glucose-lowering therapy available. When used in combination, these medications work through complementary mechanisms to improve blood glucose control. However, this combination must be initiated and monitored by healthcare professionals due to the increased risk of hypoglycaemia (low blood sugar) and the need for careful dose adjustments.
The decision to combine these therapies typically occurs when:
A person's HbA1c remains above target despite maximum tolerated doses of other therapies
Existing insulin therapy is insufficient to achieve glycaemic control
There is a need to reduce insulin doses whilst maintaining glucose control
NICE criteria for adding a GLP-1 RA are met (including BMI thresholds and response criteria)
It is essential that patients never initiate this combination independently. Your GP or diabetes specialist team will assess your individual circumstances, current medications, diabetes duration, and overall health status before recommending combination therapy. They will provide specific guidance on dosing schedules, blood glucose monitoring frequency, and signs of potential complications. If you are currently taking insulin and your healthcare provider is considering adding Ozempic, or vice versa, expect close monitoring during the initial adjustment period.
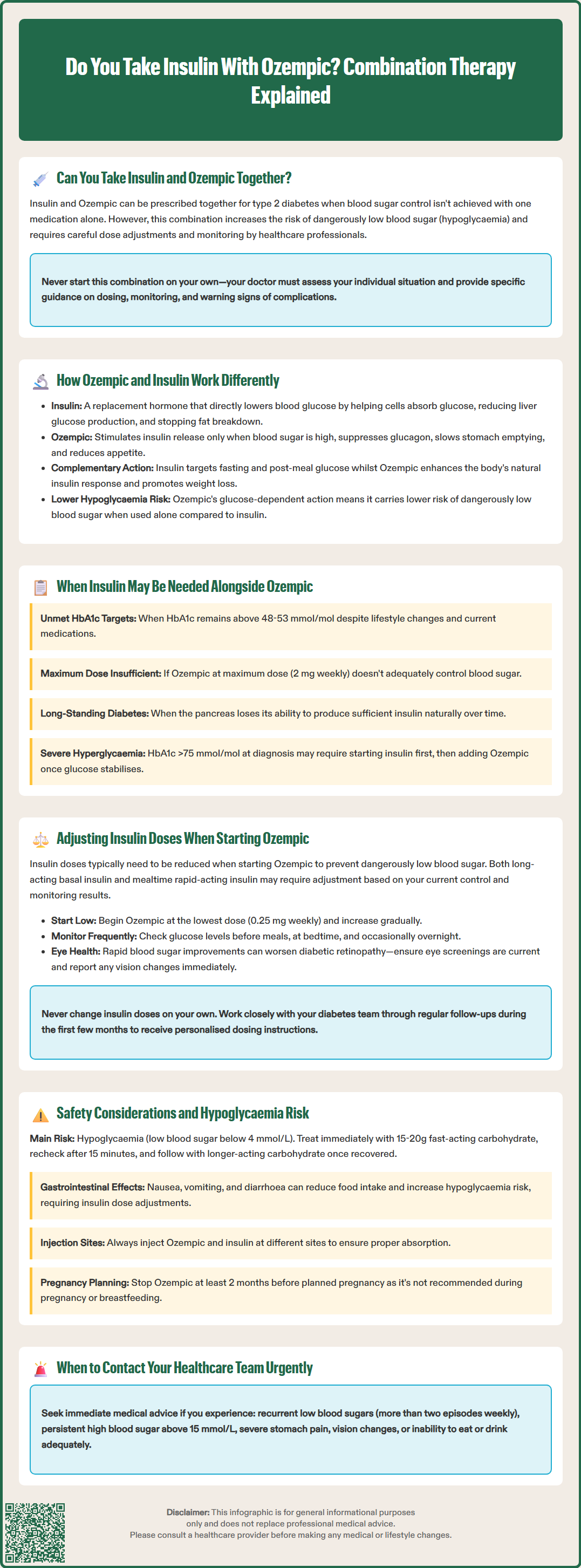
Understanding the distinct mechanisms of action helps explain why these medications can be used together effectively. Insulin is a replacement hormone that directly lowers blood glucose by facilitating glucose uptake into cells, suppressing hepatic glucose production, and inhibiting fat breakdown. People with type 2 diabetes have insulin resistance and progressive beta-cell dysfunction, often requiring exogenous insulin to maintain adequate glycaemic control.
Ozempic works through multiple complementary pathways. As a GLP-1 receptor agonist, semaglutide:
Enhances glucose-dependent insulin secretion – stimulating the pancreas to release insulin only when blood glucose is elevated, reducing hypoglycaemia risk
Suppresses glucagon secretion – decreasing the liver's glucose output when it is not needed
Slows gastric emptying – reducing post-meal glucose spikes by delaying food absorption
Promotes satiety – acting on brain appetite centres to reduce food intake and support weight loss
These differing mechanisms mean that Ozempic addresses several pathophysiological defects in type 2 diabetes simultaneously, whilst insulin primarily addresses the absolute or relative insulin deficiency. The glucose-dependent nature of Ozempic's action means it carries a lower intrinsic hypoglycaemia risk compared to insulin when used alone.
When combined, basal insulin primarily targets fasting glucose levels, while prandial (mealtime) insulin addresses post-meal glucose excursions. Ozempic enhances the body's own insulin response, reduces appetite, and often facilitates weight loss—a significant benefit since many people with type 2 diabetes struggle with weight management on insulin therapy alone. This complementary action can lead to improved overall glycaemic control with potentially lower total insulin requirements.
Several clinical scenarios warrant the addition of insulin to Ozempic therapy, or conversely, adding Ozempic to existing insulin regimens. NICE guidelines (NG28) recommend considering combination therapy when HbA1c targets are not achieved with lifestyle modifications and existing pharmacological interventions.
Common situations requiring combination therapy include:
Inadequate glycaemic control on Ozempic alone – When a person has been titrated to the maximum dose of Ozempic (2 mg weekly) but HbA1c remains above their individualised target (NICE recommends targets typically between 48-53 mmol/mol for most people with type 2 diabetes, though this should be individualised)
Long-standing diabetes with significant beta-cell dysfunction – As type 2 diabetes progresses, the pancreas's ability to produce insulin diminishes, necessitating exogenous insulin supplementation even with optimal GLP-1 receptor agonist therapy
Severe hyperglycaemia at diagnosis – NICE guidance suggests considering insulin therapy for people presenting with markedly elevated blood glucose (HbA1c >75 mmol/mol or symptoms of hyperglycaemia), with Ozempic potentially added once glucose levels stabilise
Weight management concerns on insulin – Adding Ozempic to existing insulin therapy can help reduce insulin doses, potentially limiting insulin-associated weight gain whilst improving glucose control
Your diabetes team will assess multiple factors before recommending combination therapy, including your current HbA1c, diabetes duration, presence of complications, other medications, kidney function, and personal treatment goals. They will also consider whether intensifying other aspects of your diabetes management—such as dietary modifications or increasing physical activity—might achieve targets before adding another medication. Regular review appointments ensure the treatment regimen remains appropriate for your evolving needs.
Insulin dose reduction is typically necessary when initiating Ozempic to minimise hypoglycaemia risk. The glucose-lowering effects of semaglutide, combined with existing insulin therapy, can significantly increase the likelihood of low blood sugar episodes if insulin doses remain unchanged.
General principles for dose adjustment include:
Basal insulin adjustment – Many clinicians may recommend reducing long-acting insulin (such as insulin glargine, detemir, or degludec) when starting Ozempic. The exact reduction should be individualised based on current glycaemic control, hypoglycaemia risk, and ongoing monitoring
Mealtime insulin consideration – Short-acting or rapid-acting insulin doses may require adjustment due to Ozempic's effects on gastric emptying and post-meal glucose excursions
Gradual Ozempic titration – Starting with the lowest dose (0.25 mg weekly for four weeks, then 0.5 mg) allows time to assess glucose response and adjust insulin accordingly. Doses can be increased to 1 mg weekly after at least 4 weeks, and if needed, to the maximum 2 mg weekly dose based on response and tolerability (per SmPC)
Individualised approach – Dose adjustments depend on baseline insulin requirements, current glycaemic control, hypoglycaemia history, and individual response to Ozempic
Enhanced blood glucose monitoring is essential during this transition period. Your healthcare team will likely recommend checking blood glucose more frequently—typically before meals and at bedtime, and occasionally during the night initially—to identify patterns and guide dose adjustments. Keep a detailed record of readings, insulin doses, meals, and any hypoglycaemic episodes.
Important safety consideration: Rapid improvements in blood glucose control with semaglutide can worsen diabetic retinopathy in some patients, particularly those with pre-existing retinopathy who are also on insulin. Ensure your eye screening is up to date and report any new or worsening visual symptoms promptly.
Never adjust insulin doses independently without guidance from your diabetes team. They will provide specific instructions tailored to your regimen, whether you use a basal-bolus regimen, premixed insulin, or another approach. Expect several follow-up appointments or telephone consultations during the first few months to optimise your treatment.
The primary safety concern when combining Ozempic and insulin is hypoglycaemia (blood glucose below 4 mmol/L). Whilst Ozempic alone carries minimal hypoglycaemia risk due to its glucose-dependent mechanism, the addition of insulin—which lowers blood glucose regardless of current levels—substantially increases this risk.
Recognising and managing hypoglycaemia:
Early warning signs include trembling, sweating, anxiety, hunger, palpitations, and difficulty concentrating
Immediate treatment involves consuming 15-20g of fast-acting carbohydrate (e.g., glucose tablets, 150-200ml fruit juice, or 4-5 jelly babies)
Recheck blood glucose after 15 minutes and repeat treatment if still below 4 mmol/L
Follow with a longer-acting carbohydrate (e.g., slice of bread, biscuits) once blood glucose recovers
Additional safety considerations include:
Diabetic retinopathy – Semaglutide may worsen diabetic retinopathy, particularly in those with pre-existing retinopathy and when rapid HbA1c reductions occur. Ensure regular eye screening and report any new or worsening visual symptoms immediately
Gastrointestinal effects – Ozempic commonly causes nausea, vomiting, and diarrhoea, particularly when initiating therapy or increasing doses. These effects can impact food intake and increase hypoglycaemia risk if insulin doses are not adjusted
Gallbladder disease – Semaglutide has been associated with increased risk of gallstones and cholecystitis
Kidney function – While semaglutide does not require dose adjustment in renal impairment, severe gastrointestinal symptoms may lead to dehydration and acute kidney injury. Insulin doses may need reduction as renal function declines
Pregnancy and breastfeeding – Ozempic is not recommended during pregnancy or breastfeeding. Effective contraception is advised during treatment, and Ozempic should be discontinued at least 2 months before a planned pregnancy
Injection site management – Administer Ozempic and insulin at different injection sites to avoid potential absorption issues
Pancreatitis awareness – Though rare, severe abdominal pain should prompt immediate medical attention, as GLP-1 receptor agonists carry a potential pancreatitis risk
When to contact your healthcare team urgently:
Recurrent hypoglycaemia (more than two episodes below 4 mmol/L weekly)
Severe hypoglycaemia requiring assistance from another person
Persistent hyperglycaemia (blood glucose consistently above 15 mmol/L)
Severe gastrointestinal symptoms preventing adequate food or fluid intake
New or worsening visual symptoms
Signs of diabetic ketoacidosis (excessive thirst, frequent urination, confusion, fruity breath odour)
Ensure you have an up-to-date diabetes management plan, including emergency contact numbers and clear instructions for sick day management. Never stop basal insulin during illness, and consider ketone testing when unwell. Carry glucose tablets or another fast-acting carbohydrate source at all times, and consider wearing medical identification indicating you have diabetes and use insulin.
Suspected side effects should be reported via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Yes, insulin and Ozempic can be safely prescribed together for type 2 diabetes when supervised by healthcare professionals. This combination requires careful dose adjustments and enhanced blood glucose monitoring to minimise hypoglycaemia risk.
Doctors prescribe both medications when HbA1c remains above target despite maximum doses of other therapies, when long-standing diabetes causes significant beta-cell dysfunction, or when weight management on insulin alone is problematic. The medications work through complementary mechanisms to improve overall glucose control.
Insulin doses typically require reduction when initiating Ozempic to prevent hypoglycaemia, as the combined glucose-lowering effects significantly increase low blood sugar risk. Your diabetes team will provide individualised dose adjustment guidance with enhanced monitoring during the transition period.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.