Does GLP-1 decrease muscle mass? This question concerns many patients considering or currently using GLP-1 receptor agonists such as semaglutide (Wegovy, Ozempic) or liraglutide (Saxenda, Victoza) for weight management or type 2 diabetes. Whilst these medications produce substantial weight loss, understanding their impact on body composition—particularly muscle tissue—is essential for safe, effective treatment. Current evidence suggests that GLP-1 medications do not cause disproportionate muscle loss compared to equivalent weight loss achieved through other methods. However, proactive strategies including adequate protein intake and resistance training remain crucial for preserving lean mass during treatment.
Quick Answer: GLP-1 receptor agonists do not appear to cause disproportionate muscle loss compared to equivalent weight loss achieved through other methods.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications originally developed for type 2 diabetes management, with some now specifically licensed for weight management. These medicines include semaglutide (Ozempic for diabetes; Wegovy for weight management), liraglutide (Victoza for diabetes; Saxenda for weight management), and dulaglutide (Trulicity for diabetes). Tirzepatide (Mounjaro) is a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist currently licensed for diabetes in the UK.
GLP-1 is a naturally occurring incretin hormone released by the intestine in response to food intake. GLP-1 receptor agonists work by mimicking this hormone's effects on multiple body systems. The primary mechanisms of action include:
Enhancing insulin secretion from pancreatic beta cells in a glucose-dependent manner, which helps lower blood glucose levels (with a low but not zero risk of hypoglycaemia, particularly when combined with insulin or sulfonylureas)
Suppressing glucagon release from pancreatic alpha cells, reducing hepatic glucose production
Slowing gastric emptying, which prolongs satiety and reduces appetite
Acting on appetite centres in the brain, particularly the hypothalamus, to reduce hunger and food intake
In the UK, only semaglutide (Wegovy) and liraglutide (Saxenda) are specifically licensed for weight management in adults with a body mass index (BMI) of 30 kg/m² or greater, or 27 kg/m² or greater with at least one weight-related comorbidity. NHS access is typically via specialist weight management services and subject to specific eligibility criteria outlined in NICE technology appraisals. The substantial weight loss achieved—typically 10–15% of body weight with semaglutide 2.4mg as demonstrated in the STEP clinical trials—has raised important questions about body composition changes during treatment.
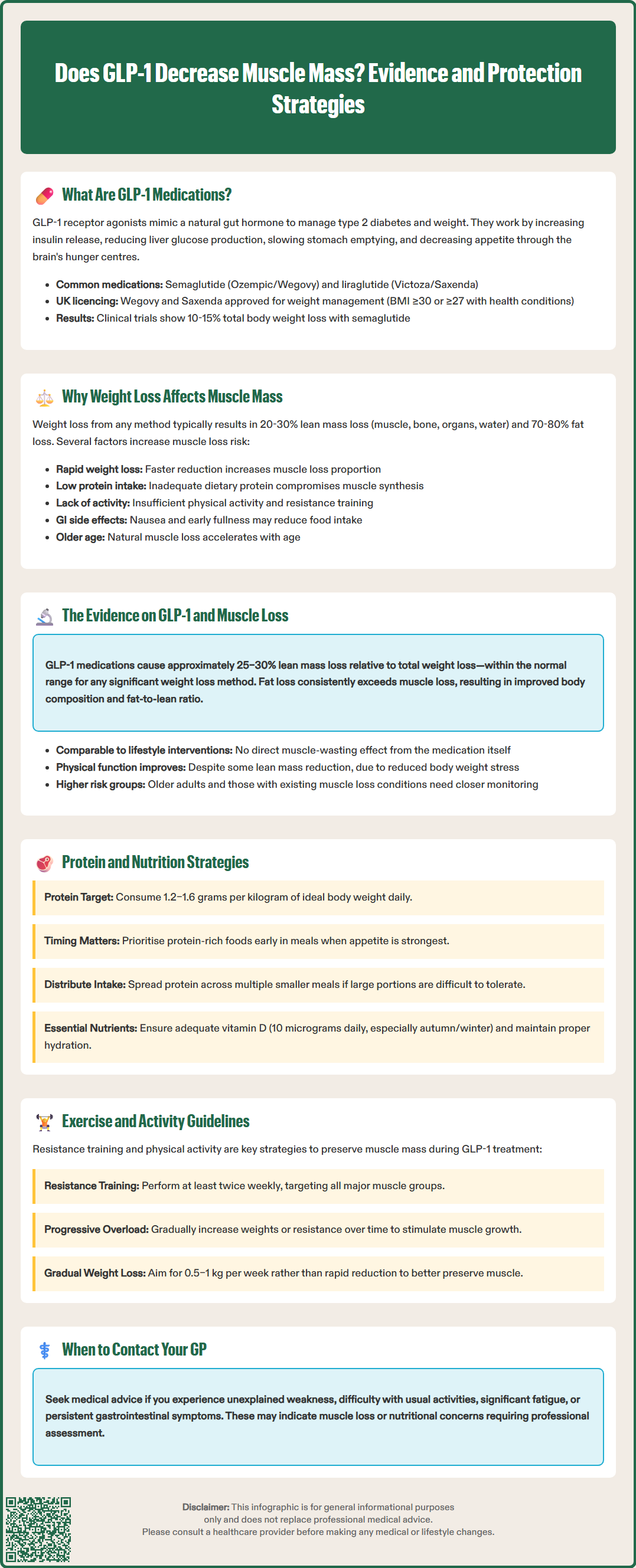
Weight loss, regardless of the method used, typically results in loss of both fat mass and lean body mass (which includes muscle, bone, organs, and water). This is a well-established physiological phenomenon observed across different weight loss interventions, including dietary restriction, bariatric surgery, and pharmacotherapy.
During caloric restriction, the body mobilises energy stores to meet metabolic demands. Whilst adipose tissue provides the majority of energy, some lean tissue is inevitably lost. Research consistently demonstrates that approximately 20–30% of weight lost through caloric restriction comprises lean mass, with the remainder being fat mass. Early weight loss measurements may overestimate true muscle loss due to changes in fluid and glycogen stores. This proportion can vary considerably depending on several factors:
Rate of weight loss: Rapid weight loss tends to result in greater proportional lean mass loss
Baseline body composition: Individuals with lower initial fat mass may lose proportionally more lean tissue
Protein intake: Inadequate dietary protein increases muscle protein breakdown
Physical activity levels: Resistance training and adequate physical activity help preserve muscle mass
Age: Older adults are more susceptible to muscle loss during weight reduction
The concern with GLP-1 medications centres on whether they cause disproportionate muscle loss compared to other weight loss methods. The appetite suppression and reduced food intake associated with these medications can lead to inadequate protein consumption if patients are not properly counselled. Additionally, the gastrointestinal side effects—including nausea, vomiting, and early satiety—may further compromise nutritional intake, potentially affecting muscle protein synthesis. Understanding these mechanisms is essential for implementing appropriate protective strategies during GLP-1 treatment.
Current evidence suggests that GLP-1 receptor agonists do not appear to cause disproportionate muscle loss compared to equivalent weight loss achieved through other methods, though individual responses may vary. Multiple clinical trials and real-world studies have examined body composition changes during GLP-1 treatment, providing generally reassuring data.
The STEP (Semaglutide Treatment Effect in People with obesity) trials included body composition sub-studies using dual-energy X-ray absorptiometry (DEXA) scanning. These studies demonstrated that approximately 25–30% of total weight loss comprised lean mass, which falls within the expected range for substantial weight loss interventions. Importantly, the absolute amount of fat mass lost was considerably greater than lean mass lost, resulting in improved body composition overall.
Key findings from clinical research include:
The proportion of lean mass loss with GLP-1 medications appears comparable to that seen with lifestyle interventions alone
Fat mass loss consistently exceeds lean mass loss, improving the overall fat-to-lean ratio
Some evidence suggests improvements in physical function despite some lean mass reduction, likely due to decreased mechanical load and improved metabolic health, though more research is needed
Individual responses vary, with some patients experiencing greater lean mass preservation than others
A 2023 systematic review published in Obesity Reviews concluded that whilst lean mass decreases during GLP-1 treatment, this reflects the expected consequences of weight loss rather than a direct catabolic effect of the medication. The ratio of fat loss to lean mass loss with GLP-1 therapy appears favourable compared to many other weight loss interventions. However, individual variation exists, and certain patient groups—particularly older adults, those with pre-existing sarcopenia, or individuals with very low baseline muscle mass—may require enhanced monitoring and intervention strategies to optimise body composition outcomes during treatment.
Preserving muscle mass during GLP-1 treatment requires a proactive, multifaceted approach focusing on adequate nutrition and appropriate physical activity. Healthcare professionals should provide comprehensive lifestyle guidance alongside prescribing these medications.
Optimising protein intake is the cornerstone of muscle preservation. Current evidence supports consuming 1.2–1.6 grams of protein per kilogram of ideal body weight daily, distributed across meals, though this should be individualised. People with kidney or liver disease should consult their healthcare provider before increasing protein intake. High-quality protein sources include:
Lean meats, poultry, and fish
Eggs and dairy products
Legumes, beans, and lentils
Protein supplements if dietary intake is insufficient
Given the appetite-suppressing effects of GLP-1 medications, patients should prioritise protein-rich foods early in meals when appetite is strongest. Smaller, more frequent protein-containing meals may be better tolerated than large portions.
Resistance training is essential for maintaining and building muscle mass during weight loss. The UK Chief Medical Officers' Physical Activity Guidelines emphasise the importance of muscle-strengthening activities, and this is particularly relevant for patients on GLP-1 therapy. Recommended strategies include:
Resistance exercises at least 2 times weekly, targeting all major muscle groups
Progressive overload, gradually increasing weights or resistance
Adequate recovery between training sessions
Combining resistance training with moderate aerobic activity for overall health benefits
Additional protective measures include ensuring adequate vitamin D status (the NHS recommends 10 micrograms daily, particularly during autumn and winter), maintaining proper hydration, and aiming for gradual, sustainable weight loss of 0.5–1 kg per week rather than rapid reduction.
When to seek medical advice: Contact your GP if you experience unexplained weakness, difficulty performing usual activities, significant fatigue, persistent gastrointestinal symptoms, or concerns about nutritional intake. Simple functional assessments (such as grip strength or chair-rise tests) may be useful for monitoring, with specialist referral for more detailed body composition assessment if concerns arise. Referral to a registered dietitian can provide personalised nutritional guidance, whilst physiotherapy or exercise specialist input may benefit those new to resistance training or with mobility limitations.
If you experience any suspected side effects from GLP-1 medications, report them through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Approximately 25–30% of total weight lost during GLP-1 treatment comprises lean mass, which is comparable to other weight loss methods. The majority of weight lost is fat mass, resulting in improved overall body composition.
Yes, muscle loss can be minimised through adequate protein intake (1.2–1.6g per kg ideal body weight daily) and resistance training at least twice weekly. Prioritising protein-rich foods early in meals and ensuring gradual weight loss also help preserve lean tissue.
Older adults may be more susceptible to muscle loss during weight reduction and may benefit from enhanced monitoring, increased protein intake, and structured resistance training. Healthcare providers should assess individual risk factors and provide tailored guidance.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.