Mounjaro (tirzepatide) is a dual incretin hormone receptor agonist licensed in the UK for type 2 diabetes mellitus, working through fundamentally hormonal mechanisms. By mimicking naturally occurring GIP and GLP-1 hormones, it influences insulin secretion, glucagon suppression, and appetite regulation. Understanding whether Mounjaro affects hormones beyond glucose control is essential for safe prescribing, particularly regarding reproductive health, thyroid function, and metabolic pathways. This article examines tirzepatide's hormonal effects, contraceptive interactions, thyroid safety considerations, and clinical monitoring requirements in line with UK guidance from NICE, MHRA, and the SmPC.
Quick Answer: Mounjaro (tirzepatide) primarily affects metabolic hormones—insulin and glucagon—but also impacts oral contraceptive absorption and requires thyroid safety monitoring due to preclinical findings.
Mounjaro (tirzepatide) is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. For weight management in adults with obesity or overweight with weight-related comorbidities, tirzepatide may be available under a different brand name. Its primary mechanism of action is fundamentally hormonal, working by mimicking two naturally occurring incretin hormones that play crucial roles in metabolic regulation.
Incretin hormones are released from the gastrointestinal tract in response to food intake and serve multiple physiological functions. GLP-1 stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner, suppresses glucagon release, slows gastric emptying, and promotes satiety through central nervous system pathways. GIP, the second incretin hormone targeted by tirzepatide, also enhances insulin secretion and may influence fat metabolism and energy expenditure. By activating both GIP and GLP-1 receptors simultaneously, Mounjaro produces a synergistic effect that is more potent than single-receptor agonists.
The dual agonist approach represents a significant advancement in incretin-based therapy. Clinical trials (SURPASS programme) have demonstrated that tirzepatide's combined action on both receptor pathways results in improved glycaemic control and weight reduction compared to selective GLP-1 receptor agonists at studied doses. The medication is administered once weekly via subcutaneous injection, with doses ranging from 2.5 mg to 15 mg, typically starting at 2.5 mg and increasing in 2.5 mg increments based on therapeutic goals and tolerability. Understanding this hormonal mechanism is essential for appreciating how Mounjaro may influence various endocrine systems throughout the body, beyond its primary metabolic effects.
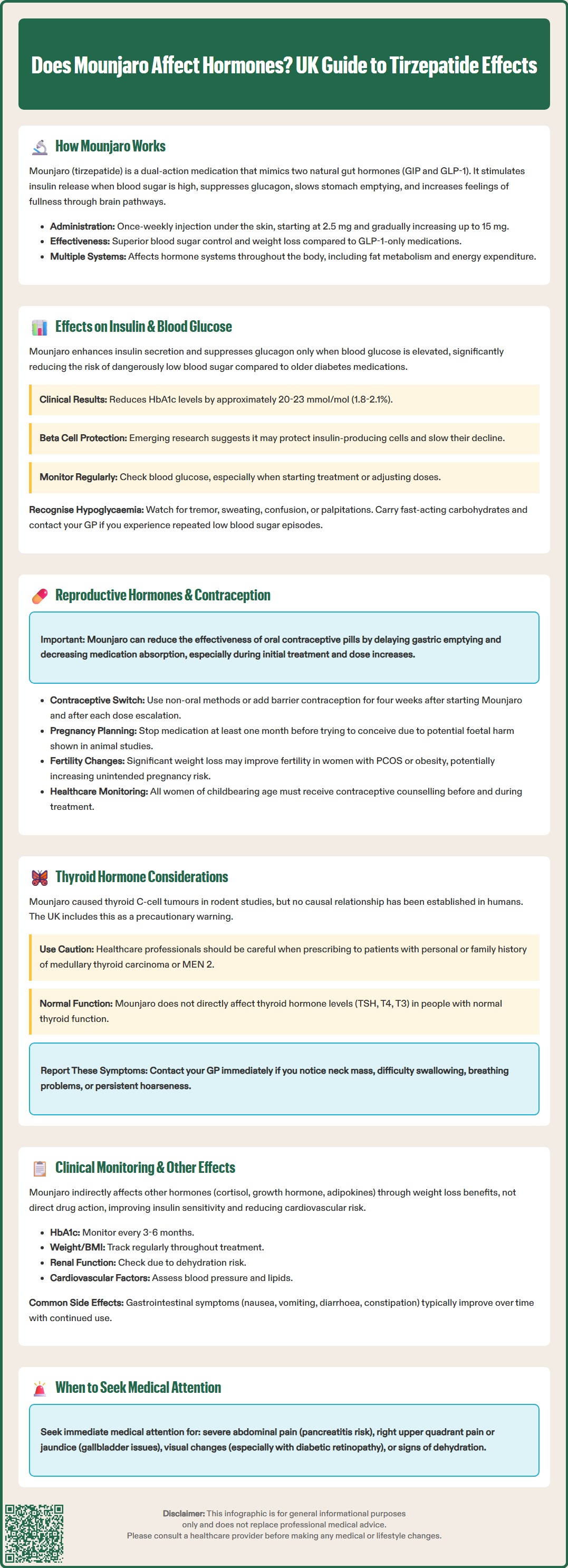
Mounjaro's most direct and clinically significant hormonal effects involve the regulation of insulin and glucagon, the two primary hormones controlling blood glucose homeostasis. Through its GLP-1 and GIP receptor agonism, tirzepatide enhances glucose-dependent insulin secretion from pancreatic beta cells. This mechanism is particularly advantageous because insulin release occurs only when blood glucose levels are elevated, substantially reducing the risk of hypoglycaemia compared to insulin secretagogues such as sulphonylureas.
Simultaneously, Mounjaro suppresses glucagon secretion from pancreatic alpha cells in a glucose-dependent manner. Glucagon normally raises blood glucose by promoting hepatic glucose production; its suppression during hyperglycaemia contributes to improved glycaemic control. This dual action—enhancing insulin whilst reducing glucagon—creates a favourable hormonal environment for glucose regulation. Clinical studies have shown HbA1c reductions of approximately 20-23 mmol/mol (1.8% to 2.1%) across various doses, with many patients achieving target glycaemic levels.
Beyond acute effects on insulin and glucagon, there is some preclinical and limited clinical evidence suggesting that GLP-1 receptor agonists may have beta-cell protective effects, potentially slowing the progressive decline in insulin secretory capacity characteristic of type 2 diabetes. Long-term data for tirzepatide specifically are still accumulating, and this remains an area of ongoing research rather than an established clinical benefit.
Patient monitoring should include regular blood glucose testing, particularly during dose titration. Individuals using Mounjaro alongside insulin or sulphonylureas require careful dose adjustments of these medications to prevent hypoglycaemia, in line with NICE guidance (NG28). Healthcare professionals should educate patients about recognising hypoglycaemic symptoms—tremor, sweating, confusion, palpitations—and the importance of carrying fast-acting carbohydrates. Patients should contact their GP if experiencing recurrent hypoglycaemia or difficulty maintaining stable glucose levels.
An important consideration for women of childbearing potential is that Mounjaro may affect the absorption and efficacy of oral contraceptives, particularly during the initial weeks of treatment. Tirzepatide delays gastric emptying, which can reduce the absorption of orally administered medications, including combined oral contraceptive pills and progestogen-only pills. The UK SmPC specifically addresses this interaction, recommending that women using oral contraceptives should switch to a non-oral contraceptive method or add a barrier method for four weeks after initiating Mounjaro and for four weeks after each dose escalation.
This interaction has significant clinical implications. Unintended pregnancy whilst taking tirzepatide is undesirable, as animal studies have shown potential foetal harm, including structural abnormalities and reduced foetal growth. Consequently, Mounjaro should not be used during pregnancy, and women should discontinue the medication at least one month before a planned pregnancy to allow adequate washout time, as specified in the UK SmPC. Healthcare professionals must discuss contraceptive planning thoroughly with all women of reproductive age before prescribing tirzepatide.
Regarding other reproductive hormones, there is currently no official link established between Mounjaro and direct effects on oestrogen, progesterone, or testosterone levels. However, significant weight loss—a common outcome with tirzepatide therapy—can independently influence reproductive hormone balance. Weight reduction in women with polycystic ovary syndrome (PCOS) or obesity may improve ovulatory function and fertility, potentially increasing pregnancy risk if contraception is inadequate.
Clinical guidance emphasises the importance of pre-treatment counselling. Women should be advised about contraceptive requirements, pregnancy planning, and the need to inform their healthcare provider immediately if pregnancy is suspected. Regular review of contraceptive adequacy should form part of ongoing monitoring for women prescribed Mounjaro.
A safety consideration with Mounjaro relates to thyroid C-cell tumours, specifically medullary thyroid carcinoma (MTC). In rodent studies, GLP-1 receptor agonists, including tirzepatide, caused dose-dependent and treatment-duration-dependent thyroid C-cell tumours. Whilst the relevance of these findings to humans remains uncertain, and no causal relationship has been established in human clinical trials, the UK SmPC includes a warning about this potential risk.
The UK SmPC includes this as a precaution rather than a formal contraindication. However, healthcare professionals should exercise caution when considering tirzepatide for patients with a personal or family history of medullary thyroid carcinoma or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2), a hereditary condition associated with increased MTC risk. Before prescribing tirzepatide, clinicians should take a thorough personal and family history to identify these risk factors. Patients should be counselled about symptoms of thyroid tumours, including a neck mass, dysphagia, dyspnoea, or persistent hoarseness, and advised to report such symptoms promptly.
Regarding thyroid function itself, there is no official link between Mounjaro and alterations in thyroid-stimulating hormone (TSH), thyroxine (T4), or triiodothyronine (T3) levels in individuals with normal thyroid function. Tirzepatide does not directly affect thyroid hormone synthesis or metabolism. However, patients with pre-existing thyroid disorders should continue their usual thyroid function monitoring as clinically indicated.
Monitoring recommendations do not mandate routine thyroid function testing or calcitonin measurement in patients without risk factors. However, clinicians should maintain vigilance for symptoms suggestive of thyroid pathology. Any patient developing a thyroid nodule during treatment should be referred according to NICE guideline NG12 for suspected cancer recognition and referral. Patients should be advised to contact their GP if they notice any neck swelling or experience difficulty swallowing or breathing.
Beyond its primary metabolic and reproductive hormone considerations, Mounjaro may have indirect effects on other endocrine systems, largely mediated through weight loss and improved metabolic health. Significant weight reduction can influence cortisol metabolism, growth hormone dynamics, and adipokine profiles (hormones secreted by adipose tissue, such as leptin and adiponectin). These changes are generally beneficial, contributing to improved insulin sensitivity and reduced cardiovascular risk, though they are consequences of weight loss rather than direct drug effects.
Patients with adrenal insufficiency or those taking corticosteroids require no specific dose adjustments for Mounjaro, as there are no known direct interactions between tirzepatide and the hypothalamic-pituitary-adrenal axis. However, improved glycaemic control may necessitate adjustments to other medications, including corticosteroid doses in some clinical contexts. Similarly, there is no evidence that Mounjaro affects parathyroid hormone, growth hormone, or prolactin secretion directly.
Gastrointestinal hormones beyond GLP-1 and GIP may be indirectly influenced by tirzepatide's effects on gastric emptying and satiety. The medication's ability to promote fullness and reduce appetite involves complex interactions with central and peripheral appetite-regulating pathways. These effects contribute to the substantial weight loss observed in clinical trials but do not constitute adverse hormonal disruption.
Clinical monitoring should follow NICE guidance for type 2 diabetes management (NG28) or weight management protocols, depending on the indication. This includes regular assessment of:
Glycaemic control (HbA1c every 3–6 months)
Weight and body mass index
Renal function (as GLP-1 receptor agonists may cause dehydration through gastrointestinal side effects)
Cardiovascular risk factors (blood pressure, lipid profile)
Patients should be educated about common adverse effects, predominantly gastrointestinal (nausea, vomiting, diarrhoea, constipation), which typically diminish over time. Red flag symptoms requiring immediate medical attention include severe abdominal pain (potential pancreatitis), right upper quadrant pain or jaundice (potential gallbladder disease), visual changes (particularly in patients with pre-existing diabetic retinopathy, which may temporarily worsen with rapid glycaemic improvement), or signs of dehydration. Regular follow-up allows for dose optimisation, management of side effects, and adjustment of concomitant medications as metabolic parameters improve. Patients should maintain open communication with their healthcare team, report any concerning symptoms promptly, and report suspected side effects via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk), ensuring safe and effective use of this potent hormonal therapy.
Yes, Mounjaro delays gastric emptying, which may reduce absorption of oral contraceptives. Women should switch to non-oral contraception or add barrier methods for four weeks after starting treatment and after each dose increase.
Animal studies showed thyroid C-cell tumours with GLP-1 receptor agonists, though human relevance is uncertain. Mounjaro should be used cautiously in patients with personal or family history of medullary thyroid carcinoma or MEN 2 syndrome.
There is no established direct effect on oestrogen, progesterone, or testosterone levels. However, weight loss from tirzepatide may indirectly improve hormonal balance and fertility in women with obesity or PCOS.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.