LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Does Mounjaro cause muscle pain? Mounjaro (tirzepatide) is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus. Whilst gastrointestinal side effects such as nausea and vomiting are well-documented, some patients report musculoskeletal symptoms, including muscle pain. Although myalgia is not listed among the most common adverse effects in the MHRA-approved Summary of Product Characteristics, clinical trial data and post-marketing reports suggest a subset of users experience muscle discomfort. This article examines the evidence, explores potential mechanisms, and provides guidance on assessment and management of muscle pain in patients taking Mounjaro.
Quick Answer: Muscle pain is not a commonly reported side effect of Mounjaro (tirzepatide), though some patients experience musculoskeletal discomfort during treatment.
Mounjaro (tirzepatide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus. It belongs to a novel class of medications known as dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonists. By mimicking the action of these naturally occurring incretin hormones, Mounjaro helps regulate blood glucose levels, reduces appetite, and slows gastric emptying, leading to improved glycaemic control and weight loss. In the UK, tirzepatide for weight management is separately licensed under the brand name Zepbound.
As with all medications, Mounjaro is associated with a range of side effects, some of which are common and generally mild to moderate in severity. According to the MHRA-approved Summary of Product Characteristics (SmPC), the most frequently reported adverse effects are gastrointestinal in nature, including nausea (very common, ≥1/10), vomiting, diarrhoea, constipation, abdominal pain, and reduced appetite. These symptoms typically occur during the initial weeks of treatment or following dose escalation and often diminish over time as the body adjusts to the medication.
Other recognised side effects include injection site reactions (such as redness, swelling, or itching), fatigue, headache, and dizziness. Hypoglycaemia (low blood sugar) may occur, particularly when Mounjaro is used in combination with insulin or sulphonylureas. The risk of hypoglycaemia is lower when Mounjaro is used as monotherapy. Patients are advised to monitor for symptoms of hypoglycaemia, including sweating, tremor, palpitations, and confusion.
While the gastrointestinal effects are well-documented and expected, patients occasionally report musculoskeletal symptoms, including muscle pain or discomfort. Understanding whether these symptoms are directly related to Mounjaro, coincidental, or secondary to other factors is important for both patients and healthcare professionals managing treatment.
Muscle pain, medically termed myalgia, has been reported by some individuals taking Mounjaro, though it is not listed among the most common adverse effects in the Summary of Product Characteristics (SmPC) approved by the Medicines and Healthcare products Regulatory Agency (MHRA). In clinical trials evaluating tirzepatide for type 2 diabetes (SURPASS programme), musculoskeletal complaints—including muscle pain, joint pain (arthralgia), and back pain—were documented, but these occurred at relatively low frequencies.
According to the European Medicines Agency's European Public Assessment Report (EPAR) for tirzepatide, musculoskeletal adverse events were reported in clinical trials, but at rates that were generally comparable between tirzepatide and comparator groups. The specific frequency category for myalgia is not prominently featured in the core safety profile, suggesting it is not among the most commonly observed effects.
Post-marketing surveillance and patient-reported experiences suggest that a subset of users do experience muscle discomfort, aching, or stiffness whilst on Mounjaro. These reports vary considerably in terms of severity, location (generalised versus localised), and timing relative to treatment initiation or dose changes. Some patients describe a generalised muscle soreness similar to that experienced after physical exertion, whilst others report more focal discomfort in specific muscle groups.
It is important to note that there is no definitive, established causal link between Mounjaro and muscle pain based on current evidence. Individual responses to medications can vary, and it is plausible that certain patients may experience musculoskeletal symptoms as part of their unique reaction to the drug.
Healthcare professionals should take patient reports of muscle pain seriously, conducting a thorough assessment to determine whether the symptom is likely related to Mounjaro, attributable to another cause, or multifactorial. Documenting the onset, duration, severity, and any associated features (such as weakness, swelling, or systemic symptoms) is essential for appropriate clinical evaluation and management. Suspected adverse reactions can be reported via the MHRA Yellow Card scheme.
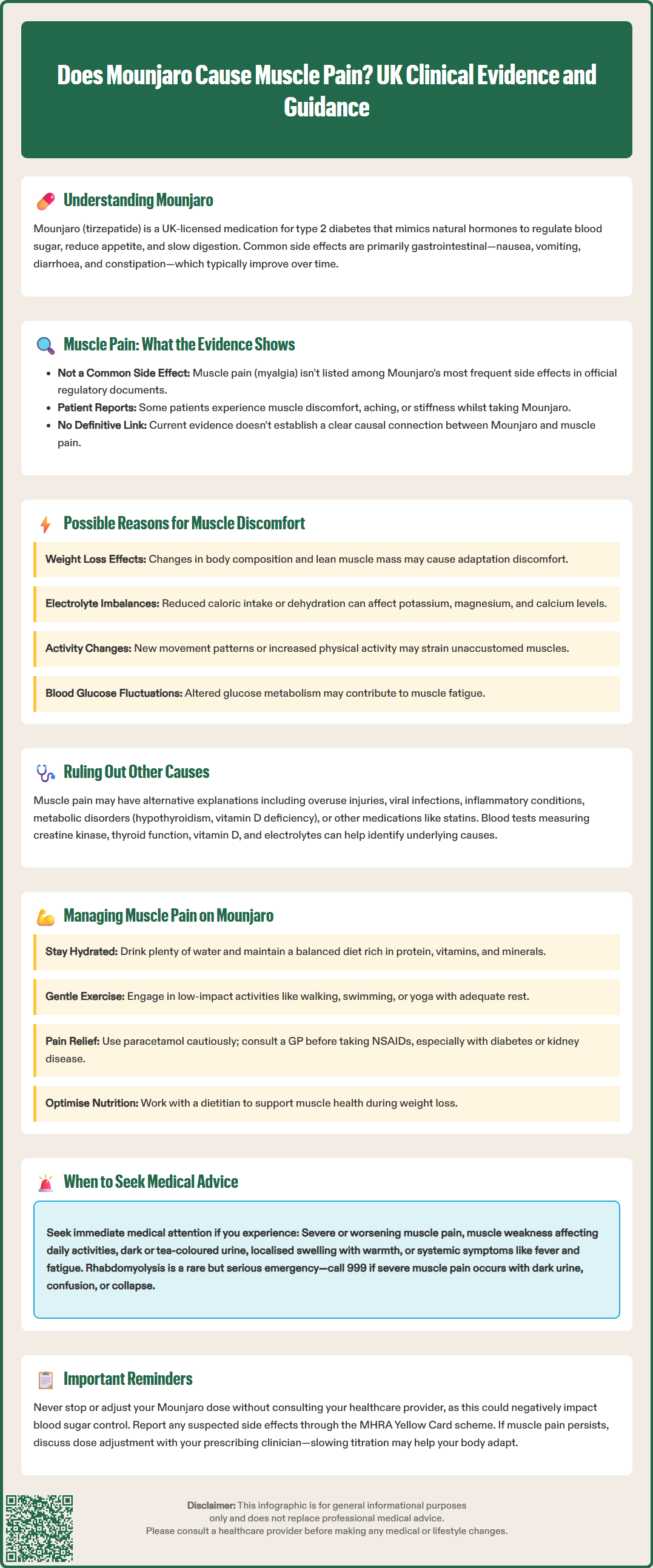
Although the precise mechanism by which Mounjaro might contribute to muscle pain is not fully elucidated, several hypotheses have been proposed based on the drug's pharmacological actions and the physiological changes it induces.
Weight loss is one plausible contributor. Mounjaro can promote significant weight reduction, and substantial weight loss can lead to changes in body composition. Analysis of body composition data from clinical trials suggests that while most weight loss is from fat mass, some loss of lean mass may also occur. This process may potentially result in muscle adaptation, fatigue, and discomfort in some individuals. Patients losing weight may also alter their physical activity levels or posture, inadvertently straining muscles unaccustomed to new movement patterns.
Metabolic and electrolyte shifts associated with weight loss and changes in dietary intake may also play a role. Reduced caloric intake, dehydration, or imbalances in electrolytes such as potassium, magnesium, or calcium can affect muscle function and lead to cramping, aching, or stiffness. Gastrointestinal side effects like vomiting or diarrhoea may exacerbate these imbalances.
Another consideration is the potential for indirect effects on muscle tissue through alterations in glucose metabolism and insulin sensitivity. While improved glycaemic control is generally beneficial, fluctuations in blood glucose levels—particularly if hypoglycaemia occurs—can cause muscle fatigue and discomfort.
It is worth emphasising that these mechanisms remain speculative, and further research is needed to clarify whether and how Mounjaro directly influences musculoskeletal symptoms. The current evidence base does not definitively establish a direct pharmacological mechanism by which tirzepatide would cause myalgia.
When a patient reports muscle pain whilst taking Mounjaro, it is essential to conduct a comprehensive clinical assessment to differentiate between drug-related effects and alternative aetiologies. Muscle pain is a common symptom with numerous potential causes, and attributing it solely to Mounjaro without proper evaluation may lead to missed diagnoses or inappropriate management.
Timing and pattern are important clues. Muscle pain that begins shortly after starting Mounjaro or following a dose increase may suggest a drug-related effect, particularly if no other obvious cause is present. Conversely, pain that predates treatment or develops independently of dosing changes is less likely to be directly attributable to the medication.
Clinicians should consider alternative musculoskeletal causes, including:
Overuse or injury: New exercise regimens, physical activity, or occupational strain
Inflammatory conditions: Polymyalgia rheumatica, fibromyalgia, or autoimmune myositis
Infections: Viral illnesses (e.g., influenza) commonly cause myalgia
Metabolic disorders: Hypothyroidism, vitamin D deficiency, or electrolyte disturbances
Medication interactions: Statins, for example, are well-known to cause myalgia and are often co-prescribed in patients with type 2 diabetes
Investigations may be warranted depending on clinical suspicion. Blood tests to assess creatine kinase (CK) levels, thyroid function, vitamin D status, electrolytes, and inflammatory markers (ESR, CRP) can help identify underlying causes. Persistent, severe, or progressive muscle pain—especially if accompanied by weakness, swelling, or systemic symptoms—requires prompt evaluation to exclude serious conditions such as rhabdomyolysis or inflammatory myopathy.
A detailed medication history, including over-the-counter supplements and recent changes to other prescriptions, is also essential. Collaborative discussion between the patient, GP, and specialist diabetes services ensures a thorough and patient-centred approach to diagnosis and management.
Patients should be advised not to stop or change their Mounjaro dose without consulting their healthcare professional, as abrupt discontinuation could affect blood glucose control.
For patients experiencing muscle pain whilst on Mounjaro, several practical strategies can help alleviate discomfort and support continued treatment, provided the pain is mild to moderate and not indicative of a serious underlying condition.
Lifestyle and self-care measures are often the first line of management:
Hydration: Ensuring adequate fluid intake helps maintain electrolyte balance and supports muscle function
Balanced nutrition: A diet rich in protein, vitamins (particularly B vitamins and vitamin D), and minerals (magnesium, potassium, calcium) supports muscle health during weight loss
Gradual physical activity: Gentle stretching, low-impact exercise (such as walking, swimming, or yoga), and progressive strength training can reduce stiffness and improve muscle tone without overexertion
Rest and recovery: Allowing adequate time for muscles to recover, particularly after physical activity, is important
Heat or cold therapy: Warm baths, heating pads, or cold compresses may provide symptomatic relief
Pharmacological options for symptom relief include over-the-counter analgesics such as paracetamol or, if appropriate, non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen. NSAIDs should be used with caution, particularly in patients with diabetes who may have renal impairment, cardiovascular disease, or gastrointestinal risk factors. Patients should consult their GP or pharmacist before using NSAIDs, especially if they have hypertension, heart failure, kidney disease, or are taking medications such as ACE inhibitors or diuretics.
If muscle pain is thought to be related to rapid weight loss or nutritional factors, working with a dietitian or diabetes specialist nurse to optimise dietary intake may be beneficial. Supplementation (e.g., vitamin D) should only be considered if deficiency is confirmed through testing. Regular monitoring of weight loss trajectory and adjusting expectations to a more gradual pace can also reduce musculoskeletal strain.
In some cases, dose adjustment of Mounjaro may be considered, but this must only be done in consultation with the prescribing clinician. Slowing the titration schedule or temporarily maintaining a lower dose may allow the body more time to adapt, potentially reducing side effects including muscle discomfort.
Patients should be encouraged to maintain open communication with their healthcare team, reporting any new or worsening symptoms promptly to ensure timely intervention and support.
While mild, transient muscle discomfort may not require immediate medical attention, certain red flag symptoms warrant prompt evaluation by a healthcare professional. Patients taking Mounjaro should be advised to contact their GP or diabetes specialist if they experience:
Severe or worsening muscle pain that does not improve with rest or simple analgesia
Muscle weakness, particularly if it affects daily activities or mobility
Dark or tea-coloured urine, which may indicate rhabdomyolysis (a serious condition involving muscle breakdown)
Swelling, tenderness, or warmth in a specific muscle group, which could suggest injury or inflammation
Systemic symptoms such as fever, unexplained weight loss, night sweats, or profound fatigue
Persistent pain lasting more than a few weeks without clear cause or improvement
Rhabdomyolysis, though rare, is a medical emergency characterised by the breakdown of muscle tissue and release of muscle proteins into the bloodstream, potentially leading to kidney damage. Symptoms include severe muscle pain, weakness, and dark urine. If severe muscle pain occurs with dark urine, confusion, or collapse, patients should call 999 or go to A&E immediately. Any suspicion of this condition requires urgent assessment, including blood tests to measure creatine kinase levels and renal function.
For urgent advice when GP services are unavailable, patients should contact NHS 111.
Patients should also seek advice if muscle pain is accompanied by signs of hypoglycaemia (sweating, tremor, confusion, palpitations) or other concerning side effects of Mounjaro, such as severe abdominal pain, persistent vomiting, or signs of pancreatitis.
For those with pre-existing musculoskeletal or metabolic conditions (e.g., statin-induced myopathy, hypothyroidism, inflammatory arthritis), closer monitoring and earlier medical review may be appropriate. Collaborative care involving the GP, diabetes team, and, where necessary, rheumatology or neurology services ensures comprehensive assessment and management.
Patients are encouraged to report suspected side effects to the MHRA through the Yellow Card scheme, which helps monitor the safety of medicines after they have been licensed.
Ultimately, patient safety is paramount. When in doubt, individuals should err on the side of caution and seek professional guidance to ensure that muscle pain is appropriately evaluated and managed, allowing them to continue their treatment safely and effectively.
Muscle pain is not listed among the most common side effects of Mounjaro in the MHRA-approved Summary of Product Characteristics. Clinical trials documented musculoskeletal complaints at relatively low frequencies, comparable to comparator groups.
For mild muscle discomfort, ensure adequate hydration, balanced nutrition, and gentle physical activity. If pain is severe, worsening, or accompanied by weakness or dark urine, contact your GP or diabetes specialist promptly for assessment.
Significant weight loss may lead to changes in body composition, including some loss of lean mass, which can result in muscle adaptation and discomfort. Metabolic shifts and altered physical activity patterns may also contribute to musculoskeletal symptoms.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.