Does Ozempic cause bruising? Ozempic (semaglutide) is a GLP-1 receptor agonist used to treat type 2 diabetes mellitus in the UK. Whilst bruising is not listed as a common side effect in the Summary of Product Characteristics, some patients experience localised bruising at injection sites. This typically results from the injection process itself rather than a direct effect of semaglutide. Understanding why bruising occurs and how to minimise it can help patients manage their treatment confidently. This article examines the causes of injection-site bruising, practical prevention strategies, and when to seek medical advice.
Quick Answer: Ozempic does not directly cause bruising, but localised bruising at injection sites can occur due to minor blood vessel damage during subcutaneous injection.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Administered as a once-weekly subcutaneous injection, Ozempic is prescribed across NHS and private healthcare settings. While bruising is not specifically listed as a common adverse effect in the Summary of Product Characteristics (SmPC), injection-site reactions are reported, and some patients experience localised bruising at injection sites.
Bruising associated with Ozempic is typically mild and transient, occurring as a result of the injection process itself rather than a direct pharmacological effect of semaglutide. When a needle penetrates the skin and subcutaneous tissue, small blood vessels (capillaries) may be damaged, leading to localised bleeding under the skin that manifests as a bruise (ecchymosis). This is a recognised phenomenon with any subcutaneous injection and is not unique to Ozempic.
It is important to distinguish between injection-site bruising and more widespread or unexplained bruising, which may indicate an underlying haematological disorder or interaction with anticoagulant or antiplatelet medications. If you experience bruising beyond the injection site, bruising that does not resolve within a week or two, or bruising accompanied by other symptoms such as prolonged bleeding, petechiae (small red or purple spots), or unusual fatigue, you should contact your GP or healthcare provider promptly. There is no established association in the UK product information between semaglutide and systemic bleeding disorders, but any new or concerning symptoms warrant clinical review.
If you suspect an adverse reaction to Ozempic, you can report it via the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk.
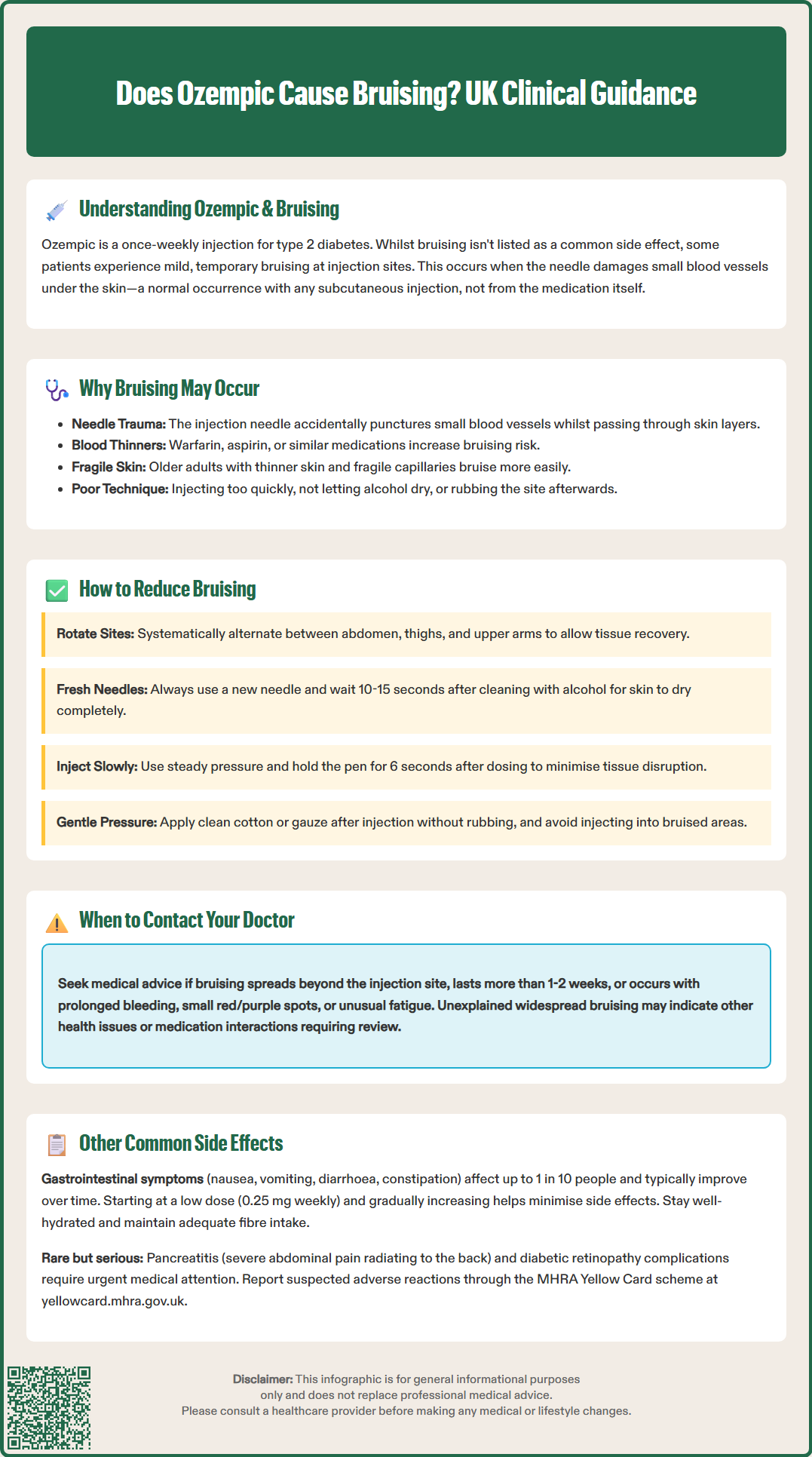
Understanding the mechanism behind injection-site bruising can help patients manage expectations and adopt preventive strategies. Ozempic is delivered via a pre-filled pen into the subcutaneous tissue of the abdomen, thigh, or upper arm. The needle must pass through the epidermis, dermis, and into the subcutaneous fat layer. During this process, it is possible to inadvertently puncture a small blood vessel, causing localised bleeding and subsequent bruising.
Several patient-specific factors may increase the likelihood of bruising. Individuals taking anticoagulant medications (such as warfarin, apixaban, or rivaroxaban) or antiplatelet agents (such as aspirin or clopidogrel) are at higher risk due to impaired clotting mechanisms. Older adults often have thinner skin and more fragile capillaries, making bruising more common. Additionally, patients with conditions affecting connective tissue or those with a history of easy bruising may be more susceptible.
Injection technique also plays a significant role. Injecting too quickly, failing to allow the skin to dry after cleansing with alcohol, or reusing needles can all contribute to tissue trauma and bruising. Injecting into areas with less subcutaneous fat or into muscle rather than fat may increase discomfort and bruising. Furthermore, massaging or rubbing the injection site immediately after administration can exacerbate bleeding under the skin.
It is worth noting that bruising does not indicate reduced efficacy of Ozempic. The medication is absorbed systemically regardless of minor localised bruising, and patients should continue their prescribed regimen unless advised otherwise by their healthcare provider. Avoid injecting into bruised, inflamed, or scarred areas, and apply gentle, sustained pressure after injection, particularly if you take blood-thinning medications.
Adopting best-practice injection techniques can significantly reduce the incidence and severity of bruising. The following strategies align with recommendations from FIT UK (Forum for Injection Technique) and Diabetes UK:
Rotate injection sites systematically: Avoid injecting into the same area repeatedly. Use a rotation pattern across the abdomen, thighs, and upper arms to allow tissues to recover and reduce cumulative trauma.
Allow alcohol to dry completely: After cleansing the skin with an alcohol wipe, wait at least 10–15 seconds for the area to dry. Injecting through wet skin can increase stinging and tissue irritation.
Use a fresh needle for each injection: Never reuse needles. Blunt or damaged needles cause more tissue trauma and increase the risk of bruising and infection.
Inject slowly and steadily: Rapid injection can cause more tissue disruption. Depress the pen button smoothly and hold for 6 seconds after the dose counter returns to 0, as instructed in the Ozempic Patient Information Leaflet.
Apply gentle pressure after injection: After withdrawing the needle, apply gentle pressure with a clean cotton pad or gauze if needed, but do not rub or massage the area.
Use appropriate needle length: FIT UK recommends 4 mm pen needles for most adults. A skinfold is generally not needed with 4 mm needles but may be considered in very lean individuals to avoid intramuscular injection.
Avoid injecting into damaged skin: Do not inject into bruised, inflamed, or scarred areas as this may increase discomfort and affect absorption.
If you take anticoagulant or antiplatelet medication and experience excessive bruising, consult your healthcare provider. Never stop these medications without medical advice.
If bruising persists despite these measures, or if you have concerns about your injection technique, request a review with a diabetes specialist nurse or practice nurse. Many NHS diabetes services offer injection technique assessments and can provide personalised guidance.
Beyond injection-site reactions, Ozempic is associated with a range of gastrointestinal side effects, which are the most commonly reported adverse reactions. These occur because semaglutide slows gastric emptying and affects gut motility as part of its mechanism of action. According to the SmPC, the most frequent side effects include:
Nausea: Very common (may affect more than 1 in 10 people), particularly during dose initiation or escalation. This typically improves over several weeks as the body adjusts.
Vomiting and diarrhoea: Common (may affect up to 1 in 10 people). Staying well-hydrated is important, especially if experiencing severe or persistent symptoms.
Constipation: Common (may affect up to 1 in 10 people). Adequate fluid intake and dietary fibre are important.
Abdominal pain and dyspepsia: Common (may affect up to 1 in 10 people). Discomfort in the upper abdomen or indigestion-like symptoms may occur.
These gastrointestinal effects are usually dose-dependent and tend to diminish with continued use. The Ozempic SmPC recommends starting at 0.25 mg weekly for 4 weeks (for tolerability), then increasing to 0.5 mg weekly, with further escalation as clinically indicated.
Hypoglycaemia (low blood sugar) is uncommon with Ozempic monotherapy, as GLP-1 receptor agonists have a glucose-dependent mechanism. However, when used in combination with insulin or sulfonylureas, the risk increases, and dose adjustments of these medications may be necessary.
Rare but serious adverse effects include pancreatitis (severe, persistent abdominal pain radiating to the back). If pancreatitis is suspected, stop taking Ozempic and seek urgent medical assessment. Diabetic retinopathy complications may occur, particularly in patients with pre-existing retinopathy when glycaemic control improves rapidly. Regular eye screening is important, especially during treatment intensification.
In animal studies, semaglutide caused thyroid C-cell tumours, though the clinical relevance in humans is unknown. Patients should report any symptoms such as a lump in the neck, hoarseness, difficulty swallowing, or shortness of breath.
Patients should be advised to seek urgent medical attention if they experience severe abdominal pain, persistent vomiting, signs of pancreatitis, or visual changes. Routine monitoring as per NICE guidelines for type 2 diabetes should continue, including HbA1c, renal function, and cardiovascular risk assessment.
Report any suspected adverse reactions to Ozempic via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Yes, mild localised bruising at injection sites is a recognised occurrence with subcutaneous injections and results from minor blood vessel damage during needle insertion. It is typically transient and does not affect the efficacy of Ozempic.
Rotate injection sites systematically, use a fresh needle each time, allow alcohol to dry completely before injecting, inject slowly, and apply gentle pressure afterwards without rubbing. These techniques significantly reduce bruising risk.
Contact your GP if you experience widespread bruising beyond injection sites, bruising that does not resolve within one to two weeks, or bruising accompanied by prolonged bleeding, petechiae, or unusual fatigue, as these may indicate an underlying condition.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.