Does tirzepatide burn belly fat? Tirzepatide is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes management, with emerging evidence supporting substantial weight loss. Whilst clinical trials demonstrate significant reductions in total body fat—including visceral abdominal fat—tirzepatide does not selectively target belly fat through a unique mechanism. Rather, it facilitates overall fat loss by suppressing appetite, enhancing satiety, and regulating metabolism. This article examines the clinical evidence, expected outcomes, eligibility criteria, and the importance of combining tirzepatide with lifestyle modifications for optimal results.
Quick Answer: Tirzepatide does not selectively burn belly fat, but clinical trials show it produces significant overall fat loss, including substantial reductions in visceral abdominal fat through appetite suppression and metabolic regulation.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereTirzepatide is a novel injectable medication approved in the UK for the treatment of type 2 diabetes (marketed as Mounjaro). In some countries, it has also received approval for chronic weight management in adults with obesity or overweight with weight-related comorbidities (marketed as Zepbound in some jurisdictions).
The drug functions as a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist. This dual mechanism distinguishes tirzepatide from earlier GLP-1 receptor agonists like semaglutide. By activating both GIP and GLP-1 receptors, tirzepatide enhances insulin secretion in response to meals, suppresses glucagon release (which reduces glucose production by the liver), and significantly slows gastric emptying. These actions collectively improve glycaemic control in people with diabetes.
For weight management, tirzepatide acts on appetite-regulating centres in the brain, particularly the hypothalamus, leading to reduced hunger and increased satiety. Patients typically report feeling fuller for longer periods and experiencing fewer food cravings. The medication is administered once weekly via subcutaneous injection, with doses gradually titrated upwards to minimise gastrointestinal side effects. The starting dose of 2.5 mg is used for tolerability and is not considered therapeutic; clinical effect is achieved after up-titration.
In the UK, tirzepatide is regulated by the Medicines and Healthcare products Regulatory Agency (MHRA) and prescribing guidance is informed by the National Institute for Health and Care Excellence (NICE). It is important to note that tirzepatide should not be used concurrently with other GLP-1 receptor agonists.
Patients should be aware that tirzepatide's effect on delaying gastric emptying can reduce the effectiveness of oral contraceptives. Women using oral contraceptives should use additional barrier contraception for 4 weeks after starting tirzepatide and after each dose increase, or consider switching to non-oral contraceptive methods.
While the medication has demonstrated substantial weight loss in clinical trials, it is important to understand that tirzepatide is not specifically a "fat-burning" agent in the traditional sense, but rather works through appetite suppression and metabolic regulation.
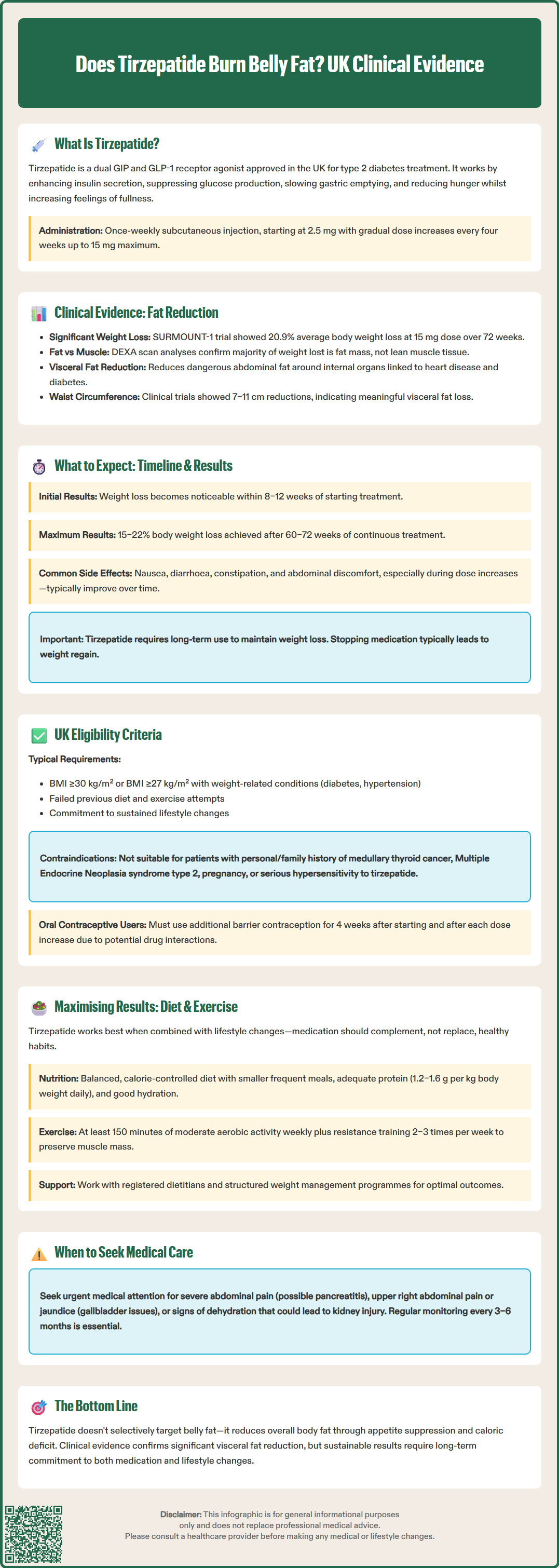
Robust clinical trial data demonstrate that tirzepatide produces significant reductions in total body weight, with evidence suggesting preferential loss of fat mass, including visceral (abdominal) fat. The landmark SURMOUNT clinical trial programme has provided the most comprehensive evidence to date.
In the SURMOUNT-1 trial, published in the New England Journal of Medicine, participants without diabetes but with obesity received tirzepatide at varying doses (5 mg, 10 mg, or 15 mg weekly) or placebo, alongside lifestyle interventions. At 72 weeks, those on the highest dose achieved an average weight loss of 20.9% of their initial body weight, compared to 3.1% with placebo. Importantly, body composition analyses using dual-energy X-ray absorptiometry (DEXA) scans revealed that the majority of weight lost was fat mass rather than lean muscle tissue.
Regarding visceral adipose tissue specifically—the metabolically active fat stored around internal organs in the abdominal cavity—studies have shown meaningful reductions. Visceral fat is particularly associated with cardiovascular disease, type 2 diabetes, and metabolic syndrome. While tirzepatide does not selectively "target" belly fat through a unique mechanism, the substantial overall fat loss naturally includes significant reductions in abdominal adiposity.
A sub-analysis of the SURPASS trials (focused on type 2 diabetes management) demonstrated reductions in waist circumference averaging 7–11 cm across different doses, serving as a proxy measure for visceral fat reduction. However, it is essential to note that there is no official evidence that tirzepatide preferentially burns belly fat over fat in other body regions. Rather, it facilitates overall fat loss through caloric deficit induced by appetite suppression, and the distribution of fat loss follows typical patterns seen with substantial weight reduction.
Patients considering tirzepatide for weight management should have realistic expectations about the timeline and magnitude of results. Weight loss with tirzepatide is gradual and progressive, not immediate, with most significant changes occurring over several months.
In clinical trials, meaningful weight loss typically becomes apparent within the first 8–12 weeks of treatment, with continued progression throughout the first year. The dose is usually started at 2.5 mg weekly and increased every four weeks (2.5 mg → 5 mg → 7.5 mg → 10 mg → 12.5 mg → 15 mg) based on tolerability and response. Maximum weight loss is generally achieved between 60–72 weeks of continuous treatment.
Expected outcomes based on clinical trial data include:
Average weight loss of 15–22% of initial body weight at maximum doses
Approximately 1–2 kg loss per month during the active weight loss phase (individual results may vary)
Reductions in waist circumference of 7–12 cm on average
Improvements in metabolic markers (HbA1c, blood pressure, lipid profiles)
Individual responses vary considerably. Factors influencing outcomes include baseline weight, adherence to lifestyle modifications, dose achieved, genetic factors, and concurrent medications. Some patients may experience more modest results (10–12% weight loss), whilst others achieve losses exceeding 25%.
Common side effects, particularly during dose escalation, include nausea, diarrhoea, constipation, vomiting, and abdominal discomfort. These are usually mild to moderate and diminish over time. More serious side effects to be aware of include:
Severe, persistent abdominal pain (with or without vomiting) – seek urgent medical care as this could indicate acute pancreatitis
Upper right abdominal pain or jaundice – may indicate gallbladder disease
Risk of dehydration – maintain adequate fluid intake to reduce risk of acute kidney injury
Potential worsening of diabetic retinopathy in those with pre-existing condition
Increased risk of hypoglycaemia when used with insulin or sulfonylureas (dose adjustments may be needed)
Patients should inform surgical and anaesthetic teams about tirzepatide use due to its effect on gastric emptying, which may increase aspiration risk during procedures.
Weight loss may plateau after the first year, and maintaining results requires ongoing treatment combined with sustained lifestyle changes. Discontinuation of tirzepatide typically results in weight regain, emphasising that this is a long-term therapeutic intervention rather than a short-term solution.
Patients are encouraged to report any suspected side effects to the MHRA Yellow Card Scheme.
In the UK, tirzepatide (Mounjaro) is currently licensed by the MHRA for the treatment of type 2 diabetes. The regulatory status for weight management should be confirmed at the time of reading, as approvals may have changed. NHS funding and access are determined by NICE guidance, which may differ from the licensed indications.
If approved for weight management, general eligibility criteria would typically include:
Body Mass Index (BMI) ≥30 kg/m² (obesity), or
BMI ≥27 kg/m² (overweight) with at least one weight-related comorbidity such as type 2 diabetes, hypertension, dyslipidaemia, obstructive sleep apnoea, or cardiovascular disease
Age 18 years or older
Previous unsuccessful attempts at weight loss through diet and exercise alone
Commitment to a comprehensive weight management programme including dietary modification and increased physical activity
NICE guidance may specify lower BMI thresholds for certain ethnic groups (particularly those of South Asian origin) who are at increased risk of complications at lower BMI levels.
Important safety considerations include:
Caution in patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 (patients should be counselled about thyroid symptoms)
Previous serious hypersensitivity to tirzepatide
Pregnancy or breastfeeding (effective contraception required in women of childbearing potential)
Caution in patients with gastrointestinal disease, particularly severe gastroparesis
History of pancreatitis (requires careful assessment)
Women using oral contraceptives should use additional barrier contraception for 4 weeks after starting tirzepatide and after each dose increase, or consider non-oral contraceptive methods
In the UK, tirzepatide for weight management may be available through private prescription, while NHS availability would depend on NICE guidance and local commissioning decisions. Access through the NHS would typically be via specialist weight management services (tier 3 or 4).
Patients should undergo comprehensive assessment by a qualified healthcare professional, including baseline investigations (HbA1c, lipid profile, liver and kidney function, thyroid function) and screening for contraindications. Regular monitoring is essential, with review appointments typically scheduled every 3–6 months to assess response, tolerability, and ongoing appropriateness of treatment. Treatment should be discontinued if inadequate response is observed, with specific criteria likely defined in NICE guidance.
Whilst tirzepatide is highly effective as a pharmacological intervention, optimal outcomes are achieved when medication is combined with comprehensive lifestyle modifications. The medication should be viewed as an adjunct to, not a replacement for, healthy eating patterns and regular physical activity.
Dietary recommendations for patients on tirzepatide include:
Balanced, calorie-controlled diet: Focus on nutrient-dense whole foods including vegetables, fruits, lean proteins, whole grains, and healthy fats
Smaller, more frequent meals: This approach may help manage the gastrointestinal side effects and work synergistically with the medication's effect on satiety
Adequate protein intake: Aim for 1.2–1.6 g per kg of body weight daily to preserve lean muscle mass during weight loss (individualised advice from a dietitian is recommended)
Hydration: Maintain good fluid intake, particularly important given potential gastrointestinal side effects
Limiting ultra-processed foods: Reduce consumption of foods high in added sugars, saturated fats, and sodium
Low-fat meals: Particularly helpful for reducing gastrointestinal symptoms
Physical activity guidance includes:
Aerobic exercise: Aim for at least 150 minutes of moderate-intensity activity (brisk walking, cycling, swimming) per week, as recommended by UK Chief Medical Officers
Resistance training: Include strength-building exercises 2–3 times weekly to maintain muscle mass and metabolic rate
Gradual progression: Start at a comfortable level and progressively increase intensity and duration
Incorporate movement throughout the day: Reduce sedentary time with regular activity breaks
Behavioural support is equally important. Consider:
Working with a registered dietitian for personalised nutrition guidance
Engaging with structured weight management programmes (available through some NHS services or privately)
Addressing psychological factors such as emotional eating, stress management, and sleep quality
Setting realistic, achievable goals with regular self-monitoring
Patients should be advised that sustainable weight management requires long-term commitment. The combination of tirzepatide with lifestyle interventions produces superior outcomes compared to either approach alone, with better maintenance of weight loss and improvements in overall metabolic health. Regular follow-up with healthcare professionals ensures ongoing support, monitoring for adverse effects, and adjustment of the treatment plan as needed.
Meaningful weight loss typically becomes apparent within the first 8–12 weeks of treatment, with continued progression throughout the first year. Maximum weight loss is generally achieved between 60–72 weeks of continuous treatment, with doses gradually titrated upwards every four weeks.
Tirzepatide is not indicated solely for cosmetic fat reduction. In the UK, it is licensed for type 2 diabetes management, with eligibility for weight management typically requiring BMI ≥30 kg/m² or BMI ≥27 kg/m² with weight-related comorbidities, alongside commitment to comprehensive lifestyle modifications.
Discontinuation of tirzepatide typically results in weight regain, emphasising that this is a long-term therapeutic intervention rather than a short-term solution. Maintaining results requires ongoing treatment combined with sustained lifestyle changes including healthy eating patterns and regular physical activity.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.