Tirzepatide (Mounjaro) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for type 2 diabetes mellitus and chronic weight management. Many patients wonder whether tirzepatide speeds up metabolism, particularly given the substantial weight loss observed in clinical trials. Understanding how this medication affects metabolic processes is essential for setting realistic expectations. This article examines the evidence on tirzepatide's metabolic effects, clarifies common misconceptions about metabolic rate, and explains what patients can expect during treatment.
Quick Answer: Tirzepatide does not directly speed up basal metabolic rate but influences metabolism through multiple pathways including enhanced insulin sensitivity, reduced appetite, and slowed gastric emptying.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereTirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus and, more recently, for chronic weight management in adults with obesity or overweight with weight-related comorbidities. In the UK, tirzepatide is marketed under the brand name Mounjaro for both indications, representing an important addition to metabolic therapeutics due to its dual incretin receptor activity.
The mechanism of action involves binding to both GIP and GLP-1 receptors, which are naturally occurring hormones released from the gut in response to food intake. GLP-1 receptor activation enhances glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriate glucagon release, slows gastric emptying, and reduces appetite through central nervous system pathways. GIP receptor activation complements these effects by further enhancing insulin secretion and may influence fat metabolism, though the precise mechanisms remain under investigation.
Administered as a once-weekly subcutaneous injection, tirzepatide is typically initiated at a low dose (2.5 mg) for tolerability and gradually titrated upwards over several weeks to minimise gastrointestinal side effects. The 2.5 mg dose is for initiation only and not intended for glycaemic control. The maximum licensed dose is up to 15 mg weekly for both type 2 diabetes and weight management, though some patients may require lower maintenance doses. The MHRA approved tirzepatide following clinical trial data demonstrating improvements in glycaemic control and substantial weight reduction compared to placebo and other diabetes medications.
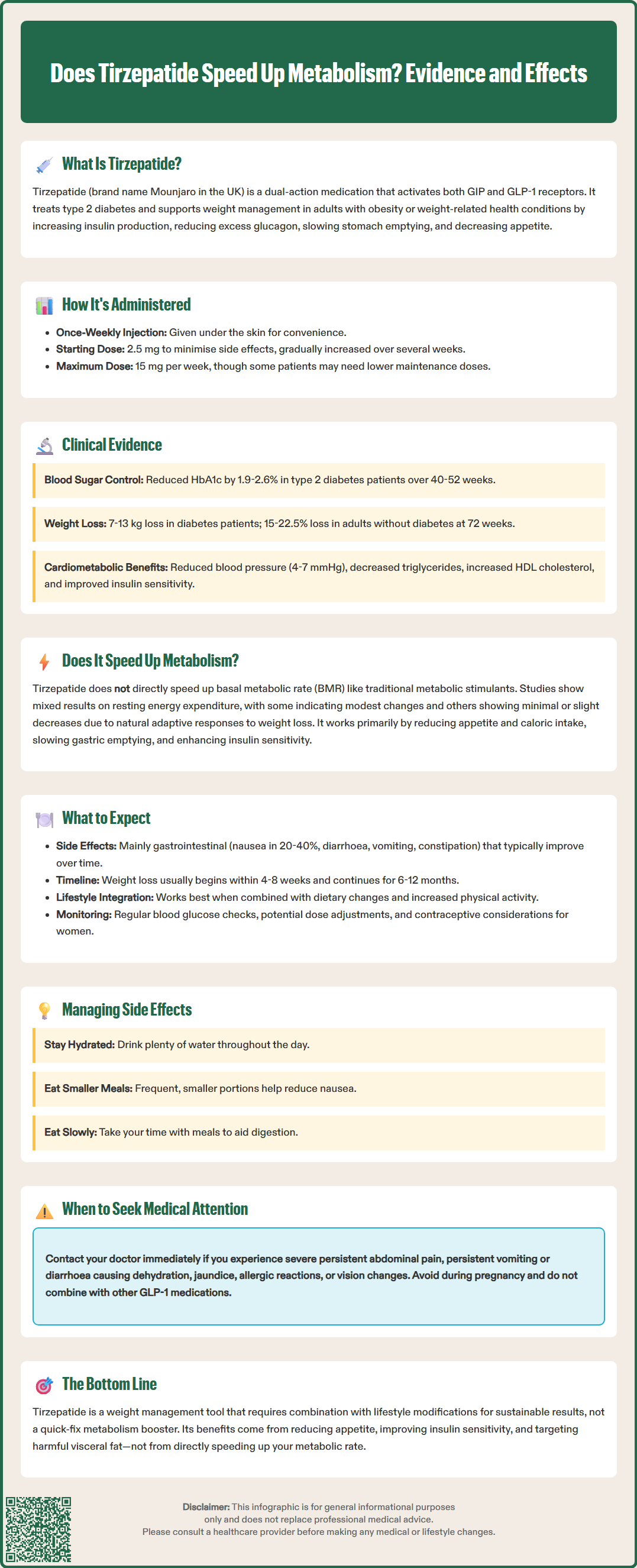
Extensive clinical trial programmes, including the SURPASS and SURMOUNT studies, have documented tirzepatide's effects on multiple metabolic parameters. In the SURPASS trials involving patients with type 2 diabetes, tirzepatide demonstrated superior HbA1c reductions (ranging from 1.9% to 2.6% [21-28 mmol/mol] depending on dose) compared to placebo, semaglutide, and insulin glargine. Concurrently, participants experienced substantial weight loss, with reductions of 7–13 kg observed across different doses over 40–52 weeks.
The SURMOUNT trials specifically examined tirzepatide's efficacy in weight management among adults without diabetes. SURMOUNT-1 reported mean weight reductions of 15–22.5% from baseline at 72 weeks, significantly exceeding placebo responses. These outcomes were accompanied by improvements in cardiometabolic risk factors, including reductions in systolic blood pressure (4–7 mmHg), improvements in lipid profiles (decreased triglycerides, increased HDL cholesterol), and enhanced insulin sensitivity markers.
Metabolic assessments within these trials suggest that tirzepatide influences several physiological processes beyond simple caloric restriction. Some studies have observed changes in resting energy expenditure in participants, though the magnitude varies considerably between individuals and findings are inconsistent. Research using imaging techniques has shown that tirzepatide treatment is associated with reductions in visceral adipose tissue—the metabolically harmful fat surrounding internal organs—which may contribute to improved insulin sensitivity.
The metabolic benefits observed appear to extend beyond weight loss alone. Even accounting for the degree of weight reduction, tirzepatide demonstrates improvements in glycaemic control and insulin sensitivity, suggesting effects mediated through its dual incretin receptor activity. However, researchers continue to investigate the precise mechanisms underlying these broader metabolic improvements.
Patients initiating tirzepatide should be prepared for a gradual dose escalation protocol designed to optimise tolerability. Treatment typically begins with 2.5 mg weekly for four weeks, followed by incremental increases every four weeks until reaching the target maintenance dose or the maximum tolerated dose. This titration schedule helps minimise the most common adverse effects, which are predominantly gastrointestinal in nature.
Common side effects include nausea (reported in 20–40% of patients, depending on dose), diarrhoea, vomiting, constipation, abdominal discomfort, and reduced appetite. These symptoms are usually most pronounced during dose escalation and tend to diminish over time as the body adapts. Staying well-hydrated, eating smaller, more frequent meals, and eating slowly can help manage these effects. If gastrointestinal symptoms become severe or persistent, patients should contact their GP or diabetes specialist, as dose adjustment may be necessary.
Weight loss typically becomes noticeable within the first 4–8 weeks of treatment, with progressive reductions continuing over 6–12 months. The rate and extent of weight loss vary considerably between individuals, influenced by factors including baseline weight, adherence to lifestyle modifications, dose achieved, and individual metabolic responses. Patients should be counselled that tirzepatide is most effective when combined with dietary modifications and increased physical activity, as recommended in NICE guidance.
Regular monitoring is essential during tirzepatide therapy. For patients with diabetes, blood glucose levels should be checked as advised by the healthcare team. Doses of insulin or sulfonylureas may need to be reduced when initiating or increasing tirzepatide to prevent hypoglycaemia. Blood pressure and heart rate should be monitored periodically. Women using oral hormonal contraceptives should use an additional barrier method for 4 weeks after initiation and after each dose increase.
Patients should seek medical attention if they experience severe or persistent abdominal pain (which could indicate pancreatitis or gallbladder disease), persistent vomiting or diarrhoea leading to dehydration, jaundice, or signs of allergic reaction. Any visual changes should prompt prompt assessment by an ophthalmologist or diabetes team, particularly in patients with pre-existing diabetic retinopathy. Tirzepatide should not be used during pregnancy, and concurrent use with other GLP-1 receptor agonists is not recommended. Patients should report suspected side effects via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
The question of whether tirzepatide directly "speeds up metabolism" requires careful interpretation of what metabolism encompasses and what the current evidence demonstrates. In common usage, "speeding up metabolism" typically refers to increasing the basal metabolic rate (BMR)—the energy expended at rest to maintain vital bodily functions. The scientific evidence suggests that tirzepatide's metabolic effects are more nuanced than simply accelerating metabolic rate.
Resting energy expenditure studies have produced mixed findings. Some research indicates modest changes in resting metabolic rate among tirzepatide users, whilst other studies show minimal changes or even slight decreases—a typical adaptive response to significant weight loss. When substantial weight is lost through any means, the body often reduces energy expenditure as a compensatory mechanism, making further weight loss more challenging. Whether tirzepatide might affect this metabolic adaptation differently from other weight loss methods remains an area of active investigation, with limited conclusive evidence currently available.
More accurately, tirzepatide appears to affect metabolism through multiple pathways. It enhances insulin sensitivity, allowing cells to utilise glucose more effectively. It influences appetite-regulating hormones and neural pathways, reducing caloric intake. The medication slows gastric emptying, which affects nutrient absorption timing. Additionally, the dual GIP/GLP-1 receptor activation may influence lipid metabolism, though the clinical significance of these effects requires further clarification.
There is no established evidence suggesting that tirzepatide functions as a traditional metabolic stimulant like thyroid hormones or sympathomimetic agents. Rather, it works primarily by reducing appetite and caloric intake, slowing gastric emptying, and improving the body's metabolic response to nutrients. The resulting weight loss and improved insulin sensitivity then contribute to broader metabolic improvements. Patients should understand that tirzepatide is not a "quick fix" but rather a tool that, when combined with lifestyle modifications, facilitates sustainable metabolic improvements and weight management. Any concerns about metabolic effects or treatment response should be discussed with a prescribing clinician who can provide personalised guidance based on individual circumstances and monitoring results.
Tirzepatide does not consistently increase basal metabolic rate. Studies show mixed findings on resting energy expenditure, with the medication working primarily through appetite reduction, slowed gastric emptying, and improved insulin sensitivity rather than directly accelerating metabolism.
Weight loss typically becomes noticeable within 4–8 weeks of starting tirzepatide, with progressive reductions continuing over 6–12 months. The rate varies between individuals and is most effective when combined with dietary modifications and increased physical activity.
The most common side effects are gastrointestinal, including nausea (20–40% of patients), diarrhoea, vomiting, constipation, and abdominal discomfort. These symptoms are usually most pronounced during dose escalation and tend to diminish over time as the body adapts.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.