Wegovy (semaglutide 2.4 mg) is a GLP-1 receptor agonist licensed in the UK for chronic weight management in adults with obesity or overweight with weight-related comorbidities. Many patients and healthcare professionals ask: does Wegovy cause hypoglycaemia? Understanding the medication's glucose-dependent mechanism and associated risk factors is essential for safe prescribing and patient counselling. This article examines the hypoglycaemic potential of Wegovy, identifies at-risk populations, and provides practical guidance aligned with NICE, MHRA, and NHS recommendations for monitoring and managing low blood sugar during treatment.
Quick Answer: Wegovy has a low intrinsic risk of causing hypoglycaemia when used alone, but the risk increases significantly when combined with insulin or sulphonylureas.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWegovy (semaglutide 2.4 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for chronic weight management in adults with obesity or overweight with weight-related comorbidities. The Medicines and Healthcare products Regulatory Agency (MHRA) approved Wegovy following clinical trials demonstrating significant weight reduction when combined with lifestyle interventions.
In the UK, NICE Technology Appraisal 875 recommends semaglutide for adults with at least one weight-related comorbidity who have a BMI of at least 35 kg/m² (or at least 30 kg/m² in exceptional circumstances). Treatment should be initiated and supervised within specialist weight management services and is typically recommended for a maximum of 2 years.
The mechanism of action of semaglutide involves mimicking the naturally occurring hormone GLP-1, which is released from the intestine after eating. GLP-1 receptor agonists work by:
Stimulating insulin secretion from pancreatic beta cells in a glucose-dependent manner
Suppressing glucagon release when blood glucose levels are elevated
Slowing gastric emptying, which moderates post-meal glucose rises (this effect may attenuate over time)
Reducing appetite through effects on brain centres controlling satiety
This glucose-dependent mechanism is clinically significant because insulin secretion is only enhanced when blood glucose levels are elevated. When glucose levels fall towards or below normal range, the insulinotropic effect diminishes substantially. This inherent safety feature distinguishes GLP-1 receptor agonists from some other glucose-lowering medications, such as sulphonylureas or insulin itself, which can stimulate insulin release regardless of prevailing glucose concentrations.
Understanding this pharmacological profile is essential when considering the hypoglycaemic potential of Wegovy. The medication's effects on blood sugar regulation are fundamentally different from those of traditional diabetes medications, which has important implications for patients and healthcare professionals assessing the risk of low blood sugar episodes during treatment.
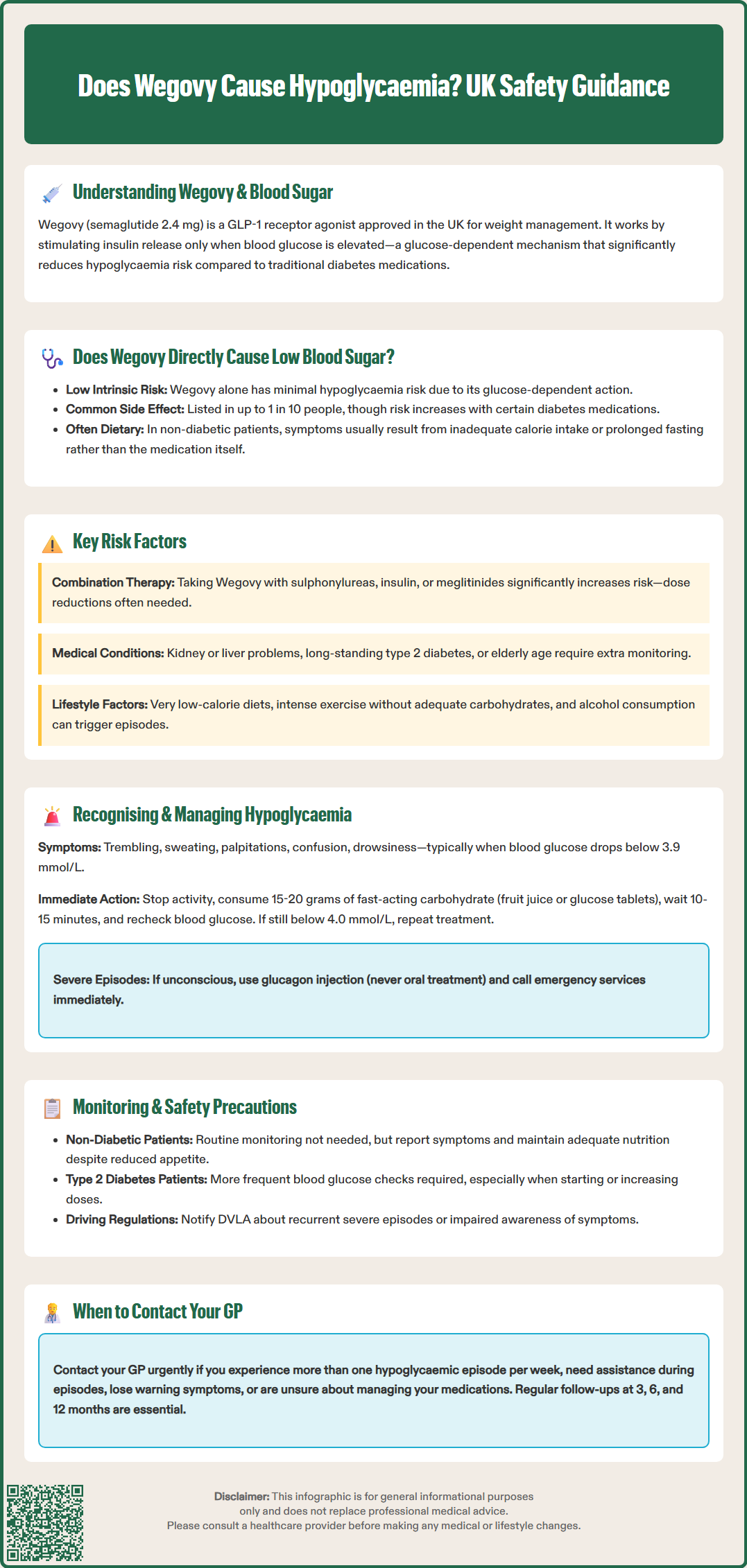
When used as monotherapy (on its own, without other glucose-lowering medications), Wegovy has a low intrinsic risk of causing hypoglycaemia. However, according to the Wegovy Summary of Product Characteristics (SmPC), hypoglycaemia is listed as a common adverse reaction (affecting up to 1 in 10 people) even in people without diabetes.
The glucose-dependent mechanism of GLP-1 receptor agonists means that as blood glucose approaches normal physiological levels (typically 4.0–5.5 mmol/L fasting), the medication's effect on insulin secretion naturally diminishes. This built-in safety mechanism substantially reduces the likelihood of blood glucose falling into hypoglycaemic ranges (generally defined as below 3.9 mmol/L, though symptomatic thresholds vary between individuals).
Clinical trial data from the STEP programme, as reviewed by the European Medicines Agency (EMA), showed that while hypoglycaemia can occur with Wegovy monotherapy, the risk is significantly higher when combined with insulin or insulin secretagogues. NHS patient information confirms that hypoglycaemia can occur as a side effect of semaglutide even in people without diabetes.
It is important to distinguish between:
Biochemical hypoglycaemia – laboratory-confirmed low blood glucose
Symptomatic hypoglycaemia – symptoms such as tremor, sweating, or confusion with or without confirmed low glucose
Severe hypoglycaemia – requiring third-party assistance
In weight management populations without diabetes, reports of hypoglycaemia-like symptoms are relatively uncommon and often relate to inadequate caloric intake, prolonged fasting, or increased physical activity rather than direct drug effects alone. Patients experiencing such symptoms should be carefully assessed, as they may reflect dietary factors or other medical conditions rather than true drug-induced hypoglycaemia.
Whilst Wegovy alone carries a low hypoglycaemia risk, certain clinical scenarios significantly increase vulnerability to low blood sugar episodes:
Concomitant diabetes medications represent the most important risk factor. Patients taking Wegovy alongside:
Sulphonylureas (e.g., gliclazide, glimepiride) – these stimulate insulin release independent of glucose levels
Insulin therapy – exogenous insulin administration can cause hypoglycaemia regardless of endogenous glucose regulation
Meglitinides (e.g., repaglinide) – short-acting insulin secretagogues
When GLP-1 receptor agonists are combined with these medications, the risk of hypoglycaemia increases substantially. NICE guidance (NG28) on type 2 diabetes management recommends dose reduction of sulphonylureas or insulin when initiating GLP-1 receptor agonist therapy to mitigate this risk.
Additional risk factors include:
Type 2 diabetes with impaired counter-regulatory responses – long-standing diabetes may blunt the body's natural protective mechanisms against hypoglycaemia
Renal impairment – reduced kidney function can affect drug clearance and alter glucose homeostasis, particularly if on insulin or sulphonylureas
Hepatic dysfunction – the liver plays a central role in glucose production and metabolism
Excessive caloric restriction – very low-calorie diets combined with Wegovy may precipitate symptoms mimicking hypoglycaemia
Increased physical activity – particularly unplanned or intense exercise without adequate carbohydrate intake
Alcohol consumption – alcohol inhibits hepatic glucose production and can mask hypoglycaemia symptoms
Elderly patients – may have reduced awareness of hypoglycaemic symptoms and altered drug metabolism
According to the Wegovy SmPC, patients with type 1 diabetes should not use Wegovy, as it is not licensed for this indication and the complex insulin requirements make management challenging. Healthcare professionals should conduct thorough medication reviews before prescribing Wegovy, particularly scrutinising all glucose-lowering therapies.
Early recognition of hypoglycaemia is crucial for prompt management and prevention of progression to severe episodes. Symptoms typically emerge when blood glucose falls below 3.9 mmol/L, though individual thresholds vary.
Common symptoms of hypoglycaemia include:
Autonomic symptoms – trembling, sweating, palpitations, hunger, anxiety
Neuroglycopenic symptoms – difficulty concentrating, confusion, drowsiness, visual disturbances, weakness
Behavioural changes – irritability, aggression (often noticed by others first)
Severe symptoms – loss of consciousness, seizures (requiring emergency treatment)
Patients taking Wegovy, particularly those with diabetes on combination therapy, should be educated about these warning signs. Hypoglycaemia awareness can be impaired in some individuals, especially those with long-standing diabetes, making regular monitoring more important.
Immediate management of mild-to-moderate hypoglycaemia (as recommended by Diabetes UK and NHS guidance):
Consume 15–20 grams of fast-acting carbohydrate:
150–200 ml pure fruit juice
4–5 glucose tablets
5–6 standard jelly babies
Severe hypoglycaemia (where the person cannot self-treat) requires:
Glucagon injection (if available and the person is trained to administer it) – family members should be instructed
Nasal glucagon (Baqsimi) – an alternative option available in the UK that doesn't require injection
Emergency services (999) – if glucagon unavailable, ineffective, or the person does not regain consciousness
Never attempt oral treatment in someone who is unconscious or unable to swallow safely
Patients at risk of hypoglycaemia should be advised to carry fast-acting carbohydrate with them at all times and consider wearing medical identification. They should contact their GP or diabetes specialist nurse if they experience recurrent hypoglycaemic episodes, as medication adjustment is likely necessary.
Appropriate monitoring strategies depend on individual patient characteristics, particularly the presence of diabetes and concurrent medications.
For patients without diabetes using Wegovy for weight management:
Routine blood glucose monitoring is not typically required, as hypoglycaemia risk is low
Patients should be counselled about maintaining adequate nutritional intake despite appetite suppression
Report any symptoms suggestive of hypoglycaemia (tremor, sweating, confusion) to their healthcare provider
Annual HbA1c testing may be appropriate for those with prediabetes or metabolic syndrome
For patients with type 2 diabetes on combination therapy:
Self-monitoring of blood glucose (SMBG) frequency should be individualised based on hypoglycaemia risk
Those on insulin or sulphonylureas should monitor more frequently, particularly during Wegovy initiation and dose escalation
Continuous glucose monitoring (CGM) may be considered for high-risk individuals or those with impaired awareness, in line with NICE and NHS England access criteria
Medication review and adjustment – sulphonylurea and insulin doses often require reduction when starting GLP-1 therapy; adjustments should be individualised and monitored closely under clinical supervision
NICE-aligned safety recommendations include:
Structured education about hypoglycaemia recognition and management for all at-risk patients
Driving safety – patients must be aware of DVLA regulations regarding hypoglycaemia and driving; Group 1 drivers (cars/motorcycles) must notify the DVLA if they have recurrent severe hypoglycaemia or impaired awareness; Group 2 drivers (lorries/buses) face stricter requirements
Occupational considerations – certain occupations (working at heights, operating machinery) require particular caution
Regular review appointments – typically at 3, 6, and 12 months after initiation, then annually, in line with NICE TA875 recommendations for specialist weight management service follow-up
When to contact your GP urgently:
Recurrent hypoglycaemic episodes (more than one per week)
Severe hypoglycaemia requiring third-party assistance
Loss of hypoglycaemia awareness (no longer experiencing warning symptoms)
Uncertainty about medication management
Patients should maintain an up-to-date medication list and inform all healthcare providers about Wegovy use, particularly before surgical procedures or when other medications are prescribed. Pharmacists play a valuable role in identifying potential drug interactions and reinforcing safety advice during prescription collection.
Yes, hypoglycaemia is listed as a common side effect (up to 1 in 10 people) even in people without diabetes, though the risk is low when Wegovy is used alone. Symptoms are often related to inadequate caloric intake or increased physical activity rather than direct drug effects.
Sulphonylureas (such as gliclazide), insulin, and meglitinides significantly increase hypoglycaemia risk when combined with Wegovy. NICE guidance recommends dose reduction of these medications when starting GLP-1 receptor agonist therapy.
Consume 15–20 grams of fast-acting carbohydrate (such as 150–200 ml fruit juice or 4–5 glucose tablets), wait 10–15 minutes, and recheck blood glucose if possible. If symptoms persist or recur frequently, contact your GP for medication review.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.