
Many people wonder whether Wegovy speeds up metabolism as part of its weight management approach. Wegovy (semaglutide 2.4 mg) is a GLP-1 receptor agonist licensed by the MHRA for chronic weight management in adults with obesity or overweight with weight-related comorbidities. Contrary to popular belief, Wegovy does not directly increase basal metabolic rate or thermogenesis. Instead, it works primarily by reducing appetite and promoting feelings of fullness, leading to decreased caloric intake. Understanding how Wegovy actually functions helps set realistic expectations and supports informed treatment decisions within specialist weight management services.
Quick Answer: Wegovy does not speed up metabolism; it facilitates weight loss primarily through appetite suppression and reduced caloric intake rather than increasing basal metabolic rate.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWegovy (semaglutide 2.4 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed by the MHRA for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27-<30 kg/m²) with at least one weight-related comorbidity. Contrary to common misconceptions, Wegovy does not directly speed up metabolism in the traditional sense of increasing basal metabolic rate or thermogenesis.
The medication works by mimicking the action of naturally occurring GLP-1, a hormone produced in the intestines following food intake. Semaglutide binds to GLP-1 receptors located throughout the body, particularly in the brain, pancreas, and gastrointestinal tract. This binding triggers several physiological responses that collectively support weight reduction.
In the pancreas, Wegovy enhances glucose-dependent insulin secretion and suppresses inappropriate glucagon release, thereby improving glycaemic control. This mechanism explains why semaglutide was initially developed for type 2 diabetes management (marketed as Ozempic at lower doses). In the brain, particularly within the hypothalamus and brainstem regions controlling appetite, the medication modulates neural pathways involved in hunger and satiety signalling.
According to NICE Technology Appraisal 875, Wegovy should be prescribed within specialist weight management services that offer comprehensive lifestyle support.
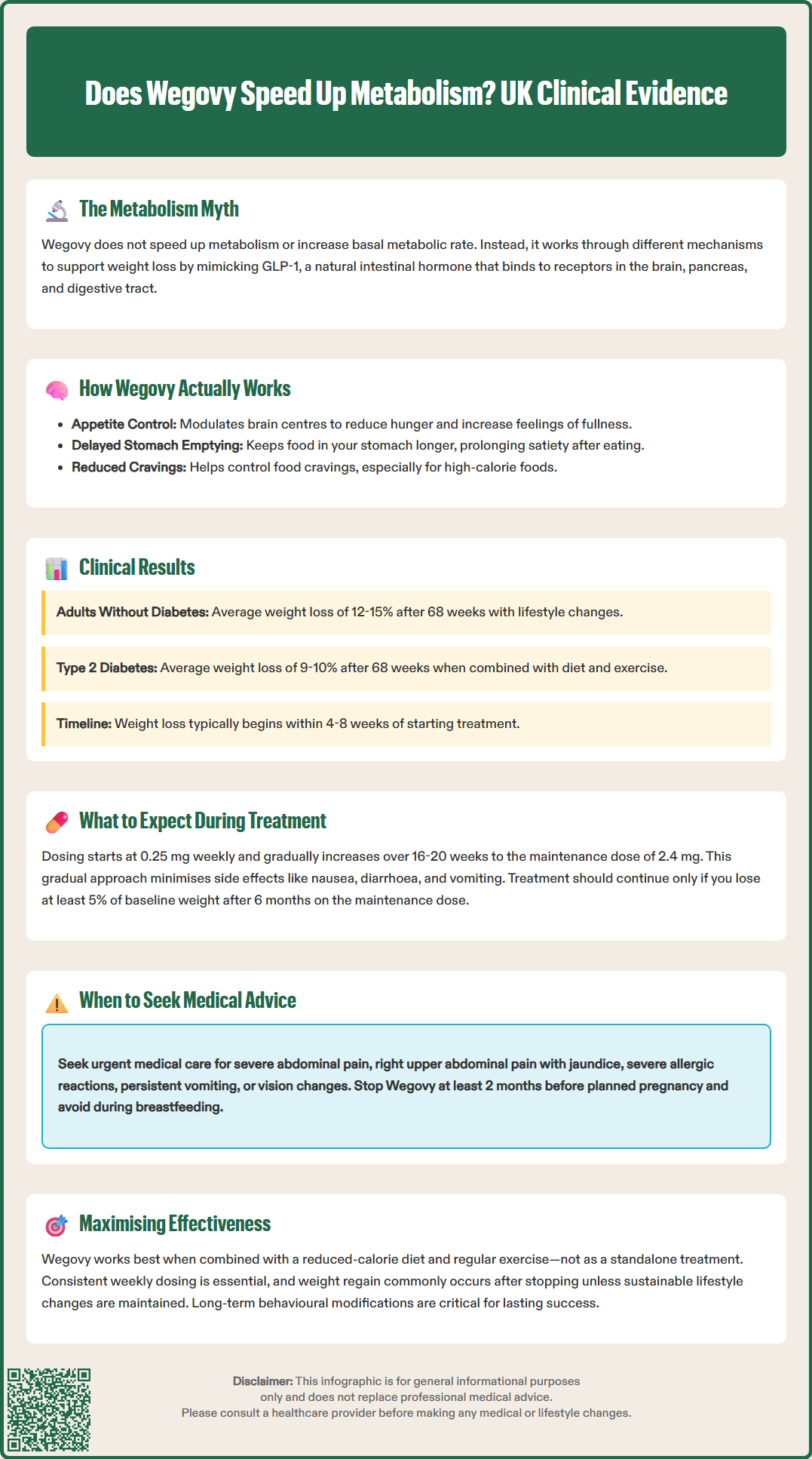
The primary mechanism through which Wegovy facilitates weight loss is appetite suppression and reduced energy intake, not metabolic enhancement. Clinical trials, including the STEP (Semaglutide Treatment Effect in People with obesity) programme, demonstrate that patients typically consume fewer calories due to increased satiety and decreased hunger signals.
Wegovy acts centrally on appetite-regulating centres in the brain, particularly the arcuate nucleus of the hypothalamus. By activating GLP-1 receptors in these regions, semaglutide influences the balance between orexigenic (appetite-stimulating) and anorexigenic (appetite-suppressing) neuropeptides. This results in earlier satiation during meals and prolonged feelings of fullness between eating occasions.
The delayed gastric emptying induced by Wegovy contributes significantly to these satiety effects. Food remains in the stomach longer, sending sustained signals of fullness to the brain. Patients often report feeling satisfied with smaller portion sizes and experiencing reduced food cravings, particularly for high-calorie, palatable foods.
Key weight loss mechanisms include:
Reduced appetite and hunger between meals
Earlier satiation during eating occasions
Decreased food cravings and preoccupation with food
Slower gastric emptying prolonging fullness
Improved control over eating behaviours
Whilst some research suggests GLP-1 receptor agonists may have minor effects on energy expenditure, current evidence shows no clinically meaningful increase in basal metabolic rate, fat oxidation, or thermogenesis. Weight reduction occurs predominantly through the caloric deficit created by reduced food intake. In clinical trials, when combined with lifestyle modifications, average weight loss was approximately 12-15% at 68 weeks in adults without diabetes (STEP 1), and somewhat lower (about 9-10%) in people with type 2 diabetes (STEP 2). Individual results vary considerably based on adherence to lifestyle changes and other factors.
Wegovy treatment follows a structured dose-escalation schedule over 16-20 weeks to minimise gastrointestinal side effects whilst achieving the therapeutic maintenance dose of 2.4 mg weekly. Patients typically begin with 0.25 mg weekly for four weeks, gradually increasing through 0.5 mg, 1 mg, and 1.7 mg before reaching the full dose.
Common adverse effects predominantly involve the gastrointestinal system and include nausea (reported by 20-44% of patients), diarrhoea, constipation, vomiting, and abdominal discomfort. These effects are usually most pronounced during dose escalation and often diminish with continued treatment. Taking the injection on the same day each week and eating smaller, more frequent meals may help manage these symptoms.
Weight loss typically becomes noticeable within 4-8 weeks of treatment, with progressive reduction continuing over 12-18 months. According to NICE guidance (TA875), treatment should be reassessed after 6 months on the maintenance dose (or maximum tolerated dose). Continuation is appropriate only if patients achieve at least 5% weight loss from baseline. Treatment is prescribed for a maximum of 2 years within specialist weight management services.
Patients should seek urgent medical attention if they experience:
Severe, persistent abdominal pain (potential pancreatitis)
Signs of gallbladder problems (right upper abdominal pain, jaundice)
Severe allergic reaction (swelling of face/throat, breathing difficulty)
Persistent vomiting leading to dehydration
Changes in vision, particularly in people with diabetes or existing retinopathy
Wegovy is contraindicated in pregnancy and should be discontinued at least 2 months before a planned pregnancy due to its long half-life. It is not recommended during breastfeeding. People taking insulin or sulfonylureas may need dose adjustments to reduce hypoglycaemia risk.
Wegovy is administered via subcutaneous injection in the abdomen, thigh, or upper arm. Patients receive training on proper injection technique. The medication should be stored in a refrigerator (2-8°C) and protected from light, though it can be kept at temperatures up to 30°C for up to 28 days. Treatment is most effective when combined with a reduced-calorie diet and increased physical activity.
Suspected side effects should be reported via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Individual response to Wegovy varies considerably, with multiple factors determining treatment outcomes. Understanding these variables helps set realistic expectations and optimise therapeutic success.
Adherence to lifestyle modifications significantly impacts results. Wegovy is licensed as an adjunct to a reduced-calorie diet and increased physical activity, not as monotherapy. Patients who actively engage with dietary changes and regular exercise typically achieve superior weight loss compared to those relying solely on medication. NICE recommends that Wegovy be prescribed within specialist weight management services offering comprehensive lifestyle support.
Baseline characteristics influence outcomes. Patients with higher starting body mass index (BMI) often lose more absolute weight, though percentage reductions may be similar across BMI categories. Age, sex, and ethnicity may affect response, though clinical trials demonstrate efficacy across diverse populations. Evidence from the STEP 2 trial shows that while weight loss remains clinically meaningful in people with type 2 diabetes, the average reduction is somewhat smaller than in those without diabetes.
Medication adherence is crucial. Missing doses or discontinuing treatment prematurely reduces effectiveness. The once-weekly dosing schedule improves adherence compared to daily medications, but patients must maintain consistency. If a dose is missed, it should be administered within five days; otherwise, the next scheduled dose should be taken.
Individual variability in response may be influenced by genetic factors and metabolic differences affecting GLP-1 receptor sensitivity and drug metabolism, though these are not routinely assessed in clinical practice. Regarding medication interactions, the MHRA SmPC notes few clinically relevant interactions, though delayed gastric emptying can affect absorption timing of some oral medicines. Combining Wegovy with other GLP-1 receptor agonists should be avoided.
Psychological factors including eating behaviours, stress management, and mental health status influence outcomes. Patients with binge eating disorder or significant emotional eating may require additional psychological support alongside pharmacotherapy. Realistic goal-setting and understanding that Wegovy facilitates—but does not replace—healthy lifestyle changes are essential for long-term success. Weight regain commonly occurs if treatment is discontinued without maintained lifestyle modifications, emphasising the importance of sustainable behavioural changes.
Wegovy causes weight loss primarily by suppressing appetite and increasing feelings of fullness, which leads to reduced caloric intake. It acts on brain appetite centres and delays gastric emptying, helping patients feel satisfied with smaller portions and experience fewer food cravings.
Weight loss typically becomes noticeable within 4-8 weeks of starting Wegovy, with progressive reduction continuing over 12-18 months. NICE guidance requires reassessment at 6 months, with continuation appropriate only if at least 5% weight loss from baseline is achieved.
The most common side effects are gastrointestinal, including nausea (affecting 20-44% of patients), diarrhoea, constipation, vomiting, and abdominal discomfort. These effects are usually most pronounced during dose escalation and often diminish with continued treatment.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.