
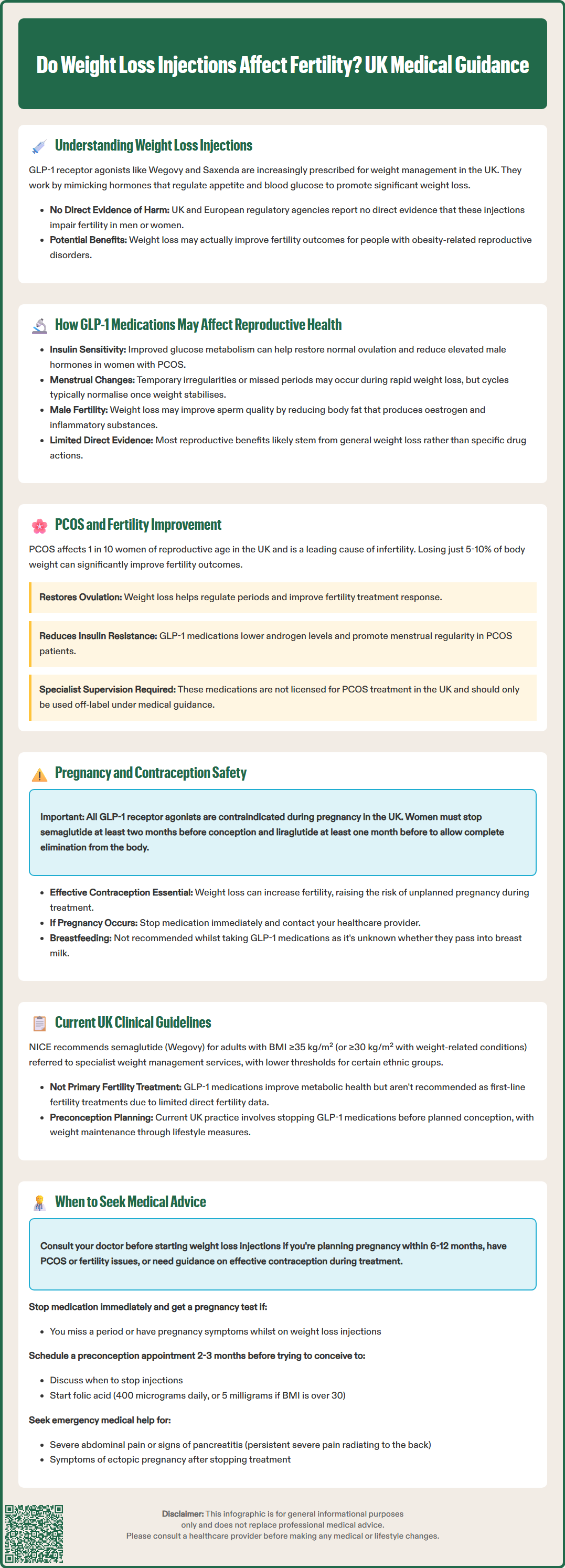
Weight loss injections, particularly GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), are increasingly prescribed for weight management in the UK. As more individuals of reproductive age use these medications, questions arise about their potential impact on fertility. Currently, there is no direct evidence that GLP-1 receptor agonists impair fertility in men or women. However, the indirect effects of weight loss, hormonal changes, and metabolic improvements can influence reproductive function. For those planning pregnancy, understanding both the potential benefits and necessary precautions is essential. Weight loss achieved through these medications may improve fertility outcomes in certain populations, particularly those with obesity-related reproductive disorders, though specific safety considerations apply during the preconception period and pregnancy.
Quick Answer: Weight loss injections (GLP-1 receptor agonists) do not directly impair fertility, but may indirectly improve it through weight loss and metabolic benefits, particularly in women with PCOS, though they must be stopped before conception.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWeight loss injections, particularly glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have become increasingly prescribed for weight management in the UK. As more individuals of reproductive age use these medications, questions naturally arise about their potential impact on fertility and reproductive health.
These injectable medications work by mimicking natural hormones that regulate appetite and blood glucose levels. They slow gastric emptying, increase feelings of fullness, and reduce food intake, leading to significant weight loss in many patients. However, the relationship between these medications and fertility is complex and multifaceted.
Currently, there is limited human data on whether GLP-1 receptor agonists affect fertility in either men or women. According to the Medicines and Healthcare products Regulatory Agency (MHRA) product information, animal studies have not indicated direct harmful effects on fertility, but comprehensive human fertility studies are lacking. It's important to note that semaglutide (Ozempic) is licensed only for type 2 diabetes in the UK, not for weight management.
For individuals planning pregnancy or currently trying to conceive, understanding both the potential benefits and precautions associated with weight loss injections is essential. The interaction between body weight, metabolic health, and fertility means that weight loss achieved through these medications may actually improve fertility outcomes in certain populations, particularly those with obesity-related reproductive disorders. Nevertheless, specific safety considerations apply during pregnancy and the preconception period, which require careful medical guidance and planning.
GLP-1 receptor agonists exert their effects primarily through the central nervous system and gastrointestinal tract, but GLP-1 receptors are also present in reproductive tissues, including the ovaries, uterus, and testes. The clinical significance of this receptor distribution remains an area of ongoing research and is not yet fully understood.
In terms of mechanism of action, these medications enhance insulin sensitivity and improve glucose metabolism. Since insulin resistance plays a crucial role in several reproductive disorders, particularly polycystic ovary syndrome (PCOS), the metabolic improvements induced by GLP-1 agonists may have beneficial effects on reproductive function. Improved insulin sensitivity can help restore normal ovulatory cycles in women with PCOS and reduce hyperandrogenism (elevated male hormones).
Rapid weight loss itself can temporarily disrupt menstrual cycles in some women. When the body experiences significant caloric restriction or rapid fat loss, it may interpret this as a period of nutritional stress, potentially affecting the hypothalamic-pituitary-ovarian axis. This can lead to irregular periods or temporary amenorrhoea (absence of menstruation). However, these changes are typically transient and resolve as weight stabilises.
For men, obesity is associated with reduced testosterone levels, impaired sperm quality, and erectile dysfunction. Weight loss achieved through GLP-1 receptor agonists may improve male fertility parameters, though evidence is primarily observational and limited. The potential benefits occur by reducing adipose tissue, which produces oestrogen and inflammatory cytokines that negatively affect testosterone production and sperm function. Men experiencing fertility difficulties should still undergo standard fertility investigations regardless of weight loss treatment, as recommended by NICE fertility guidelines.
Polycystic ovary syndrome (PCOS) affects approximately one in ten women of reproductive age in the UK and is a leading cause of anovulatory infertility. The condition is characterised by irregular menstrual cycles, hyperandrogenism, and polycystic ovarian morphology on ultrasound. Importantly, insulin resistance and obesity are present in 50–70% of women with PCOS, creating a complex interplay between metabolic and reproductive dysfunction.
Weight loss of just 5–10% of body weight can significantly improve fertility outcomes in women with PCOS, according to the International Evidence-based Guideline for PCOS (2023) and NICE Clinical Knowledge Summary. This modest weight reduction can restore ovulation, improve menstrual regularity, and enhance response to fertility treatments. GLP-1 receptor agonists have shown promise in achieving this therapeutic weight loss target in women with PCOS.
Several clinical studies have demonstrated that liraglutide and semaglutide can improve metabolic parameters in PCOS, including reducing insulin resistance, lowering androgen levels, and promoting weight loss. Some research indicates improved menstrual regularity and ovulation rates following treatment with these medications. However, it's important to emphasise that GLP-1 receptor agonists are not currently licensed specifically for PCOS treatment in the UK, and their use in this context would be considered off-label and should be under specialist oversight.
The fertility benefits observed with weight loss injections in PCOS are primarily attributed to weight reduction and metabolic improvement rather than a direct effect on ovarian function. Women with PCOS who achieve significant weight loss through these medications may find their natural fertility improves, potentially reducing the need for assisted reproductive technologies. However, because these medications are contraindicated during pregnancy, careful planning and contraception are essential during treatment, with discontinuation required before attempting conception.
All currently available GLP-1 receptor agonists are contraindicated during pregnancy in the UK. The Summary of Product Characteristics (SmPC) for medications such as semaglutide and liraglutide clearly states that they should not be used during pregnancy due to insufficient data on safety for the developing foetus. Animal studies have shown potential risks, including skeletal abnormalities and growth restriction, though the relevance to human pregnancy remains uncertain.
The MHRA and manufacturer guidance recommend that women of childbearing potential should use effective contraception during treatment with weight loss injections. If pregnancy is planned, semaglutide (Wegovy) should be discontinued at least two months before conception due to its longer half-life of approximately one week. For liraglutide (Saxenda), the SmPC advises discontinuation when planning pregnancy, without specifying a particular timeframe. These medications do not have clinically meaningful interactions with combined oral contraceptives.
An important consideration is that weight loss and metabolic improvement may increase fertility, potentially leading to unplanned pregnancy in women who were previously subfertile due to obesity or PCOS. Healthcare professionals should counsel patients about this possibility and ensure appropriate contraceptive measures are in place throughout treatment. Women should be advised to perform a pregnancy test if they miss a period or experience pregnancy symptoms.
If pregnancy occurs while taking a GLP-1 receptor agonist, the medication should be stopped immediately, and the patient should contact their GP or healthcare provider for guidance. There is currently limited human data on inadvertent exposure in early pregnancy; patients should be referred for specialist advice, potentially including consultation with the UK Teratology Information Service (UKTIS). Breastfeeding is also not recommended while taking these medications, as the SmPCs state it is unknown whether they pass into breast milk in clinically significant amounts.
The evidence base regarding GLP-1 receptor agonists and fertility is evolving but remains limited. Most clinical trials of these medications have excluded pregnant women and those actively trying to conceive, meaning direct fertility data is sparse. However, several observational studies and secondary analyses provide useful insights.
A systematic review examining metabolic and reproductive outcomes in women with PCOS found that GLP-1 receptor agonists improved body weight, insulin sensitivity, and menstrual regularity compared to placebo or metformin alone. However, the review authors noted that dedicated fertility outcome studies are needed, and current evidence does not support using these medications as primary fertility treatments.
NICE Technology Appraisals provide specific guidance on GLP-1 receptor agonists for weight management in the UK. Semaglutide (Wegovy) and liraglutide (Saxenda) are recommended within specialist weight management services for adults with a BMI of at least 35 kg/m² (or ≥32.5 kg/m² for people from South Asian, Chinese, other Asian, Middle Eastern, Black African, or African-Caribbean backgrounds) with at least one weight-related comorbidity. These medications are prescribed as part of a comprehensive weight management programme with specific eligibility criteria and treatment duration limits.
The Royal College of Obstetricians and Gynaecologists (RCOG) emphasises that obesity significantly impacts fertility and pregnancy outcomes, recommending weight optimisation before conception. However, specific guidance on GLP-1 receptor agonists in the preconception period is still developing as these medications become more widely used.
Current UK prescribing practice typically involves discontinuing weight loss injections before planned conception, with a focus on maintaining weight loss through lifestyle measures during the preconception period and pregnancy. Healthcare professionals should provide individualised advice based on each patient's circumstances, including their BMI, underlying conditions, and fertility goals.
Individuals considering or currently using weight loss injections should seek medical advice in several specific circumstances related to fertility and reproductive health:
Before starting treatment:
If you are planning pregnancy within the next 6–12 months, discuss whether weight loss injections are appropriate or whether alternative weight management strategies should be prioritised
If you have PCOS or other fertility concerns, ensure your healthcare provider considers how treatment may affect your reproductive health
Discuss contraception requirements and ensure you have effective contraceptive measures in place if pregnancy is not desired
During treatment:
If you experience significant menstrual irregularities (either new irregular bleeding or absence of periods), contact your GP to rule out pregnancy and assess whether this represents a treatment effect
If you suspect you might be pregnant (missed period, pregnancy symptoms), stop the medication immediately and arrange a pregnancy test and medical review
If you develop severe gastrointestinal symptoms (persistent nausea, vomiting, abdominal pain) that prevent adequate nutrition, seek medical advice, as this may affect overall health and fertility
Report any suspected side effects via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk)
When planning pregnancy:
Schedule a preconception consultation with your GP or fertility specialist at least 2–3 months before you plan to conceive
Discuss the appropriate timing for stopping weight loss injections and strategies for maintaining weight loss through lifestyle measures
Ensure you begin taking folic acid supplementation (400 micrograms daily, or 5 milligrams daily if BMI >30 kg/m² – note this higher dose requires a prescription in the UK) before conception
Consider referral to specialist services if you have complex medical needs or have been trying to conceive unsuccessfully for 12 months (or 6 months if aged over 35), in line with NICE fertility guidelines
Emergency situations requiring urgent medical attention include severe abdominal pain, signs of pancreatitis, or any symptoms suggesting ectopic pregnancy (such as one-sided lower abdominal pain, shoulder-tip pain, vaginal bleeding, or dizziness/collapse) in someone who has recently stopped weight loss injections and may have conceived.
No, weight loss injections such as semaglutide and liraglutide are contraindicated during pregnancy and should be stopped at least two months before planned conception. Women of childbearing potential must use effective contraception during treatment.
Weight loss injections may improve fertility in women with PCOS by promoting weight loss, reducing insulin resistance, and lowering androgen levels, which can restore ovulation and menstrual regularity. However, they are not licensed specifically for PCOS treatment in the UK.
If you become pregnant whilst taking weight loss injections, stop the medication immediately and contact your GP or healthcare provider for guidance. Perform a pregnancy test if you miss a period or experience pregnancy symptoms.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.