Mounjaro (tirzepatide) is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus. Whilst its appetite-suppressing effects contribute to improved glycaemic control, many patients experience significantly reduced hunger, sometimes making it challenging to maintain adequate nutritional intake. Forcing yourself to eat on Mounjaro may feel counterintuitive when natural hunger cues diminish, yet structured nutrition remains essential for preserving muscle mass, preventing deficiencies, and supporting metabolic health. Understanding how to manage appetite suppression safely—through scheduled meals, nutrient-dense foods, and proactive communication with your healthcare team—ensures that treatment remains both effective and sustainable for your individual circumstances.
Quick Answer: Forcing yourself to eat on Mounjaro may be necessary because tirzepatide significantly suppresses appetite, but maintaining adequate nutrition through structured meals prevents muscle loss, nutritional deficiencies, and metabolic complications.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMounjaro (tirzepatide) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK specifically for the treatment of type 2 diabetes mellitus. Its mechanism of action involves mimicking naturally occurring incretin hormones that regulate blood glucose levels and appetite. By activating both GIP and GLP-1 receptors, Mounjaro slows gastric emptying (most pronounced after initial doses), enhances insulin secretion in response to meals, and reduces glucagon release. Importantly, it also acts on appetite centres in the hypothalamus, leading to significant reductions in hunger and food intake.
The appetite-suppressing effects of Mounjaro are among its most pronounced actions. Many patients report a marked decrease in hunger, early satiety (feeling full quickly), and sometimes a significantly reduced interest in food. Whilst this contributes to the weight loss often observed with tirzepatide therapy, it can also create nutritional challenges. Some individuals find themselves needing to consciously plan meals, as natural hunger cues become substantially diminished.
This appetite suppression typically begins within the first few weeks of treatment and may intensify following dose escalations. The effect varies considerably between individuals—some experience mild reductions in appetite, whilst others report much more pronounced effects. Understanding that this is an expected pharmacological effect of the medication, rather than a cause for immediate alarm, helps patients and clinicians manage the situation appropriately. However, maintaining adequate nutritional intake remains essential for overall health, metabolic function, and preventing adverse outcomes such as excessive muscle loss or nutritional deficiencies.
It's worth noting that the delayed gastric emptying effect can temporarily reduce the absorption of oral medications, including oral contraceptives. Women using oral contraceptives should consider using an additional non-hormonal contraceptive method for 4 weeks after starting Mounjaro and for 4 weeks after each dose increase.
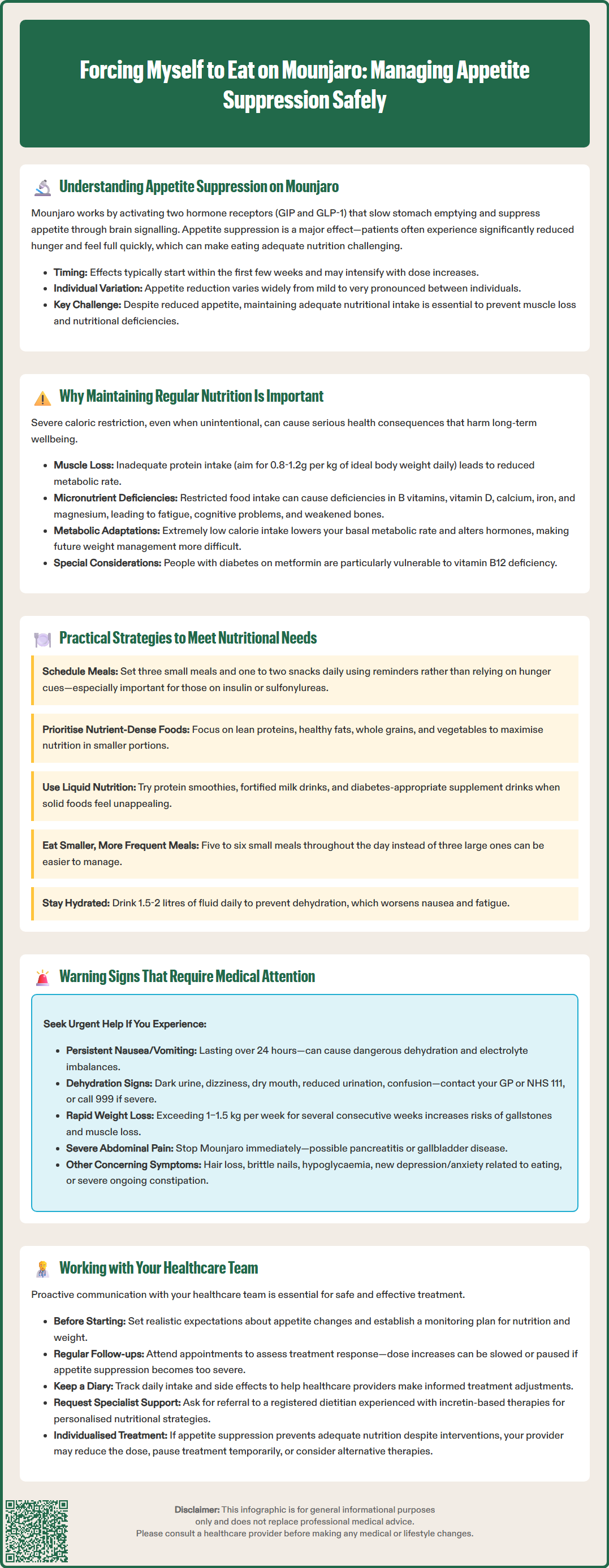
Despite reduced appetite, maintaining adequate caloric and nutritional intake is essential for several physiological reasons. Severe caloric restriction—even when unintentional—can lead to loss of lean muscle mass, nutritional deficiencies, fatigue, and metabolic adaptations that may ultimately hinder long-term health outcomes. Whilst Mounjaro is designed to improve glycaemic control in type 2 diabetes, with weight loss as a beneficial additional effect in appropriate patients, this should occur through controlled, sustainable reductions in energy intake rather than through involuntary inadequate nutrition.
Protein intake deserves particular attention. Adequate protein consumption is important for preserving muscle mass during weight loss. Without sufficient protein, the body may catabolise muscle tissue to meet its amino acid requirements, leading to sarcopenia, reduced metabolic rate, and functional decline. This is especially important for older adults or those with pre-existing muscle loss. Protein requirements vary by individual circumstances—typically 0.8-1.2g per kilogram of ideal body weight daily is recommended for most adults, though requirements may be lower in those with kidney disease. An HCPC-registered dietitian can provide personalised advice.
Micronutrient deficiencies represent another significant concern. Vitamins and minerals—including B vitamins, vitamin D, calcium, iron, and magnesium—are essential for numerous bodily functions. Severely restricted food intake over extended periods can contribute to deficiencies that manifest as fatigue, cognitive impairment, bone health deterioration, and immune dysfunction. Patients with diabetes may be particularly vulnerable to certain deficiencies (such as vitamin B12 deficiency in those on long-term metformin) that can complicate glycaemic control and overall health.
Furthermore, extremely low caloric intake can trigger adaptive metabolic responses, including reduced basal metabolic rate and hormonal changes that may make subsequent weight management more challenging. Structured, adequate nutrition—even when appetite is suppressed—supports sustainable metabolic health and helps prevent the adverse consequences of malnutrition whilst still allowing for appropriate therapeutic weight loss where indicated.
When natural hunger signals are diminished, adopting structured eating patterns becomes essential. Scheduled meals rather than appetite-driven eating can help ensure consistent nutritional intake. Setting reminders for three small meals and one to two snacks daily creates a framework that doesn't rely on hunger cues. Even if portions are smaller than pre-treatment, regular eating prevents prolonged fasting periods and supports metabolic stability. This is particularly important if you are taking insulin or sulfonylureas, as skipping meals could increase hypoglycaemia risk.
Nutrient-dense foods should be prioritised to maximise nutritional value in smaller volumes. Focus on:
High-quality proteins: lean meats, fish, eggs, Greek yoghurt, cottage cheese, legumes, and tofu provide essential amino acids in relatively small servings
Healthy fats: avocados, nuts, seeds, olive oil, and oily fish deliver concentrated energy and fat-soluble vitamins
Whole grains and complex carbohydrates: brown rice, quinoa, oats, and wholemeal bread provide sustained energy and fibre
Fruits and vegetables: whilst important for micronutrients and fibre, these should complement rather than replace protein and energy-dense foods when appetite is severely suppressed
Liquid nutrition can be particularly helpful when solid food feels unappealing or overwhelming. Protein smoothies, fortified milk drinks, soups with added protein powder, and nutritional supplement drinks (preferably diabetes-appropriate formulations with lower sugar content) can provide substantial nutrition in more palatable forms. These are often better tolerated than solid meals when nausea or early satiety is problematic.
Consider smaller, more frequent portions rather than attempting standard meal sizes. Eating five to six small meals throughout the day may feel more manageable than three larger ones. If nausea is an issue, lower-fat options may be better tolerated. Protein-rich snacks such as cheese, nuts, boiled eggs, or protein bars can bridge gaps between meals.
Adequate hydration is crucial, especially as dehydration can worsen nausea and fatigue. Aim for 1.5-2 litres of fluid daily, monitoring urine colour (pale straw colour indicates good hydration). Some patients find that certain times of day are more conducive to eating; identifying and capitalising on these windows can improve overall intake. Working with a registered dietitian experienced in supporting patients on GLP-1 receptor agonist therapy can provide personalised strategies tailored to individual circumstances, preferences, and nutritional requirements.
Whilst reduced appetite is an expected effect of Mounjaro, certain symptoms indicate that nutritional intake has become inadequate or that other complications have developed. Persistent nausea and vomiting that prevents any meaningful food or fluid intake for more than 24 hours requires urgent medical assessment. Severe or prolonged vomiting can lead to dehydration, electrolyte imbalances, and acute kidney injury—complications that necessitate prompt intervention.
Signs of dehydration include dark-coloured urine, dizziness upon standing, dry mouth, reduced urine output, and confusion. Patients should contact their GP or NHS 111 if these symptoms develop, as intravenous fluid replacement may be necessary. Dehydration is particularly concerning for individuals with diabetes, as it can precipitate hyperosmolar hyperglycaemic state (HHS) in type 2 diabetes, or diabetic ketoacidosis (DKA) in insulin-deficient states. Call 999 or attend A&E if symptoms are severe.
Unintentional weight loss exceeding 1–1.5 kg per week over several consecutive weeks may indicate excessive caloric restriction. Whilst weight loss is often a beneficial effect, excessively rapid loss increases the risk of gallstones, muscle wasting, and nutritional deficiencies. Patients should discuss concerning weight loss patterns with their healthcare provider, who may recommend dose adjustment or additional nutritional support.
Other warning signs include:
Severe, persistent abdominal pain (which may indicate pancreatitis, a rare but serious adverse effect). If pancreatitis is suspected, stop taking Mounjaro immediately and seek urgent medical attention. Do not restart if pancreatitis is confirmed.
Right upper quadrant pain, fever, or yellowing of the skin/eyes (possible gallbladder disease)
Extreme fatigue or weakness that interferes with daily activities
Hair loss, brittle nails, or other signs of nutritional deficiency
Symptoms of hypoglycaemia (particularly in patients taking insulin or sulfonylureas concurrently)
New or worsening depression or anxiety related to eating difficulties
Severe or ongoing constipation with abdominal distension
Patients experiencing any of these symptoms should contact their GP promptly. In cases of severe abdominal pain, persistent vomiting, or signs of serious dehydration, call 999 or attend A&E immediately. Regular monitoring and open communication with healthcare providers help identify problems early and prevent serious complications. Report suspected side effects via the Yellow Card scheme at yellowcard.mhra.gov.uk or via the Yellow Card app.
Proactive communication with your healthcare team is essential when managing appetite suppression on Mounjaro. Before starting treatment, discuss realistic expectations about appetite changes and establish a plan for monitoring nutritional intake and weight. Your prescribing clinician—whether a GP, diabetes specialist nurse, or consultant—should provide guidance on recognising concerning symptoms and when to seek advice.
Regular follow-up appointments allow for assessment of treatment response, side effects, and nutritional status. NICE guidance (NG28 and the technology appraisal for tirzepatide) recommends ongoing monitoring of patients prescribed GLP-1 receptor agonists, including assessment of glycaemic control, weight, and tolerability. These appointments provide opportunities to discuss eating difficulties, review weight loss patterns, and adjust treatment if necessary. Some patients benefit from dose titration adjustments—slowing the rate of dose increases (standard titration is 2.5mg weekly, increasing by 2.5mg every 4 weeks as tolerated) or temporarily maintaining a lower dose can sometimes improve tolerability whilst still providing therapeutic benefit.
Referral to specialist services may be appropriate in certain circumstances. A registered dietitian can provide expert nutritional assessment and develop personalised eating strategies. Dietitians experienced in supporting patients on incretin-based therapies understand the unique challenges these medications present and can recommend specific interventions, including appropriate use of nutritional supplements. For patients with complex diabetes management needs or those experiencing significant complications, referral to specialist diabetes services ensures comprehensive, multidisciplinary care.
Patients should maintain a symptom and food diary to track eating patterns, symptoms, and any concerning changes. This information helps healthcare providers make informed decisions about treatment adjustments. Recording daily food intake, even when minimal, provides objective data that can guide nutritional interventions. Similarly, documenting symptoms such as nausea, vomiting, or abdominal discomfort helps identify patterns and triggers.
It's important to note that Mounjaro is not recommended during pregnancy or breastfeeding. Women of childbearing potential should use effective contraception while taking tirzepatide, being aware that oral contraceptive effectiveness may be reduced after starting treatment or increasing doses.
Finally, remember that treatment should be individualised. If appetite suppression becomes so severe that adequate nutrition cannot be maintained despite interventions, your healthcare provider may recommend dose reduction, temporary treatment interruption, or consideration of alternative therapies. The goal is to achieve therapeutic benefit—improved glycaemic control and, where appropriate, weight management—whilst maintaining overall health and quality of life. Open dialogue with your healthcare team ensures that treatment remains safe, effective, and sustainable for your individual circumstances.
Mounjaro (tirzepatide) activates GIP and GLP-1 receptors, which slow gastric emptying and act on appetite centres in the hypothalamus, leading to significantly reduced hunger and early satiety. This is an expected pharmacological effect that varies in intensity between individuals.
Prioritise nutrient-dense foods including high-quality proteins (lean meats, fish, eggs, Greek yoghurt), healthy fats (nuts, avocados, oily fish), and whole grains. Liquid nutrition such as protein smoothies and fortified drinks may be better tolerated when solid food feels overwhelming.
Contact your GP if you experience persistent vomiting preventing food or fluid intake for over 24 hours, signs of dehydration, weight loss exceeding 1–1.5kg weekly over several weeks, severe abdominal pain, or extreme fatigue interfering with daily activities. Severe symptoms require urgent or emergency assessment.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.