
Hair loss whilst taking Ozempic (semaglutide) can be distressing, though it is not listed as a common adverse effect in UK regulatory documentation. Most cases relate to rapid weight reduction triggering telogen effluvium—a temporary shedding phase—rather than direct drug toxicity. Nutritional deficiencies secondary to reduced appetite may also contribute. Understanding the underlying mechanisms and implementing practical strategies, including optimising dietary intake, moderating weight loss pace, and addressing deficiencies through blood tests, can support hair regrowth. This article provides evidence-based guidance aligned with NHS and NICE recommendations to help manage and prevent hair thinning during Ozempic therapy.
Quick Answer: Hair loss from Ozempic is typically temporary telogen effluvium triggered by rapid weight loss, managed through optimised nutrition, gradual weight reduction, and correction of deficiencies.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus and, at higher doses (as Wegovy), for weight management. Whilst hair loss is not listed as a common adverse effect in the Summary of Product Characteristics, some patients report increased hair shedding during treatment. Understanding the potential mechanisms can help contextualise this experience.
The most plausible explanation relates to rapid weight loss rather than a direct pharmacological effect of semaglutide itself. Significant caloric restriction and substantial weight reduction can trigger a condition called telogen effluvium. This is a form of temporary hair shedding that occurs when a large number of hair follicles simultaneously enter the resting (telogen) phase of the hair growth cycle. Typically, telogen effluvium manifests two to four months after the triggering event, which aligns with the timeline many patients observe after starting Ozempic.
Additional contributing factors may include nutritional deficiencies secondary to reduced food intake and dietary quality, particularly inadequate protein, iron, zinc, biotin, and essential vitamins. GLP-1 receptor agonists suppress appetite and delay gastric emptying, which can lead to reduced overall nutrient intake if dietary quality is poor. There is no official link established between semaglutide and direct follicular toxicity, and hair loss is not listed as a recognised adverse drug reaction in regulatory documentation from the MHRA or EMA. However, the physiological stress of metabolic change may indirectly affect hair health, warranting a holistic approach to management.
It's important to note that patchy hair loss or alopecia associated with scalp inflammation or scarring is unlikely to be related to Ozempic and warrants prompt medical assessment to investigate other causes.
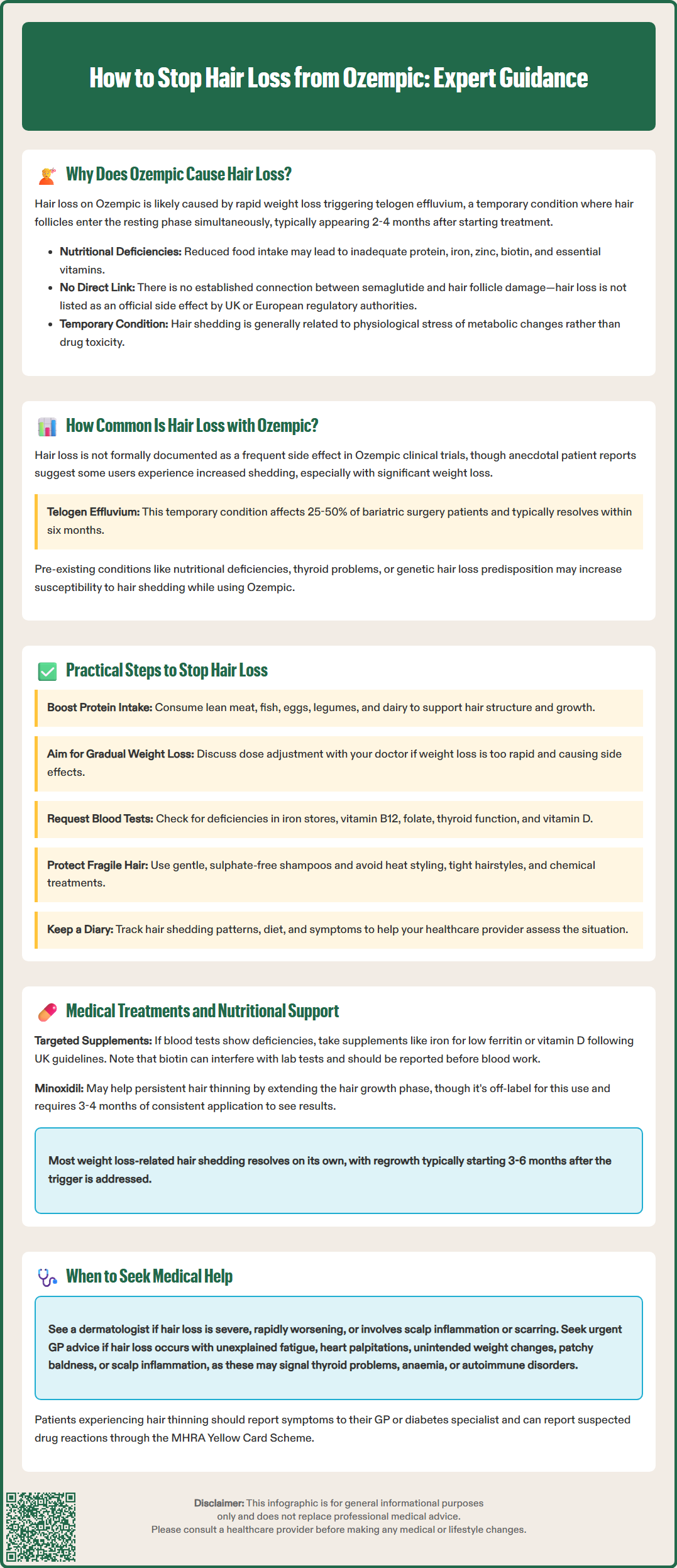
Hair loss associated with Ozempic use is not formally quantified in clinical trial data or post-marketing surveillance reports submitted to the MHRA. In pivotal trials such as SUSTAIN and STEP, alopecia was not reported as a frequent adverse event according to the European Medicines Agency's European Public Assessment Report (EPAR) for semaglutide. However, anecdotal reports from patients and online forums suggest that a subset of individuals—particularly those experiencing substantial weight loss—do notice increased hair shedding.
It is important to distinguish between perceived prevalence and clinically significant alopecia. Telogen effluvium, the likely underlying cause, is generally self-limiting and affects a proportion of individuals undergoing rapid weight reduction, regardless of the method (whether pharmacological, surgical, or dietary). Studies of bariatric surgery patients show variable rates of hair thinning in the months following significant weight loss, with reported ranges of 25-50% depending on the study population and definition used. These figures should be interpreted cautiously as they may not directly translate to GLP-1 receptor agonist users.
Patient-reported outcomes from social media and patient support groups suggest variability in experience. Some individuals report mild, transient shedding that resolves spontaneously within six months, whilst others describe more persistent concerns. It is worth noting that baseline factors—such as pre-existing nutritional deficiencies, thyroid dysfunction, or genetic predisposition to androgenetic alopecia—may amplify susceptibility.
Currently, there is insufficient robust epidemiological data to assign a precise incidence rate. Clinicians should reassure patients that hair loss, if it occurs, is typically temporary and related to metabolic adaptation rather than permanent follicular damage. Patients concerned about hair thinning should be encouraged to report symptoms to their GP or diabetes specialist nurse for appropriate assessment and, if necessary, onward referral to dermatology. Any suspected adverse drug reactions can be reported via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Addressing hair loss in the context of Ozempic therapy requires a multifaceted, patient-centred approach that balances glycaemic control or weight management goals with attention to nutritional adequacy and overall wellbeing. The following practical steps are evidence-informed and align with NICE guidance on holistic diabetes and obesity care.
Optimise nutritional intake: Ensure adequate protein consumption to support keratin synthesis, the structural protein of hair. Include high-quality sources such as lean meat, fish, eggs, legumes, and dairy. A varied, nutrient-dense diet rich in iron (red meat, spinach, lentils), zinc (shellfish, seeds, nuts), biotin (eggs, almonds), and vitamins A, C, D, and E is essential. The NHS Eatwell Guide provides a useful framework for balanced nutrition. Consider referral to a registered dietitian for personalised advice, particularly if appetite suppression is marked or if you have conditions requiring specific dietary management (such as chronic kidney disease).
Moderate the rate of weight loss: Whilst Ozempic is effective for weight reduction, excessively rapid loss may exacerbate telogen effluvium. Aim for a gradual, sustainable pace in line with NICE guidance. Discuss dose titration with your prescribing clinician if weight loss is precipitous and associated with adverse effects.
Address underlying deficiencies: Request blood tests to evaluate full blood count, serum ferritin (iron stores), vitamin B12, folate, thyroid function (TSH, free T4), and vitamin D. Consider coeliac disease screening if iron deficiency is present or symptoms suggest malabsorption. Correcting deficiencies can significantly improve hair regrowth. Supplementation should be guided by laboratory results rather than empirical use.
Maintain scalp and hair health: Use gentle, sulphate-free shampoos and avoid excessive heat styling, tight hairstyles, or chemical treatments that may further stress fragile hair.
Monitor and document: Keep a diary of hair shedding patterns, dietary intake, and any other symptoms. This information is valuable for clinical review and helps distinguish telogen effluvium from other causes of alopecia, such as autoimmune or hormonal conditions.
When conservative measures are insufficient, or if hair loss is distressing or persistent beyond six months, medical interventions may be considered. It is important to emphasise that most cases of telogen effluvium associated with weight loss are self-limiting, with regrowth typically commencing three to six months after the triggering stressor resolves.
Nutritional supplementation: If blood tests confirm deficiencies, targeted supplementation is appropriate. Iron supplementation (e.g., ferrous sulphate) is indicated for low ferritin, with dosing and duration guided by clinical assessment and laboratory values. One tablet daily or alternate-day dosing may improve tolerance, as recommended by NICE Clinical Knowledge Summaries. Vitamin D supplementation should follow UK guidance for deficiency or insufficiency, typically with an appropriate loading dose followed by maintenance therapy as directed by your healthcare provider. Biotin (vitamin B7) is often marketed for hair health, but evidence supporting its efficacy in individuals without true biotin deficiency is weak. Importantly, the MHRA has issued a Drug Safety Update warning that biotin can interfere with laboratory tests, including thyroid function and cardiac troponin; always inform healthcare professionals about biotin supplementation before blood tests. A general multivitamin and mineral supplement may provide a safety net during periods of reduced dietary intake, but should not replace a balanced diet.
Topical minoxidil: For persistent or distressing hair thinning, minoxidil solution or foam may be considered. In the UK, minoxidil is licensed for androgenetic alopecia, with 5% formulations available over-the-counter for men and 2% for women (higher strengths for women require prescription). Its use in telogen effluvium is off-label but sometimes recommended. Minoxidil works by prolonging the anagen (growth) phase of the hair cycle. Patients should be advised that initial shedding may occur, and visible results typically require at least three to four months of consistent use. Consult a pharmacist or healthcare professional before starting treatment.
Referral to dermatology: If hair loss is severe, rapidly progressive, or associated with scalp symptoms (e.g., inflammation, scarring), referral to a dermatologist is warranted. Conditions such as alopecia areata, lichen planopilaris, or androgenetic alopecia require specialist assessment and may necessitate treatments such as topical corticosteroids, immunotherapy, or anti-androgen therapy.
When to seek urgent advice: Contact your GP promptly if hair loss is accompanied by unexplained fatigue, palpitations, weight changes independent of Ozempic, patchy hair loss, scalp inflammation, or other systemic symptoms, as these may indicate thyroid dysfunction, anaemia, autoimmune conditions, or other disorders requiring investigation. Collaborative care involving your diabetes team, dietitian, and dermatologist ensures comprehensive management and supports both metabolic and psychological wellbeing during treatment.
No, hair loss associated with Ozempic is typically temporary telogen effluvium related to rapid weight loss. Regrowth usually begins three to six months after the triggering stressor resolves, provided nutritional deficiencies are addressed.
Request full blood count, serum ferritin, vitamin B12, folate, thyroid function (TSH, free T4), and vitamin D. These tests help identify deficiencies or thyroid dysfunction that may contribute to hair thinning and guide targeted supplementation.
Seek dermatology referral if hair loss is severe, rapidly progressive, persistent beyond six months, or accompanied by scalp inflammation, patchy loss, or scarring. These features may indicate conditions requiring specialist assessment and treatment.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.