
Nausea is one of the most frequently reported side effects of Wegovy (semaglutide), a GLP-1 receptor agonist licensed in the UK for weight management. Understanding how to stop nausea from Wegovy can significantly improve treatment tolerability and adherence. This symptom typically occurs during treatment initiation and dose escalation, affecting approximately 44% of patients. Whilst often temporary and manageable, persistent or severe nausea requires medical review. This article explores evidence-based strategies to minimise Wegovy-related nausea, including dietary modifications, practical management techniques, and guidance on when to seek medical advice.
Quick Answer: Nausea from Wegovy can be managed through gradual dose titration, eating smaller frequent meals, avoiding high-fat foods, staying hydrated, and allowing time for physiological adaptation.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWegovy (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with obesity or overweight with weight-related comorbidities. Nausea represents one of the most commonly reported adverse effects, particularly during treatment initiation and dose escalation phases. Understanding why this occurs can help patients manage the symptom more effectively.
The mechanism behind Wegovy-induced nausea relates to its pharmacological action. Semaglutide mimics the naturally occurring GLP-1 hormone, which slows gastric emptying—the rate at which food leaves the stomach and enters the small intestine. This delayed gastric emptying contributes to feelings of fullness and satiety, which supports weight loss, but can also trigger nausea, particularly when the stomach remains fuller for longer periods. Additionally, GLP-1 receptors are present in areas of the brain involved in nausea and vomiting responses, which may directly contribute to these symptoms.
Prevalence and typical patterns: Clinical trial data from the STEP programme indicates that approximately 44% of patients experience nausea with Wegovy, though severity varies considerably. Most patients find that nausea is most pronounced during the first few weeks of treatment or following dose increases. For many individuals, this adverse effect diminishes over time as the body adapts to the medication, typically within 4–8 weeks. However, persistent or severe nausea warrants medical review, as dose adjustment or alternative management strategies may be necessary to ensure treatment tolerability and adherence.
Importantly, if you experience severe, persistent upper abdominal pain with or without vomiting, you should stop taking Wegovy immediately and seek urgent medical attention, as this could indicate pancreatitis—a rare but serious adverse effect. Similarly, symptoms such as right upper abdominal pain, fever, yellowing of the skin/eyes, pale stools or dark urine could indicate gallbladder problems, which require prompt medical assessment.
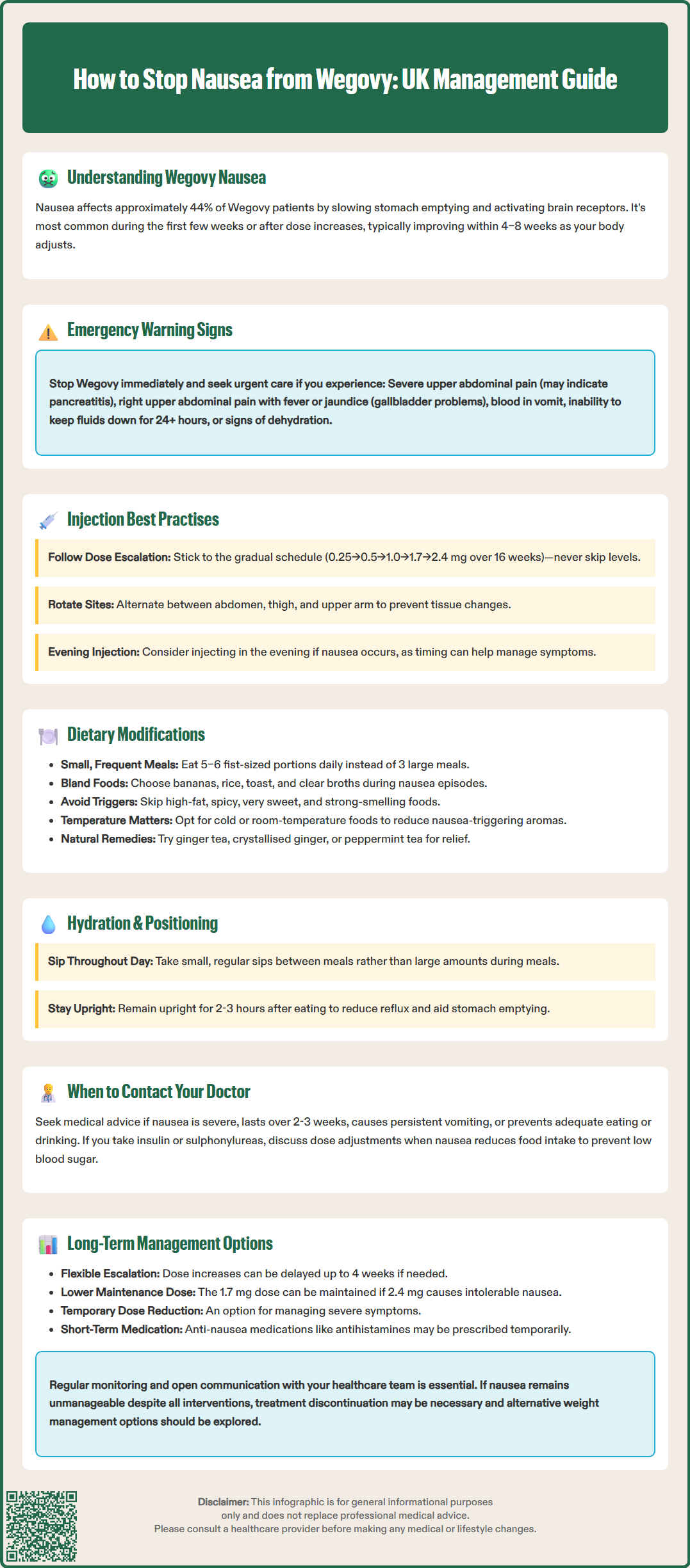
Several evidence-based strategies can help minimise nausea associated with Wegovy treatment. Gradual dose titration represents the cornerstone of nausea prevention. Wegovy is intentionally prescribed with a structured dose-escalation schedule, starting at 0.25 mg weekly and increasing gradually over 16 weeks to the maintenance dose of 2.4 mg (with each step: 0.25→0.5→1.0→1.7→2.4 mg). Adhering strictly to this schedule allows the gastrointestinal system time to adapt. If adverse effects occur, your clinician may delay dose escalation by up to 4 weeks. Patients should never skip dose levels or increase doses prematurely, as this significantly increases the risk of gastrointestinal adverse effects.
Injection timing and technique can also influence nausea severity. According to the Summary of Product Characteristics (SmPC), Wegovy can be administered at any time of day, with or without food. Some patients find that administering Wegovy in the evening helps them manage any nausea that occurs, though this is based on individual experience rather than clinical evidence. Ensuring proper injection technique—rotating injection sites between the abdomen, thigh, and upper arm—helps reduce local reactions and tissue changes that could affect absorption.
Hydration and meal timing play crucial roles in symptom management. Maintaining adequate fluid intake throughout the day helps prevent dehydration, which can exacerbate nausea. However, drinking large volumes immediately before or during meals may worsen symptoms due to increased gastric distension. Instead, focus on regular small sips between meals. Avoiding lying down immediately after eating (remaining upright for at least 2–3 hours post-meal) can reduce reflux and nausea by allowing gravity to assist gastric emptying. While evidence is limited specifically for subcutaneous semaglutide, some patients report that meal timing relative to injection affects their symptoms, so finding what works best for you may require some experimentation.
Targeted dietary adjustments represent one of the most effective non-pharmacological approaches to managing Wegovy-related nausea. Portion control and meal frequency are fundamental. Since semaglutide delays gastric emptying, consuming smaller, more frequent meals (5–6 small meals rather than 3 large ones) reduces the burden on the digestive system and minimises feelings of excessive fullness that trigger nausea. Each meal should be modest in size—roughly the size of a clenched fist as a practical rule of thumb—to avoid overwhelming the stomach's reduced emptying capacity.
Food composition and texture significantly influence tolerability. Bland, easily digestible foods are generally better tolerated during periods of nausea. Bland foods such as bananas, rice, apple purée, toast, plain crackers, and clear broths can provide a foundation, though nutritional adequacy must be maintained long-term. Conversely, certain foods commonly exacerbate nausea and should be limited or avoided:
High-fat foods (fried items, creamy sauces, fatty meats) delay gastric emptying further and increase nausea risk
Spicy or heavily seasoned dishes may irritate the gastric lining
Very sweet foods can trigger nausea in sensitive individuals
Strong-smelling foods may provoke nausea through olfactory triggers
Temperature and preparation methods also matter. Cold or room-temperature foods often produce less nausea-inducing aroma than hot meals. Ginger, in various forms (ginger tea, crystallised ginger, ginger biscuits), has natural anti-nausea properties that may provide symptomatic relief, though evidence for its effectiveness specifically with GLP-1 receptor agonist-related nausea is limited. Peppermint tea represents another traditional remedy that some patients find helpful, though evidence is more limited. These approaches can be tried alongside other management strategies but should not replace medical advice if symptoms persist.
While mild to moderate nausea is common and often manageable with self-care strategies, certain situations require prompt medical evaluation. Severe or persistent nausea that interferes significantly with daily activities, prevents adequate nutritional intake, or fails to improve after 2–3 weeks warrants contact with your prescribing clinician or GP. Persistent vomiting—particularly if occurring multiple times daily or lasting beyond a few days—requires medical assessment, as this can lead to dehydration and electrolyte imbalances.
Red flag symptoms that necessitate urgent medical attention include:
Severe abdominal pain, particularly if constant, sharp, or localised to the upper abdomen, which could indicate pancreatitis (a rare but serious adverse effect of GLP-1 receptor agonists). If you experience this, stop taking Wegovy immediately and seek urgent medical care.
Signs of dehydration: dark urine, dizziness, reduced urination, extreme thirst, or confusion
Inability to keep down fluids for more than 24 hours
Blood in vomit or vomit resembling coffee grounds
Unexplained fever accompanying nausea and vomiting
Rapid heart rate or feeling faint
Right upper abdominal pain, yellowing of skin/eyes, pale stools or dark urine which could indicate gallbladder problems
Patients with severe gastrointestinal disease including severe gastroparesis should maintain closer monitoring and lower thresholds for seeking advice, as Wegovy may exacerbate these conditions. People with diabetes taking insulin or sulfonylureas may need dose adjustments if nausea reduces food intake, to prevent hypoglycaemia. While semaglutide has minimal clinically relevant effects on the absorption of most oral medications, those taking medicines with a narrow therapeutic window (such as warfarin) should discuss monitoring requirements with their healthcare provider. Your clinician can assess whether dose reduction, temporary treatment interruption, or additional anti-nausea medication is appropriate, or whether alternative weight management strategies should be considered.
Report any suspected side effects to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
For most patients, nausea improves significantly with continued treatment as physiological adaptation occurs. However, individualised management strategies may be necessary for optimal long-term tolerability. Dose optimisation represents a key consideration. If nausea remains problematic despite dietary modifications and practical strategies, your prescribing clinician may recommend delaying dose escalation by up to 4 weeks, as outlined in the Wegovy Summary of Product Characteristics (SmPC). There is no requirement to reach the maximum 2.4 mg dose if a lower dose provides adequate weight loss with better tolerability. The SmPC acknowledges that 1.7 mg may be used as a maintenance dose if 2.4 mg is not tolerated.
In cases of severe nausea at any dose level, temporary dose adjustment may be appropriate. The SmPC provides guidance on dose management for tolerability issues. If nausea becomes intolerable, your clinician may recommend adjusting your dose according to the approved protocol. If lower doses are not tolerated, discontinuation of treatment may be considered.
Adjunctive anti-nausea medications may occasionally be prescribed for short-term use during particularly difficult periods, though this is not routinely recommended. Options might include antihistamines (such as cyclizine) or other antiemetics, prescribed at your doctor's discretion. These should be viewed as temporary measures whilst other management strategies take effect, rather than long-term solutions.
Monitoring and review should occur regularly, particularly during dose escalation phases. Patients should have regular reviews as agreed with their prescriber or service. Patients should maintain open communication with their healthcare team about symptom severity and impact on quality of life. If nausea remains unmanageable despite all interventions, discontinuation may be necessary, and alternative weight management approaches should be discussed. For NHS patients, it's worth noting that NICE guidance (TA875) specifies that semaglutide for weight management should be prescribed within specialist weight management services and treatment duration is subject to specific criteria. The goal is sustainable, tolerable treatment that supports long-term health outcomes without compromising quality of life.
Most patients find that Wegovy-related nausea improves within 4–8 weeks as the body adapts to treatment. Nausea is typically most pronounced during the first few weeks or following dose increases, then gradually diminishes with continued use.
Avoid high-fat foods (fried items, creamy sauces), spicy or heavily seasoned dishes, very sweet foods, and strong-smelling meals, as these can exacerbate nausea. Instead, opt for smaller portions of bland, easily digestible foods such as bananas, rice, toast, and clear broths.
Seek urgent medical attention if you experience severe abdominal pain, persistent vomiting lasting more than 24 hours, inability to keep down fluids, blood in vomit, signs of dehydration, or symptoms suggesting pancreatitis or gallbladder problems. Contact your GP if nausea significantly interferes with daily activities or fails to improve after 2–3 weeks.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.