
Mounjaro (tirzepatide) is a dual GIP/GLP-1 receptor agonist licensed in the UK for type 2 diabetes and weight management in specialist services. Gastric bypass surgery produces significant metabolic changes through similar incretin pathways. Patients who have undergone gastric bypass may consider Mounjaro for weight regain or persistent diabetes, but this combination requires careful clinical assessment. Whilst not absolutely contraindicated, using Mounjaro after gastric bypass is not routinely recommended without specialist guidance. This article examines the evidence, potential benefits, risks, and essential monitoring requirements for this complex clinical scenario.
Quick Answer: Mounjaro (tirzepatide) is not absolutely contraindicated after gastric bypass, but requires specialist assessment due to overlapping incretin mechanisms and limited evidence in post-bariatric populations.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMounjaro (tirzepatide) is a relatively new medication licensed in the UK for the treatment of type 2 diabetes mellitus and, more recently, for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. According to the NICE technology appraisal, NHS access to tirzepatide for weight management is restricted to specialist weight management services. Mounjaro belongs to a class of medicines known as dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonists. As described in the MHRA/EMC Summary of Product Characteristics (SmPC), Mounjaro works by mimicking the action of incretin hormones, which are naturally released after eating. These hormones help regulate blood glucose levels by stimulating insulin secretion, suppressing glucagon release, slowing gastric emptying, and reducing appetite through effects on the central nervous system.
Gastric bypass surgery, specifically Roux-en-Y gastric bypass (RYGB), is a well-established bariatric surgical procedure that involves creating a small stomach pouch and rerouting the small intestine. This anatomical alteration restricts food intake and reduces nutrient absorption, leading to significant weight loss. The procedure also produces profound metabolic changes, including alterations in gut hormone secretion—particularly increases in GLP-1 and other incretin hormones—which contribute to improved glycaemic control and appetite regulation.
Both interventions target weight management and metabolic health through overlapping mechanisms, particularly involving incretin pathways. Understanding how these treatments interact is essential for patients who have undergone gastric bypass and are considering additional pharmacological support for weight management or diabetes control. The decision to use Mounjaro after bariatric surgery requires careful clinical assessment, as the combined effects on gut hormone signalling and metabolic function may produce both benefits and potential complications that warrant thorough evaluation.
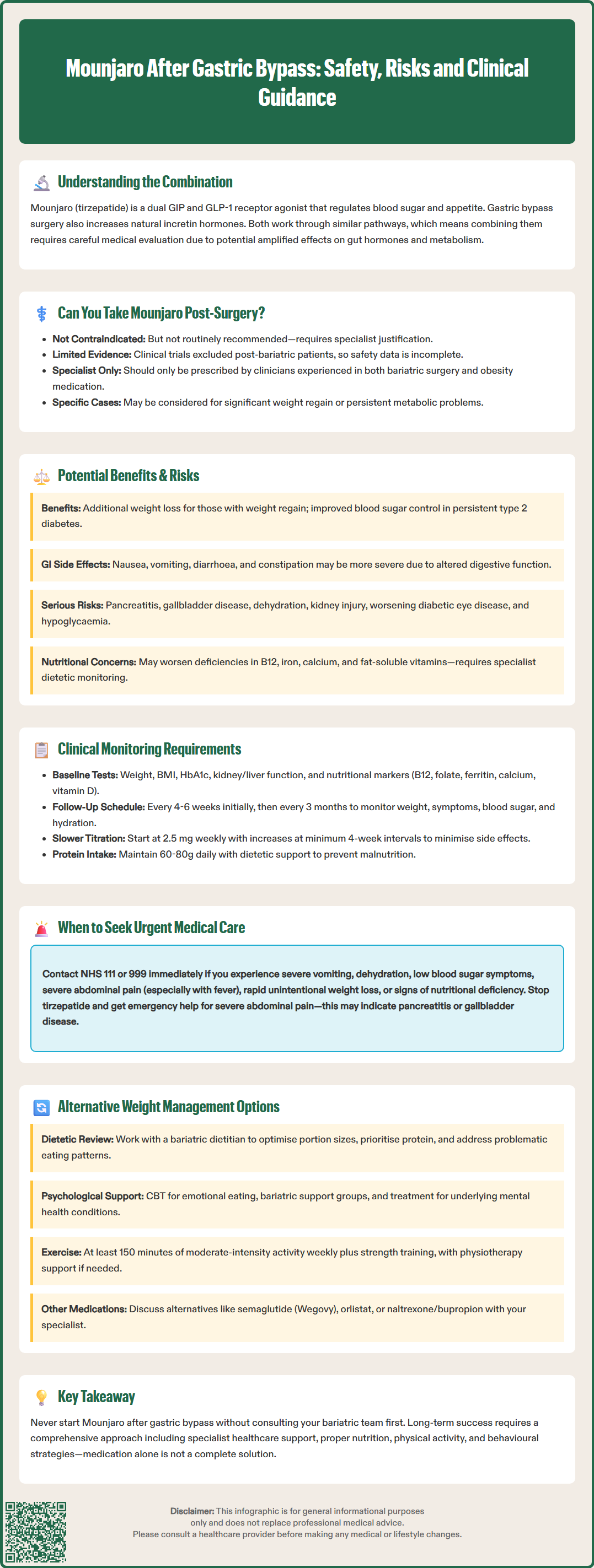
There is currently no absolute contraindication to using Mounjaro after gastric bypass surgery, but this combination is not routinely recommended without careful clinical justification. The Medicines and Healthcare products Regulatory Agency (MHRA) and the European Medicines Agency (EMA) have not issued specific warnings prohibiting tirzepatide use in post-bariatric surgery patients. However, the evidence base for this combination remains limited, as most clinical trials of Mounjaro specifically excluded individuals with previous bariatric procedures, as noted in the EMA European Public Assessment Report (EPAR).
The primary concern centres on the overlapping mechanisms of action. Gastric bypass surgery already produces substantial increases in endogenous GLP-1 and other incretin hormones, which contribute significantly to post-operative weight loss and metabolic improvements. Adding an exogenous GLP-1/GIP receptor agonist like Mounjaro may theoretically amplify these effects, though the clinical significance of this interaction is not fully characterised. Some patients who have experienced weight regain or inadequate glycaemic control following bariatric surgery may be considered for adjunctive pharmacotherapy, but this decision must be individualised.
The MHRA/EMC SmPC for tirzepatide includes relevant cautions that may be particularly important for post-bariatric patients, including use with caution in severe gastrointestinal disease, risk of pancreatitis, gallbladder disease, and dehydration potentially leading to acute kidney injury.
NICE guidance and the British Obesity and Metabolic Surgery Society (BOMSS) acknowledge that pharmacological interventions may have a role in selected post-bariatric surgery patients, particularly those with significant weight regain or persistent metabolic disease. However, such treatment should only be initiated by specialists with expertise in both bariatric surgery and obesity pharmacotherapy. The decision requires comprehensive assessment of the patient's surgical anatomy, nutritional status, current medications, and treatment goals. Patients should never initiate Mounjaro after gastric bypass without explicit guidance from their bariatric team or endocrinologist, as the safety profile in this specific population requires ongoing evaluation.
Potential benefits of using Mounjaro after gastric bypass may include additional weight loss in patients experiencing weight regain, which affects a significant proportion of bariatric surgery patients over time, with rates varying by procedure type and follow-up duration. For individuals with type 2 diabetes who have not achieved adequate glycaemic control despite surgical intervention, tirzepatide may provide supplementary glucose-lowering effects. The medication's appetite-suppressing properties could help reinforce dietary adherence and portion control, which are essential for long-term bariatric surgery success. Some patients may also experience improvements in cardiovascular risk factors, including blood pressure and lipid profiles, though these benefits must be weighed against potential risks.
Risks and adverse effects warrant careful consideration. The most common side effects of Mounjaro—nausea, vomiting, diarrhoea, and constipation—may be particularly problematic in post-gastric bypass patients who already experience altered gastrointestinal function. The combination of surgical anatomical changes and medication-induced delayed gastric emptying could potentially exacerbate gastrointestinal symptoms. There is a risk of hypoglycaemia, particularly in patients taking other glucose-lowering medications such as sulfonylureas or insulin. While tirzepatide itself has a glucose-dependent mechanism that limits intrinsic hypoglycaemia risk, post-bariatric patients may already have altered glucose metabolism and reactive hypoglycaemia that requires individualised management.
The MHRA/EMC SmPC highlights additional important safety concerns including:
Risk of pancreatitis (presenting as severe abdominal pain)
Gallbladder disease including cholelithiasis
Dehydration potentially leading to acute kidney injury
Potential worsening of diabetic retinopathy in patients with pre-existing disease, particularly with rapid glycaemic improvement
Nutritional considerations are paramount. According to BOMSS guidance, gastric bypass patients require lifelong vitamin and mineral supplementation due to malabsorption. The addition of Mounjaro, which can reduce food intake further, may increase the risk of protein-energy malnutrition and micronutrient deficiencies, including vitamin B12, iron, calcium, and fat-soluble vitamins. Specialist dietetic monitoring is essential to mitigate these risks.
Contraception and pregnancy: The SmPC states that tirzepatide may reduce the exposure to oral contraceptives. Women of childbearing potential should use non-oral contraception or add a barrier method for 4 weeks after initiating treatment or increasing the dose. Tirzepatide is not recommended during pregnancy or breastfeeding.
If Mounjaro is prescribed after gastric bypass surgery, comprehensive monitoring protocols must be established. Baseline assessments should include body weight, body mass index (BMI), glycated haemoglobin (HbA1c) for diabetic patients, full blood count, renal function (eGFR), liver function tests, and nutritional markers. In accordance with BOMSS guidance, these should include vitamin B12, folate, ferritin, calcium, vitamin D, parathyroid hormone (PTH), and magnesium levels. Additional tests such as thiamine (if vomiting is present) and trace elements (zinc, copper, selenium) may be indicated based on symptoms. A thorough medication review is essential to identify potential drug interactions and assess the need for dose adjustments of concurrent diabetes medications to minimise hypoglycaemia risk.
Regular follow-up appointments should be scheduled at 4-6 week intervals initially, then every 3 months once stable. At each visit, clinicians should assess:
Weight changes and rate of weight loss (sustained rapid weight loss with inability to meet nutritional needs requires urgent review)
Gastrointestinal symptoms, including severity and impact on quality of life
Glycaemic control through HbA1c monitoring and review of home glucose readings if applicable
Nutritional status via dietary intake assessment and repeat blood tests for vitamin and mineral levels
Hydration status and electrolyte balance, particularly sodium and potassium
Medication adherence and any barriers to treatment continuation
Dose titration of Mounjaro should be more cautious in post-bariatric surgery patients compared to standard protocols. According to the SmPC, treatment should start with 2.5 mg once weekly, with dose increases at intervals of at least 4 weeks. A slower titration approach may be appropriate in post-bariatric patients to minimise gastrointestinal side effects. Patients should be educated about recognising signs of dehydration, hypoglycaemia (tremor, sweating, confusion, palpitations), pancreatitis (severe abdominal pain), and severe gastrointestinal symptoms that warrant medical attention.
Patients should be advised to pause tirzepatide during periods of significant vomiting or diarrhoea ('sick days') and seek medical review. Dietetic input is strongly recommended to ensure adequate protein intake (60-80g daily) and appropriate supplementation. Any concerns about nutritional adequacy, persistent vomiting, or inability to maintain hydration should prompt immediate clinical review and consideration of treatment discontinuation.
Women of childbearing potential should be advised that tirzepatide may reduce oral contraceptive exposure; non-oral contraception or additional barrier methods are recommended for 4 weeks after initiation and each dose increase. Tirzepatide should be avoided in pregnancy and breastfeeding.
For patients experiencing weight regain or inadequate weight loss following gastric bypass, several alternative approaches should be considered before or alongside pharmacological interventions. Comprehensive dietary review with a specialist bariatric dietitian is fundamental, focusing on portion control, protein prioritisation, and identification of dietary patterns that may contribute to weight regain, such as grazing behaviour or consumption of high-calorie liquids. Structured meal planning and food diaries can help patients regain awareness of eating patterns and reinforce healthy behaviours established post-operatively.
Psychological support plays a crucial role in long-term bariatric surgery success. Many patients benefit from cognitive behavioural therapy (CBT) or other psychological interventions to address emotional eating, body image concerns, and behavioural factors contributing to weight regain. Bariatric support groups, whether in-person or online, provide peer support and shared strategies for maintaining weight loss. Addressing underlying mental health conditions, including depression and anxiety, which are more prevalent in bariatric surgery populations, is essential for optimising outcomes.
Physical activity programmes tailored to individual capabilities and preferences should be emphasised. The UK Chief Medical Officers' Physical Activity Guidelines recommend that adults engage in at least 150 minutes of moderate-intensity aerobic activity weekly, with additional strength training. For post-bariatric surgery patients, gradual progression under physiotherapy guidance may be beneficial, particularly for those with mobility limitations or musculoskeletal concerns.
Some patients may benefit from revisional bariatric surgery if anatomical complications such as gastric pouch enlargement or gastrojejunal anastomosis dilation are identified. According to BOMSS guidance, this option requires thorough investigation, including upper gastrointestinal endoscopy and contrast studies, and should only be considered after exhausting non-surgical interventions.
Other pharmacological options may include GLP-1 receptor agonists such as semaglutide (Wegovy), orlistat, or naltrexone/bupropion (Mysimba), though similar considerations regarding post-surgical use apply and specialist assessment is required. The choice of intervention should be individualised based on patient circumstances, preferences, and clinical assessment by the multidisciplinary bariatric team.
Patients who have undergone gastric bypass surgery should never initiate Mounjaro or any weight management medication without consulting their bariatric team or GP. If you are considering additional weight loss support, request a referral to your bariatric service or an endocrinologist with expertise in post-bariatric care. This is particularly important if you are experiencing significant weight regain (typically defined as regaining >25% of lost weight), persistent or recurrent type 2 diabetes despite surgical intervention, or concerns about your current weight management strategy.
Seek urgent medical attention (via NHS 111 or 999 if severe) if you experience any of the following whilst taking Mounjaro after gastric bypass:
Severe or persistent vomiting that prevents adequate fluid or nutrition intake
Signs of dehydration, including dark urine, dizziness, reduced urination, or extreme thirst
Symptoms of hypoglycaemia, such as trembling, sweating, confusion, rapid heartbeat, or loss of consciousness
Severe abdominal pain, particularly if accompanied by fever or vomiting, which could indicate pancreatitis or gallbladder disease (stop taking tirzepatide immediately)
Sustained rapid or unintentional weight loss with inability to meet nutritional or hydration needs
Signs of nutritional deficiency, including extreme fatigue, weakness, numbness or tingling in extremities, or cognitive changes
Routine consultations with your healthcare team should occur if you notice reduced effectiveness of the medication, intolerable side effects affecting quality of life, difficulty maintaining adequate protein or fluid intake, or any concerns about your nutritional status. Your bariatric team can arrange appropriate investigations, adjust treatment plans, and provide specialist dietetic and psychological support as needed.
If you experience any suspected side effects from Mounjaro, you can report these via the MHRA Yellow Card Scheme (website or app).
Remember that successful long-term weight management after gastric bypass requires ongoing engagement with your healthcare team, adherence to nutritional guidelines, regular physical activity, and behavioural strategies. Medication should be viewed as one component of a comprehensive, multidisciplinary approach rather than a standalone solution. Open communication with your healthcare providers ensures that any treatment decisions are made safely and in your best interests.
Mounjaro is not absolutely contraindicated after gastric bypass, but it requires specialist assessment and monitoring. The combination may amplify incretin effects and increase risks of gastrointestinal symptoms, nutritional deficiencies, and hypoglycaemia, so should only be initiated by bariatric specialists or endocrinologists.
Mounjaro may be considered for post-gastric bypass patients experiencing significant weight regain or persistent type 2 diabetes despite surgery. However, non-pharmacological approaches including dietetic review, psychological support, and physical activity should typically be optimised first.
Comprehensive monitoring includes regular assessment of weight, glycaemic control, gastrointestinal symptoms, hydration status, and nutritional markers (vitamin B12, folate, ferritin, calcium, vitamin D). Follow-up appointments should occur every 4-6 weeks initially, then every 3 months once stable, with specialist dietetic input.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.