
Mounjaro (tirzepatide) is a dual GIP/GLP-1 receptor agonist licensed in the UK for type 2 diabetes and weight management. Whilst the medication offers significant clinical benefits, some patients report experiencing a bad taste in the mouth during treatment. This taste disturbance, known as dysgeusia, may manifest as a metallic, bitter, or unpleasant flavour. Although not specifically listed in the UK Summary of Product Characteristics, anecdotal reports suggest this side effect can affect quality of life and medication adherence. Understanding the potential causes, management strategies, and when to seek medical advice is essential for patients taking Mounjaro.
Quick Answer: A bad taste in the mouth with Mounjaro (tirzepatide) is an uncommon side effect that may result from delayed gastric emptying causing reflux or from associated gastrointestinal symptoms like nausea.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMounjaro (tirzepatide) is a once-weekly injectable medication licensed in the UK for the treatment of type 2 diabetes mellitus. It is also licensed for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity, as an adjunct to diet and exercise. UK NHS access for weight management follows NICE guidance (TA1026). As a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist, Mounjaro works by enhancing insulin secretion, suppressing glucagon release, and slowing gastric emptying. These mechanisms help improve glycaemic control and promote weight loss.
Whilst Mounjaro has demonstrated significant clinical benefits in trials, patients may experience various side effects during treatment. Among the less commonly discussed adverse effects is dysgeusia—an alteration in taste perception that can manifest as a persistent bad, metallic, or bitter taste in the mouth. Dysgeusia is not specifically listed in the UK Summary of Product Characteristics (SmPC) for tirzepatide, though it has been reported anecdotally by some patients. However, low-frequency dysgeusia has been reported in other sources (e.g., “change in taste” in some international product information and pooled trial summaries).
Taste disturbances can significantly impact quality of life, affecting appetite, nutritional intake, and medication adherence. Understanding why these changes might occur, how common they are, and what can be done to manage them is essential for patients and healthcare professionals alike. This article provides guidance on taste alterations that may be associated with Mounjaro, helping patients navigate this potential side effect whilst continuing their treatment safely and effectively.
The exact mechanism by which Mounjaro might cause taste disturbances is not established, as there is no direct link confirmed in clinical trial data or the UK SmPC. However, several hypothetical explanations exist based on the drug's pharmacological actions.
Delayed gastric emptying is one of Mounjaro's documented mechanisms of action. By slowing the rate at which food leaves the stomach, the medication may potentially lead to gastro-oesophageal reflux in some patients. This reflux could bring stomach acid and partially digested food back into the oesophagus and mouth, creating an unpleasant metallic or bitter taste. Patients with pre-existing reflux symptoms may be particularly susceptible to this effect.
Gastrointestinal side effects such as nausea, vomiting, and indigestion—which are common with Mounjaro according to the SmPC—can also contribute to taste alterations. Nausea itself can be associated with changes in taste perception, and frequent episodes of reflux or regurgitation may leave a lingering bad taste.
Other potential factors to consider include:
Concomitant medications: Some commonly prescribed medications, such as metformin (often taken alongside Mounjaro for diabetes), can cause metallic taste as a recognised side effect.
Oral health issues: Reduced food intake or changes in eating patterns might affect oral hygiene, potentially contributing to taste changes.
Metabolic changes: Significant caloric restriction may lead to metabolic adaptations that could theoretically affect taste perception.
It's important to note that if you experience symptoms of diabetic ketoacidosis (excessive thirst, frequent urination, nausea, abdominal pain, confusion, unusual fatigue, or fruity-smelling breath), seek immediate medical attention, particularly if you are also taking an SGLT2 inhibitor medication.
Determining the precise incidence of taste disturbances with Mounjaro is challenging, as dysgeusia is not specifically listed as an adverse reaction in the UK Summary of Product Characteristics (SmPC) for tirzepatide. The pivotal SURPASS trials, which evaluated tirzepatide for type 2 diabetes, and the SURMOUNT trials for weight management, focused primarily on more common adverse events.
According to the UK SmPC, gastrointestinal adverse events are very common with Mounjaro treatment. These include:
Nausea (reported in 11.9-24.0% of patients, depending on dose)
Diarrhoea (13.3-22.1%)
Vomiting (4.9-10.5%)
Constipation (5.3-9.1%)
These symptoms, which can indirectly contribute to taste changes, were generally mild to moderate in severity and tended to decrease over time as patients became accustomed to the medication. Reported rates vary by dose and indication (type 2 diabetes vs. obesity cohorts).
Anecdotal reports from patient forums suggest that some individuals do experience a bad or altered taste whilst taking Mounjaro, though this appears to be relatively uncommon compared to the more frequently reported gastrointestinal effects. While dysgeusia has been documented with some other GLP-1 receptor agonists, the evidence for this being a consistent class effect is limited.
If you experience persistent taste changes while taking Mounjaro, it's worth discussing this with your healthcare professional. They can help determine whether the taste disturbance is related to your medication or might have another cause, such as oral health issues or other medications you may be taking.
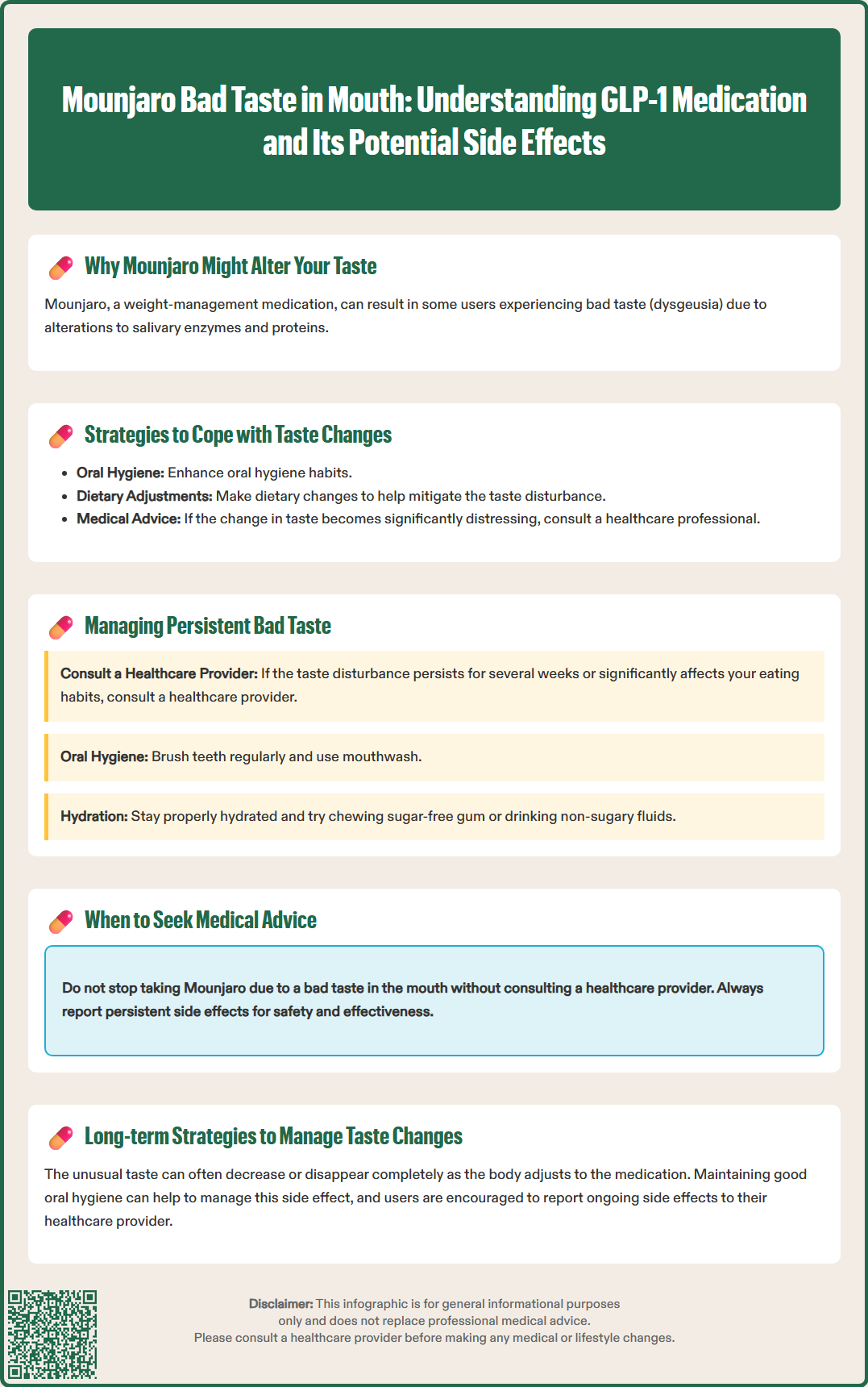
If you are experiencing a bad taste in your mouth whilst taking Mounjaro, several practical strategies may help alleviate this symptom and improve your comfort during treatment.
Maintain excellent oral hygiene: Brush your teeth at least twice daily with fluoride toothpaste, and consider brushing your tongue gently to remove bacteria and debris that may contribute to taste disturbances. Using an antibacterial mouthwash can also help, though avoid alcohol-based products if they cause mouth dryness. Regular flossing and dental check-ups are important for overall oral health.
Stay well hydrated: Drinking plenty of water throughout the day can help rinse away unpleasant tastes and keep your mouth fresh. Sipping water regularly may also help manage nausea, which can be associated with taste changes. Aim for at least 1.5–2 litres of fluid daily, unless you have heart, liver or kidney disease, in which case follow your healthcare provider's specific advice about fluid intake.
Try sugar-free mints or gum: Chewing sugar-free gum or sucking on sugar-free mints can stimulate saliva production and mask bad tastes. Opt for mint, citrus, or cinnamon flavours, which many people find particularly effective. Ensure products are sugar-free to avoid affecting blood glucose levels. Be aware that excessive consumption of sugar alcohols (often found in sugar-free products) may worsen diarrhoea in some people.
Address gastro-oesophageal reflux: If reflux is contributing to the bad taste, lifestyle modifications can help. These include eating smaller, more frequent meals; avoiding lying down within three hours of eating; elevating the head of your bed; and limiting trigger foods such as spicy dishes, caffeine, alcohol, and fatty meals. If symptoms persist, speak to your GP about appropriate antacid medications.
Consider dietary adjustments: Some patients find that certain foods help neutralise bad tastes. Tart or citrus fruits (if tolerated), fresh vegetables, and cold foods may be more palatable. Avoid foods that seem to worsen the taste disturbance.
If you experience any side effects, including taste disturbances, that are troublesome or persistent, report them to your healthcare professional. You can also report suspected side effects directly via the Yellow Card Scheme at yellowcard.mhra.gov.uk.
Whilst taste disturbances potentially associated with Mounjaro are generally benign and self-limiting, certain circumstances warrant prompt medical attention. It is important to recognise when taste changes might indicate a more serious underlying issue or when they significantly impact your health and wellbeing.
Seek advice from your GP or diabetes specialist nurse if:
The bad taste persists for more than a few weeks despite trying self-management strategies
Taste changes are accompanied by severe or persistent nausea and vomiting that prevents you from eating or drinking adequately
You experience significant unintended weight loss beyond your treatment goals
The taste disturbance is associated with signs of dehydration (dark urine, dizziness, reduced urination)
You develop new symptoms such as abdominal pain, difficulty swallowing, or persistent heartburn
The taste change is accompanied by oral symptoms such as mouth ulcers, swelling, or white patches on the tongue
You experience symptoms of hypoglycaemia (particularly if you also take insulin or sulfonylureas), as reduced food intake may increase this risk
Seek urgent medical attention if you experience:
Severe abdominal pain (which could suggest pancreatitis, a rare but serious side effect of GLP-1 receptor agonists)
Persistent vomiting leading to dehydration
Signs of an allergic reaction (rash, swelling of the face or throat, difficulty breathing)
Severe pain in the upper right side of your abdomen, possibly with fever or yellowing of the skin/eyes (potential signs of gallbladder disease, which can be associated with GLP-1 receptor agonists)
Your healthcare provider can assess whether the taste disturbance is related to Mounjaro or might have another cause, such as oral infection, medication interactions, or nutritional deficiencies. They may recommend adjusting your dose, temporarily pausing treatment, or switching to an alternative medication if the symptom is significantly affecting your quality of life. Never stop taking Mounjaro without consulting your healthcare team, as abrupt discontinuation may affect your diabetes control or weight management progress.
Remember to report suspected adverse reactions to Mounjaro via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Beyond potential taste disturbances, Mounjaro is associated with a range of gastrointestinal side effects that patients should be aware of. Understanding these potential adverse effects can help you prepare for treatment and recognise when symptoms require medical attention.
Gastrointestinal side effects are the most commonly reported adverse events with Mounjaro. According to the UK SmPC, these include:
Nausea: Very common, affecting 11.9-24.0% of patients (dose-dependent), particularly during the initial weeks of treatment or following dose increases. Nausea typically improves over time as the body adjusts.
Diarrhoea: Very common (13.3-22.1%), this can usually be managed with dietary modifications and adequate hydration.
Vomiting: Common (4.9-10.5%), particularly at higher doses.
Constipation: Common (5.3-9.1%) and may be managed with increased fibre intake, hydration, and physical activity.
Abdominal pain and dyspepsia: These symptoms can range from mild discomfort to more significant pain requiring medical assessment.
Decreased appetite: Whilst this contributes to weight loss, some patients may find the reduction in appetite excessive or uncomfortable.
While dry mouth (xerostomia) is not specifically listed in the UK SmPC for tirzepatide, some patients may experience this symptom, which could potentially contribute to taste changes. Maintaining good oral hygiene and staying hydrated are essential preventive measures.
Rare but serious gastrointestinal complications include acute pancreatitis, which has been reported with GLP-1 receptor agonists. Symptoms include severe, persistent abdominal pain that may radiate to the back, often accompanied by nausea and vomiting. This requires immediate medical attention.
Hypoglycaemia risk is increased when Mounjaro is used in combination with insulin or sulfonylureas. If you are taking these medications, your doctor may need to reduce their doses when starting Mounjaro, and you should monitor your blood glucose levels carefully.
According to NICE guidance (TA859), patients starting Mounjaro should be counselled about expected side effects and provided with strategies to manage them. Most gastrointestinal symptoms are dose-dependent and can be minimised by following the recommended dose escalation schedule, which allows the body to gradually adapt to the medication. If side effects become intolerable, your healthcare provider may recommend slowing the dose escalation or maintaining a lower dose that provides benefit with acceptable tolerability.
Mounjaro may cause a bad taste through delayed gastric emptying leading to reflux, or indirectly through common gastrointestinal side effects like nausea and vomiting. The exact mechanism is not fully established, as dysgeusia is not specifically listed in the UK Summary of Product Characteristics.
Maintain excellent oral hygiene by brushing teeth and tongue twice daily, stay well hydrated with 1.5-2 litres of water daily, use sugar-free mints or gum, and address reflux through lifestyle modifications such as eating smaller meals and avoiding lying down within three hours of eating.
Contact your GP if the bad taste persists for more than a few weeks despite self-management, is accompanied by severe nausea or vomiting, causes significant unintended weight loss, or is associated with new symptoms such as abdominal pain or difficulty swallowing.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.