
Mounjaro (tirzepatide) is a dual GIP/GLP-1 receptor agonist licensed in the UK for type 2 diabetes and weight management. Emerging evidence suggests potential benefits for metabolic dysfunction-associated steatotic liver disease (MASLD), formerly known as non-alcoholic fatty liver disease. Whilst not currently licensed for fatty liver treatment, Mounjaro's effects on weight loss and metabolic parameters have generated interest in its application for liver health. This article examines the clinical evidence, eligibility criteria, safety considerations, and alternative approaches for patients with fatty liver disease considering Mounjaro therapy.
Quick Answer: Mounjaro is not currently licensed in the UK specifically for fatty liver disease, though emerging clinical evidence suggests it may improve liver health markers in patients who meet criteria for its approved indications of type 2 diabetes or weight management.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMounjaro (tirzepatide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus and, more recently, for weight management in adults with obesity or overweight with weight-related comorbidities. It belongs to a novel class of medications known as dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonists. This dual mechanism distinguishes Mounjaro from other GLP-1 receptor agonists currently available.
The medicine works by mimicking two naturally occurring incretin hormones that play crucial roles in glucose regulation and appetite control. GLP-1 stimulates insulin secretion when blood glucose levels are elevated, suppresses glucagon release (which reduces glucose production by the liver), slows gastric emptying, and promotes satiety. GIP also enhances insulin secretion and may influence fat metabolism and energy expenditure. By activating both pathways simultaneously, tirzepatide produces robust effects on glycaemic control and body weight reduction.
Mounjaro is administered as a once-weekly subcutaneous injection, typically in the abdomen, thigh, or upper arm. According to the MHRA/EMC Summary of Product Characteristics (SmPC), the dose is gradually increased over several weeks to minimise gastrointestinal side effects, starting at 2.5 mg weekly for 4 weeks, then 5 mg weekly for 4 weeks, with potential further increases to 10 mg and 15 mg weekly at 4-week intervals, depending on individual response and tolerability.
While the MHRA has licensed tirzepatide for weight management (BMI ≥30 kg/m² or ≥27 kg/m² with comorbidity), NHS-funded access is restricted under NICE Technology Appraisal criteria to patients meeting specific eligibility requirements and treated within specialist weight management services.
The medication's effects on weight loss and metabolic parameters have generated considerable interest in its potential application for metabolic dysfunction-associated steatotic liver disease (MASLD, formerly known as non-alcoholic fatty liver disease or NAFLD), though this is not currently a licensed indication in the UK.
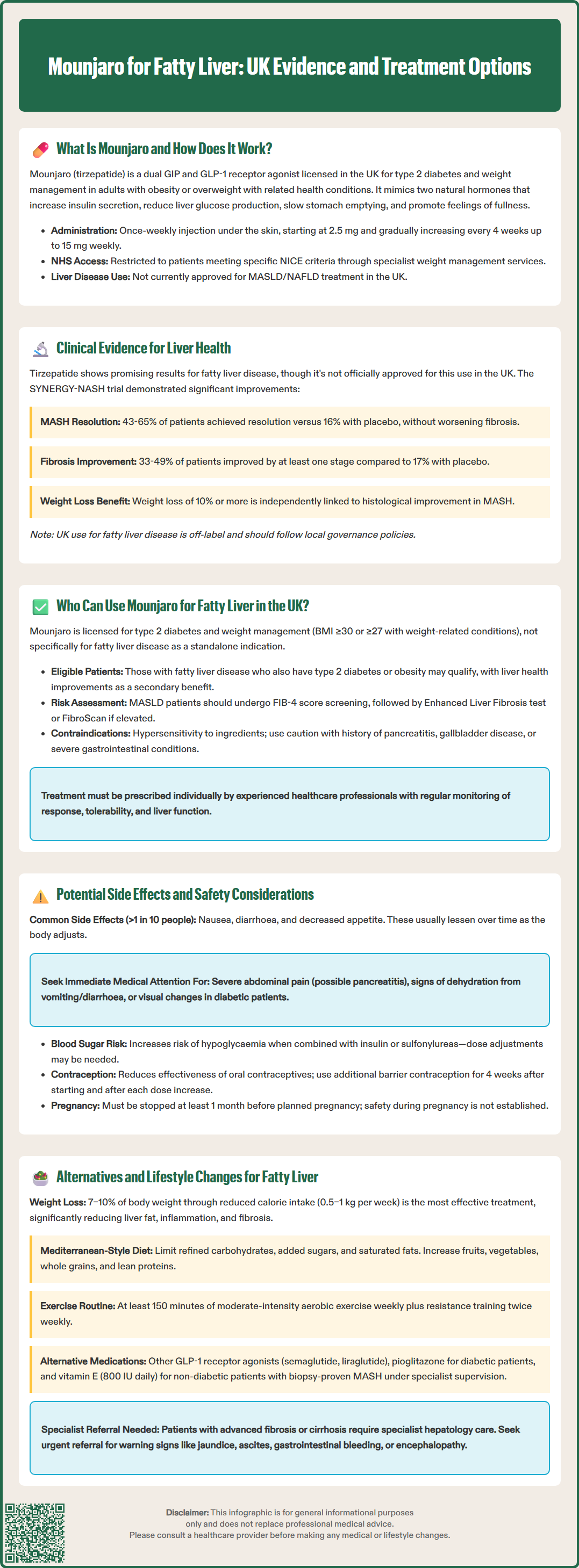
Emerging clinical evidence suggests that tirzepatide may offer benefits for patients with fatty liver disease, though it is important to note that Mounjaro is not currently licensed specifically for this indication in the UK. The rationale for its potential use stems from the established link between obesity, insulin resistance, type 2 diabetes, and the development and progression of MASLD (formerly NAFLD).
In clinical trials evaluating tirzepatide for diabetes (SURPASS programme) and weight management (SURMOUNT programme), secondary analyses have demonstrated improvements in liver-related biomarkers. Studies have shown reductions in liver enzymes such as alanine aminotransferase (ALT) and aspartate aminotransferase (AST), which are commonly elevated in patients with fatty liver disease. Additionally, non-invasive markers of liver fibrosis and steatosis have shown improvement in patients treated with tirzepatide. It should be noted that these were secondary or exploratory endpoints and not substitutes for histological assessment.
The SYNERGY-NASH phase 2 trial published in the New England Journal of Medicine in 2024 specifically examined tirzepatide's effects on biopsy-confirmed metabolic dysfunction-associated steatohepatitis (MASH, previously known as NASH). Results indicated that tirzepatide at doses of 5 mg, 10 mg, and 15 mg led to significant reductions in liver fat content compared to placebo. MASH resolution without worsening of fibrosis was achieved in 42.9% to 64.5% of patients receiving tirzepatide (depending on dose) versus 15.6% with placebo. Improvement in fibrosis of at least one stage without worsening of MASH was observed in 32.9% to 48.6% of tirzepatide-treated patients versus 17.2% with placebo.
Weight loss of 10% or more, which is frequently achieved with tirzepatide therapy, has been independently associated with histological improvement in MASH.
However, it is crucial to emphasise that there is no official MHRA or NICE approval for using Mounjaro specifically to treat fatty liver disease at present. Use of tirzepatide for MASLD/MASH would be considered off-label in the UK and should follow local governance policies. Clinicians may consider tirzepatide for patients with fatty liver disease who also have type 2 diabetes or meet criteria for weight management therapy, addressing multiple metabolic risk factors simultaneously.
In the UK, Mounjaro is currently licensed for two specific indications: the treatment of adults with insufficiently controlled type 2 diabetes mellitus as an adjunct to diet and exercise, and for weight management in adults with a body mass index (BMI) of 30 kg/m² or greater, or 27 kg/m² or greater with at least one weight-related comorbidity. It is not formally licensed for the treatment of fatty liver disease as a standalone indication.
For NHS-funded weight management treatment, NICE Technology Appraisal guidance restricts access to patients meeting specific criteria, treated within specialist weight management services, and typically for a defined treatment period. Patients should discuss eligibility with their healthcare provider.
Many patients with MASLD also have type 2 diabetes, obesity, or both conditions, which means they may be eligible for Mounjaro under its current licensed indications. If a patient with fatty liver disease meets the criteria for either diabetes treatment or weight management, their clinician may prescribe Mounjaro, with the understanding that improvements in liver health may occur as a beneficial secondary effect. Use specifically for fatty liver disease would be considered off-label and should be justified by meeting licensed indications and local policies.
According to NICE guideline NG49 and British Society of Gastroenterology guidance, patients with suspected MASLD should undergo risk stratification. This typically involves calculating the FIB-4 score; if this is ≥1.3 (for those under 65 years) or ≥2.0 (for those 65 years or older), second-line testing with Enhanced Liver Fibrosis (ELF) test or FibroScan/VCTE should be arranged. Referral to hepatology is recommended for those at high risk of advanced fibrosis or if red flags are present (e.g., jaundice, splenomegaly, low platelets, signs of decompensation).
Prescribing decisions should be made on an individual basis following comprehensive assessment. According to the UK SmPC, contraindications to tirzepatide include hypersensitivity to the active substance or any of the excipients. Caution is advised in patients with a history of pancreatitis, gallbladder disease, or severe gastrointestinal disease including gastroparesis. The SmPC notes that thyroid C-cell tumours have been observed in animal studies, though the relevance to humans is unknown.
Patients should be informed that while Mounjaro may improve liver health markers, this is not its primary licensed purpose, and treatment should be initiated and monitored by healthcare professionals experienced in managing metabolic conditions. Regular follow-up is essential to assess treatment response, tolerability, and any changes in liver function tests or imaging findings.
Like all medicines, Mounjaro can cause side effects, though not everyone experiences them. According to the MHRA/EMC SmPC, the most commonly reported adverse effects are gastrointestinal in nature and typically occur during the initial weeks of treatment or following dose increases. These include:
Nausea (very common: may affect more than 1 in 10 people)
Diarrhoea (very common) and constipation (common: may affect up to 1 in 10 people)
Vomiting (common) and abdominal pain (common)
Decreased appetite (very common) and dyspepsia (common)
These symptoms are usually mild to moderate and tend to diminish over time as the body adjusts to the medication. Taking the injection at the same time each week and eating smaller, more frequent meals may help manage these effects.
More serious but less common side effects include acute pancreatitis, which presents with severe, persistent abdominal pain that may radiate to the back. Patients experiencing such symptoms should seek immediate medical attention and discontinue Mounjaro. The SmPC includes a precaution regarding thyroid C-cell tumours observed in animal studies, though the relevance to humans is unknown.
Other important safety considerations include:
Hypoglycaemia risk, particularly when used alongside insulin or sulfonylureas (dose adjustments of these medications may be necessary)
Gallbladder problems, including cholelithiasis and cholecystitis
Diabetic retinopathy complications in patients with pre-existing eye disease
Acute kidney injury, especially in patients who become dehydrated from gastrointestinal side effects
Tirzepatide can reduce the exposure to oral contraceptives during initiation and after each dose increase. Women using oral contraceptives are advised to use barrier methods for 4 weeks after starting treatment and for 4 weeks after each dose escalation.
Patients should contact their GP or healthcare provider if they experience persistent vomiting or diarrhoea, signs of dehydration, severe abdominal pain, visual changes, or symptoms of an allergic reaction. Monitoring of relevant clinical parameters should be conducted based on individual patient needs and comorbidities.
Women of childbearing potential should use effective contraception during treatment, and tirzepatide should be discontinued at least 1 month before a planned pregnancy, as the safety of tirzepatide in pregnancy has not been established.
Patients are encouraged to report any suspected side effects via the MHRA Yellow Card scheme (website: yellowcard.mhra.gov.uk or search for 'MHRA Yellow Card' in the Google Play or Apple App Store).
While medications like Mounjaro may offer benefits for certain patients, lifestyle modification remains the cornerstone of managing fatty liver disease according to NICE guideline NG49 and British Society of Gastroenterology guidance. Evidence consistently demonstrates that weight loss of 7–10% of body weight can significantly reduce liver fat, inflammation, and even fibrosis in patients with MASLD.
Dietary interventions should focus on:
Reducing overall calorie intake to achieve gradual, sustainable weight loss (0.5–1 kg per week)
Limiting refined carbohydrates, added sugars, and sugar-sweetened beverages
Reducing saturated fat intake and avoiding trans fats
Increasing consumption of fruits, vegetables, whole grains, and lean proteins
Following a Mediterranean-style diet, which has shown particular benefit for liver health
Moderating or eliminating alcohol consumption, even in "non-alcoholic" fatty liver disease
Physical activity is equally important. NICE recommends at least 150 minutes of moderate-intensity aerobic exercise weekly, combined with resistance training on two or more days. Even without significant weight loss, regular exercise can reduce liver fat and improve insulin sensitivity.
Bariatric/metabolic surgery is an effective option for eligible patients with severe obesity, according to NICE obesity guidance, and has been shown to improve MASLD/MASH in appropriate candidates.
Pharmacological alternatives to Mounjaro for patients with fatty liver disease include other GLP-1 receptor agonists (such as semaglutide or liraglutide), which have similar metabolic benefits. For patients with type 2 diabetes, pioglitazone has demonstrated improvements in liver histology, though weight gain and other side effects limit its use. Vitamin E (at high doses of 800 IU daily) has shown benefit in non-diabetic patients with biopsy-proven MASH, though long-term safety data are limited and it should be used under specialist supervision.
Management of comorbidities is essential: optimising control of diabetes, hypertension, and dyslipidaemia all contribute to better liver outcomes. Statins are safe in fatty liver disease and should be used when indicated for cardiovascular risk reduction.
Patients with advanced fibrosis or cirrhosis require specialist hepatology input and regular surveillance for complications including hepatocellular carcinoma. Urgent or specialist referral is indicated for red flags such as jaundice, ascites, gastrointestinal bleeding, encephalopathy, or rapidly rising bilirubin/INR. Ultimately, a multidisciplinary approach combining lifestyle intervention, appropriate pharmacotherapy, and specialist monitoring when needed offers the best outcomes for patients with fatty liver disease.
No, Mounjaro is not currently licensed specifically for fatty liver disease in the UK. It is approved for type 2 diabetes and weight management, though patients with fatty liver who meet these criteria may benefit from improvements in liver health as a secondary effect.
The SYNERGY-NASH trial showed that tirzepatide achieved MASH resolution in 42.9–64.5% of patients versus 15.6% with placebo, with improvements in liver fat content and fibrosis. Secondary analyses from diabetes and weight management trials have also demonstrated reductions in liver enzymes and non-invasive markers of liver disease.
The most common side effects are gastrointestinal, including nausea, diarrhoea, vomiting, and abdominal pain, typically occurring during initial treatment or dose increases. More serious but less common risks include pancreatitis, gallbladder disease, and hypoglycaemia when used with certain diabetes medications.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.