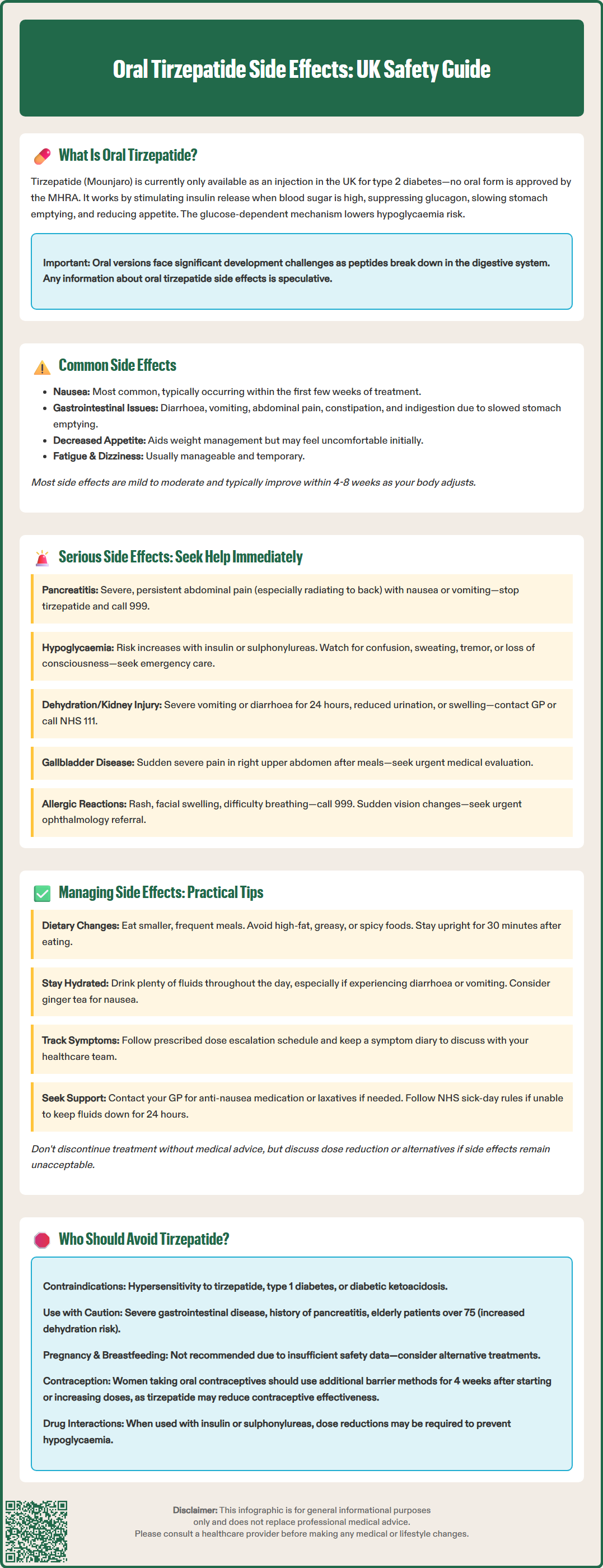
Oral tirzepatide side effects are a topic of growing interest, though it is crucial to understand that no oral formulation of tirzepatide is currently authorised by the MHRA in the UK. Tirzepatide (Mounjaro) is presently available only as an injectable treatment for type 2 diabetes. Any discussion of oral tirzepatide side effects is therefore based on extrapolation from the established safety profile of injectable tirzepatide and the broader class of GLP-1 receptor agonists. This article examines the potential side effects, serious adverse events, practical management strategies, and contraindications that would likely apply to any future oral formulation.
Quick Answer: No oral tirzepatide formulation is currently authorised in the UK; side effect information is extrapolated from injectable tirzepatide (Mounjaro).

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereTirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist, currently available in the UK only as an injectable formulation (Mounjaro) for type 2 diabetes management. It is important to note that an oral formulation of tirzepatide is not currently authorised by the MHRA in the UK.
The mechanism of action of tirzepatide involves stimulating insulin secretion in a glucose-dependent manner, meaning insulin release occurs primarily when blood glucose levels are elevated, thereby reducing the risk of hypoglycaemia. Simultaneously, tirzepatide suppresses glucagon secretion, slows gastric emptying, and promotes satiety through central nervous system pathways. These combined effects result in improved glycaemic control and significant weight reduction, which is particularly beneficial given the strong association between obesity and type 2 diabetes.
Research into oral peptide delivery systems is ongoing in the pharmaceutical industry, as GLP-1 receptor agonists have traditionally required subcutaneous injection due to poor oral bioavailability. Any future oral tirzepatide formulation would need to overcome the challenges of peptide degradation in the gastrointestinal tract.
As no oral tirzepatide formulation is currently authorised in the UK, the following information is based on the established safety profile of injectable tirzepatide (Mounjaro) and the class effects of GLP-1 receptor agonists. Any future oral formulation would likely share similar systemic effects, though the gastrointestinal profile might differ.
The most frequently reported side effects of injectable tirzepatide include:
Nausea – often the most common complaint, typically occurring within the first few weeks of treatment
Diarrhoea – loose or frequent bowel movements affecting a significant proportion of patients
Vomiting – may occur alongside nausea, particularly if dietary modifications are not implemented
Decreased appetite – whilst therapeutically beneficial for weight management, some patients find this uncomfortable
Abdominal discomfort or pain – ranging from mild bloating to cramping sensations
Constipation – paradoxically, some patients experience reduced bowel frequency
Dyspepsia – indigestion or upper abdominal discomfort
These gastrointestinal effects result directly from the medication's mechanism of slowing gastric emptying and altering gut motility. According to the MHRA-approved Summary of Product Characteristics (SmPC) for injectable tirzepatide, these effects are generally mild to moderate in severity and tend to diminish over time as the body adapts to the medication.
Other common side effects observed with injectable tirzepatide include fatigue and dizziness. Most patients find these effects manageable and temporary, with symptoms typically improving after the first 4–8 weeks of treatment. However, if side effects persist or significantly impact quality of life, patients should consult their GP or diabetes specialist nurse for guidance on dose adjustment or alternative management strategies. For urgent but non-emergency concerns, NHS 111 can provide advice.
Whilst most side effects of tirzepatide are mild and self-limiting, certain serious adverse events require immediate medical attention. Patients and carers should be educated about these warning signs before commencing treatment.
Pancreatitis represents one of the most concerning potential complications associated with GLP-1 receptor agonists. Symptoms include severe, persistent abdominal pain (often radiating to the back), nausea, vomiting, and fever. This constitutes a medical emergency requiring immediate assessment in A&E or by calling 999. According to the MHRA-approved SmPC, patients should discontinue tirzepatide if pancreatitis is suspected, and if confirmed, treatment should not be restarted.
Severe hypoglycaemia is uncommon with tirzepatide monotherapy due to its glucose-dependent mechanism, but risk increases substantially when combined with insulin or sulphonylureas. Warning signs include confusion, sweating, tremor, palpitations, and loss of consciousness. Patients should be advised about hypoglycaemia recognition and management, including when to call 999.
Acute kidney injury may occur, particularly in patients experiencing severe vomiting or diarrhoea leading to dehydration. Symptoms include reduced urine output, swelling of ankles or legs, and unusual fatigue. Patients with pre-existing renal impairment require careful monitoring.
Gallbladder disease, including cholecystitis and cholelithiasis, has been reported with GLP-1 receptor agonists. Sudden onset of severe right upper quadrant pain, particularly after meals, warrants urgent medical evaluation.
Allergic reactions, though rare, may manifest as rash, itching, swelling (particularly of face, lips, or throat), or difficulty breathing. Anaphylaxis requires immediate emergency treatment by calling 999.
Diabetic retinopathy complications have been observed in some patients with pre-existing retinopathy experiencing rapid glycaemic improvement. This is related to the speed of HbA1c reduction rather than a direct drug effect. Any sudden changes in vision should prompt urgent ophthalmology referral.
Patients should contact their GP promptly or call NHS 111 if experiencing persistent vomiting (unable to keep fluids down for 24 hours), signs of dehydration, severe abdominal pain, or any symptoms causing significant concern. Suspected side effects should be reported via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Effective side effect management can significantly improve treatment adherence and patient outcomes. Healthcare professionals should provide comprehensive counselling, and patients should feel empowered to implement practical strategies.
For gastrointestinal side effects:
Eat smaller, more frequent meals rather than three large meals daily
Avoid high-fat, greasy, or spicy foods, which may exacerbate nausea and slow digestion further
Stay well hydrated, sipping water throughout the day, particularly if experiencing diarrhoea or vomiting
Eat slowly and chew thoroughly to reduce feelings of fullness and discomfort
Avoid lying down immediately after eating; remain upright for at least 30 minutes
Consider ginger tea for nausea, but consult your pharmacist before taking ginger supplements, especially if you take anticoagulants or other medications
Take the medication as directed regarding timing with food, as this may influence tolerability
General management strategies:
Gradual dose escalation is standard practice to minimise side effects; never increase the dose faster than prescribed
Keep a symptom diary to identify patterns and triggers, which can inform discussions with your healthcare team
Maintain regular contact with your diabetes specialist nurse or GP, particularly during the first three months
Don't discontinue treatment abruptly without medical advice; many side effects improve with time
Review concomitant medications with your pharmacist, as some may worsen gastrointestinal symptoms
For specific concerns:
If nausea is severe, your GP may prescribe anti-emetic medication for short-term use. For persistent constipation, appropriate laxatives can be recommended. Follow NHS sick-day rules if you're unwell: maintain hydration, seek advice if unable to keep fluids down for 24 hours, and contact your diabetes team about whether to temporarily adjust or pause your medication.
Patients experiencing significant side effects despite these measures should discuss dose reduction or alternative treatment options with their diabetes team. NICE guidance emphasises individualised treatment approaches, and no patient should feel obligated to continue a medication causing unacceptable side effects when alternatives exist. For urgent but non-emergency advice, contact NHS 111.
Based on the current MHRA-approved SmPC for injectable tirzepatide (Mounjaro), the following guidance would likely apply to any future oral formulation, though specific contraindications may differ if such a product is eventually authorised.
Contraindications:
Not indicated for use in:
Type 1 diabetes mellitus – tirzepatide is not a substitute for insulin in insulin-dependent diabetes
Diabetic ketoacidosis – requires immediate insulin therapy, not GLP-1 receptor agonists
Cautions and special considerations:
Severe gastrointestinal disease, particularly severe gastroparesis, as tirzepatide may worsen symptoms due to delayed gastric emptying
History of pancreatitis – requires careful risk-benefit assessment and close monitoring
Dehydration risk – particularly important in patients with renal impairment, though tirzepatide generally requires no dose adjustment based on renal function
Pregnancy and breastfeeding – not recommended due to insufficient safety data; alternative treatments should be used
History of eating disorders – appetite suppression may worsen these conditions
Elderly patients (particularly those >75 years) – may be more susceptible to dehydration and adverse effects
Important drug interactions:
Oral hormonal contraceptives – tirzepatide may reduce exposure to oral contraceptives, particularly during initiation and dose increases. Women should consider using non-oral contraceptives or adding barrier methods for 4 weeks after starting tirzepatide or after each dose increase
Insulin or sulphonylureas – concomitant use increases hypoglycaemia risk; dose reductions of these medications may be needed
Medications requiring rapid gastrointestinal absorption – tirzepatide delays gastric emptying and may affect absorption of some oral medications
All patients should undergo comprehensive medical history review, including medication reconciliation, before commencing tirzepatide. Shared decision-making, incorporating patient preferences and individual risk factors, should guide treatment selection in accordance with NICE principles of person-centred care.
Patients should report any suspected side effects to their healthcare professional and via the MHRA Yellow Card Scheme at yellowcard.mhra.gov.uk.
No, oral tirzepatide is not currently authorised by the MHRA in the UK. Tirzepatide (Mounjaro) is only available as an injectable formulation for type 2 diabetes management.
The most common side effects of injectable tirzepatide include nausea, diarrhoea, vomiting, decreased appetite, abdominal discomfort, constipation, and dyspepsia. These gastrointestinal effects are typically mild to moderate and tend to diminish over the first 4–8 weeks of treatment.
Seek immediate medical attention (call 999 or attend A&E) if you experience severe persistent abdominal pain (possible pancreatitis), signs of severe hypoglycaemia with loss of consciousness, allergic reactions with difficulty breathing or facial swelling, or persistent vomiting preventing fluid intake for 24 hours.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.