Ozempic and throwing up is a common concern for patients prescribed this type 2 diabetes medication. Ozempic (semaglutide), a GLP-1 receptor agonist, frequently causes gastrointestinal side effects including nausea and vomiting, affecting approximately 5–9% of users. These symptoms typically occur because the medication slows gastric emptying and activates receptors in the brain's nausea centres. Whilst often temporary and manageable through dietary adjustments and dose titration, persistent vomiting requires medical assessment. Understanding why these side effects occur, how to manage them effectively, and when to seek professional advice helps patients make informed decisions about their diabetes treatment whilst maintaining safety and quality of life.
Quick Answer: Ozempic causes vomiting in approximately 5–9% of patients by slowing gastric emptying and activating brain receptors involved in nausea.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Its mechanism of action directly explains why gastrointestinal side effects, including nausea and vomiting, are common.
Semaglutide works by mimicking the naturally occurring hormone GLP-1, which is released from the intestine after eating. This medication slows gastric emptying—the rate at which food leaves the stomach and enters the small intestine. Whilst this delayed emptying helps control blood glucose levels and promotes satiety (feeling full), it also means food remains in the stomach for longer periods. This prolonged gastric retention can trigger feelings of fullness, nausea, and in some cases, vomiting. Importantly, this gastric-emptying effect is most pronounced early in treatment and typically attenuates with continued use (tachyphylaxis), which partly explains why symptoms often improve over time.
Additionally, GLP-1 receptors are present in areas of the brain involved in nausea and appetite regulation, particularly the area postrema in the brainstem. Activation of these receptors may contribute to the sensation of nausea. The effect is dose-dependent, meaning higher doses of Ozempic are more likely to cause these symptoms.
Individual variation in tolerance is significant. Some patients experience minimal gastrointestinal upset, whilst others find nausea and vomiting substantially affect their quality of life. Factors such as the speed of dose escalation, dietary habits, and individual sensitivity to GLP-1 receptor activation all influence symptom severity. According to the MHRA-approved Summary of Product Characteristics (SmPC), semaglutide is not recommended in patients with severe gastrointestinal disease, including severe gastroparesis.
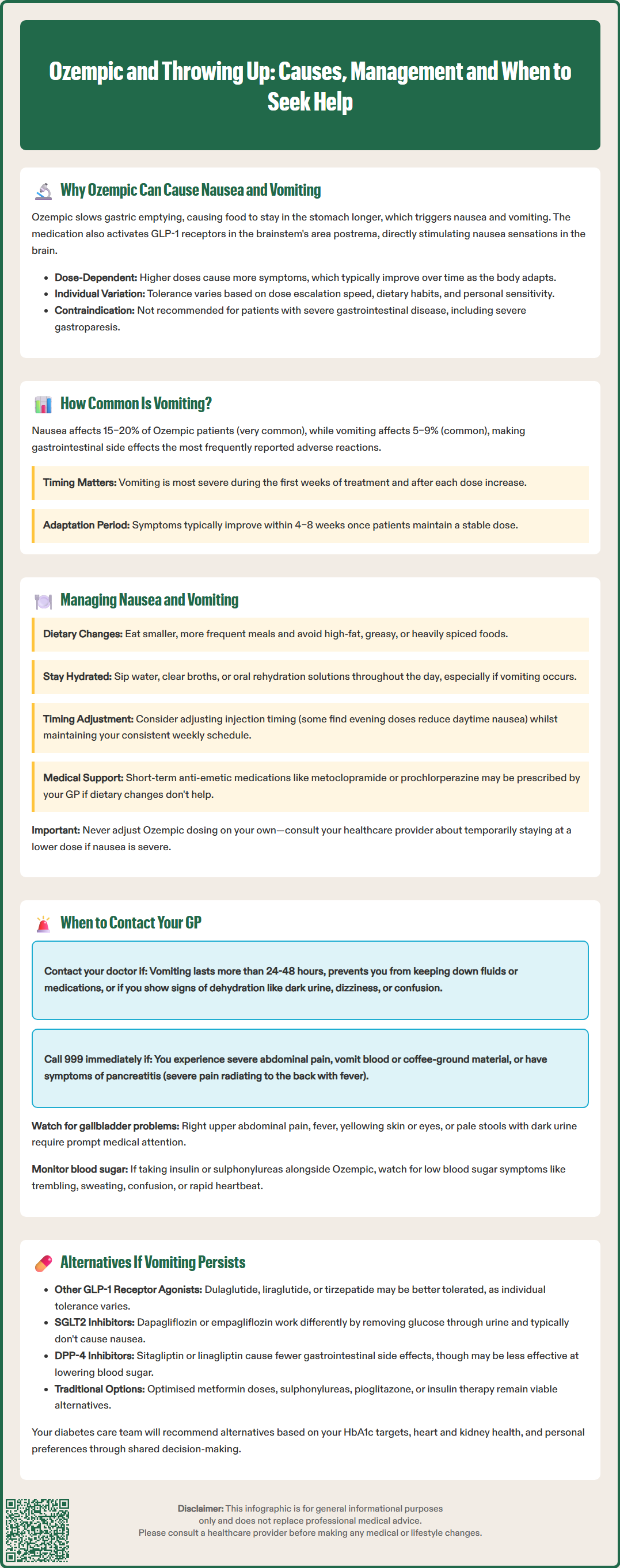
Gastrointestinal side effects are the most frequently reported adverse reactions associated with Ozempic. According to the UK SmPC, nausea is classified as 'very common' (affecting ≥1/10 patients), occurring in approximately 15–20% of patients, whilst vomiting is 'common' (affecting ≥1/100 to <1/10), affecting roughly 5–9% of those taking the medication.
The incidence of vomiting varies considerably depending on the dose and duration of treatment. Symptoms are typically most pronounced during the initial weeks of therapy and following dose increases. The standard titration schedule begins at 0.25 mg once weekly for four weeks, increasing to 0.5 mg, and potentially to 1 mg or 2 mg for optimal glycaemic control. Each dose escalation may trigger a recurrence of nausea or vomiting, even if previous doses were well tolerated.
Clinical trials demonstrate that gastrointestinal symptoms usually diminish over time as the body adapts to the medication. Most patients who experience nausea report improvement within 4–8 weeks of maintaining a stable dose. However, a small proportion of patients discontinue Ozempic specifically due to gastrointestinal adverse events that do not resolve with conservative management.
Comparative data show that vomiting rates with Ozempic are similar to other GLP-1 receptor agonists, though individual responses vary. Patients with gastroparesis or other gastrointestinal disorders may be at higher risk of experiencing troublesome vomiting. It is important to note that whilst these side effects are common, they do not indicate an allergic reaction or serious harm in most cases, though persistent vomiting requires medical assessment to prevent dehydration and ensure appropriate management.
Effective management of nausea and vomiting can significantly improve tolerability and treatment adherence. Dietary modifications represent the first-line approach and are often highly effective. Patients should consider eating smaller, more frequent meals rather than three large meals daily. Avoiding high-fat, greasy, or heavily spiced foods can reduce gastric irritation, as these foods are slower to digest and may exacerbate delayed gastric emptying.
Staying well hydrated is essential, particularly if vomiting occurs. Sipping water, clear broths, or oral rehydration solutions throughout the day helps prevent dehydration. Ginger tea or ginger supplements may provide natural anti-nausea benefits for some individuals, though evidence for their efficacy is limited.
Timing of injections may influence symptom severity for some patients, though this is based on anecdotal experience rather than robust evidence. Some patients report that administering Ozempic in the evening helps reduce daytime nausea, but maintaining consistency in your weekly dosing schedule is most important. The injection can be given at any time of day, with or without meals, providing flexibility to find what works best for you.
If conservative measures prove insufficient, anti-emetic medications may be considered for short-term use. Your GP might prescribe medications such as metoclopramide (limited to maximum 5 days' use due to neurological side effect risks), domperidone (at lowest effective dose for shortest duration due to cardiac risks), or prochlorperazine. These should only be used under medical supervision and for brief periods, as they carry their own side effect profiles and safety restrictions.
Dose adjustment represents another important strategy. If vomiting is severe or persistent, your healthcare provider may recommend remaining at a lower dose for a longer period before attempting further increases, or reducing the dose temporarily. NICE guidance emphasises individualised treatment approaches that balance glycaemic control with tolerability. Never adjust your Ozempic dose without consulting your prescriber, as this may affect diabetes management.
If you are vomiting and unable to keep fluids down, follow your local NHS sick-day rules for diabetes. This typically includes monitoring blood glucose more frequently, maintaining hydration if possible, and contacting your diabetes team for advice. Persistent vomiting can lead to dehydration and potentially acute kidney injury, particularly in older adults or those with existing kidney problems.
Whilst mild nausea is expected with Ozempic, certain symptoms warrant prompt medical attention. You should contact your GP or healthcare provider if you experience:
Persistent vomiting lasting more than 24–48 hours, or vomiting that prevents you from keeping down fluids or medications
Signs of dehydration, including dark urine, dizziness when standing, dry mouth, reduced urination, or confusion
Severe abdominal pain, particularly if constant or accompanied by fever, as this may indicate pancreatitis (a rare but serious side effect)
Vomiting blood or material that looks like coffee grounds
Inability to tolerate any food or fluids for more than 24 hours
Symptoms of hypoglycaemia (low blood sugar) if you also take insulin or sulphonylureas, including trembling, sweating, confusion, or rapid heartbeat
Seek emergency care (call 999 or go to A&E) if you have severe abdominal pain, are vomiting blood, have signs of severe dehydration, or are experiencing symptoms of pancreatitis. For urgent but non-emergency concerns, contact NHS 111 for advice.
Acute pancreatitis is a rare but recognised adverse effect of GLP-1 receptor agonists. Symptoms include severe, persistent abdominal pain (often radiating to the back), nausea, vomiting, and fever. If pancreatitis is suspected, stop taking Ozempic immediately and seek urgent medical attention.
Gallbladder problems (cholelithiasis, cholecystitis) have also been associated with GLP-1 receptor agonists. Contact your doctor promptly if you develop right upper abdominal pain, fever, jaundice (yellowing of skin/eyes), or pale stools with dark urine.
You should also contact your GP if nausea or vomiting significantly impairs your quality of life or prevents you from maintaining adequate nutrition, even if symptoms are not severe. Your healthcare provider can assess whether dose adjustment, additional supportive treatment, or consideration of alternative therapies is appropriate.
If you believe you've experienced a side effect from Ozempic, you can report it directly to the MHRA through the Yellow Card Scheme (yellowcard.mhra.gov.uk), which helps monitor medication safety.
If vomiting remains problematic despite optimal management strategies, several alternative treatment options are available for type 2 diabetes management. The choice depends on individual circumstances, including glycaemic control requirements, other medical conditions, and patient preferences.
Other GLP-1 receptor agonists may be considered, as individual tolerance varies between agents. Dulaglutide (Trulicity), liraglutide (Victoza), and exenatide (Byetta, Bydureon) work through similar mechanisms but have different pharmacokinetic profiles. Tirzepatide (Mounjaro), a newer dual GIP/GLP-1 receptor agonist, is also available in the UK, though it may also cause gastrointestinal side effects. Oral semaglutide (Rybelsus) provides a tablet option but similarly carries a risk of nausea and vomiting. Some patients who cannot tolerate one GLP-1 agonist find an alternative more acceptable, though cross-intolerance is possible.
SGLT2 inhibitors (sodium-glucose co-transporter-2 inhibitors) such as dapagliflozin, empagliflozin, or canagliflozin represent a different drug class with cardiovascular and renal benefits. These medications work by increasing glucose excretion through urine and do not typically cause nausea or vomiting. NICE guideline NG28 recommends SGLT2 inhibitors as an option for adults with type 2 diabetes, particularly those with established cardiovascular disease or chronic kidney disease.
DPP-4 inhibitors (dipeptidyl peptidase-4 inhibitors) such as sitagliptin, linagliptin, or saxagliptin offer another alternative. These oral medications enhance the body's own GLP-1 activity but generally cause fewer gastrointestinal side effects than GLP-1 receptor agonists, though their glucose-lowering efficacy is typically more modest.
For some patients, returning to or optimising traditional oral agents such as metformin (if not already at maximum tolerated dose), sulphonylureas, or pioglitazone may be appropriate. In cases requiring more intensive glucose control, insulin therapy remains an effective option, though it requires more frequent monitoring and carries a risk of hypoglycaemia and weight gain.
Your diabetes care team will consider your HbA1c targets, cardiovascular risk profile, renal function, and personal preferences when recommending alternatives. NICE guidance emphasises shared decision-making, ensuring treatment choices align with individual clinical needs and quality of life considerations. Discontinuing Ozempic due to intolerable side effects does not mean abandoning effective diabetes management—numerous evidence-based alternatives can achieve excellent glycaemic control whilst maintaining tolerability.
Vomiting from Ozempic is usually most pronounced during the first 4–8 weeks of treatment or following dose increases. Most patients experience improvement as their body adapts to the medication, though a small proportion may require dose adjustment or alternative treatment if symptoms persist.
Yes, your GP may prescribe short-term anti-emetic medications such as metoclopramide, domperidone, or prochlorperazine if dietary measures prove insufficient. These should only be used under medical supervision due to potential side effects and safety restrictions on duration of use.
Do not stop Ozempic without consulting your healthcare provider. Contact your GP if vomiting persists beyond 24–48 hours or prevents fluid intake, as dose adjustment or supportive treatment may help. Stop immediately and seek urgent care only if you experience severe abdominal pain suggesting pancreatitis.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.