
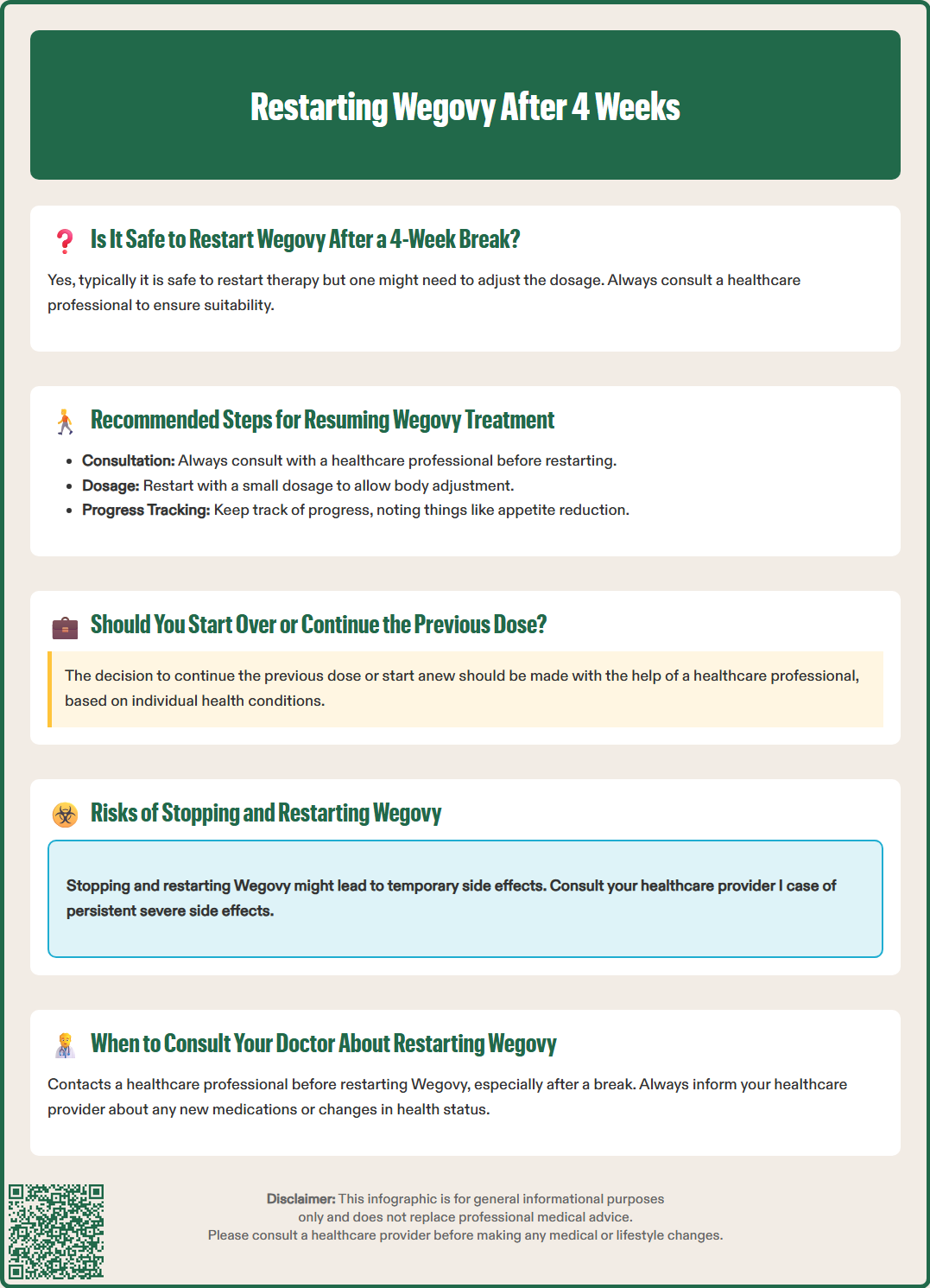
Restarting Wegovy after 4 weeks requires careful clinical consideration and dose adjustment. Wegovy (semaglutide 2.4 mg) is a GLP-1 receptor agonist licensed in the UK for weight management in adults with obesity or overweight with comorbidities. When treatment is interrupted for four weeks or longer, the body's adaptation to the medication diminishes, and gastrointestinal tolerance is lost. According to UK prescribing guidance, restarting typically requires re-titration from the initial 0.25 mg dose to minimise side effects and ensure safe, effective treatment resumption. Understanding the proper restart protocol is essential for both patients and healthcare professionals.
Quick Answer: When restarting Wegovy after a 4-week interruption, treatment should generally be reinitiated at the lowest dose (0.25 mg once weekly) and gradually re-titrated over 16-20 weeks to minimise gastrointestinal side effects.
Wegovy (semaglutide 2.4 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27-<30 kg/m²) with weight-related comorbidities. The medication works by mimicking the natural hormone GLP-1, which regulates appetite, slows gastric emptying, and enhances feelings of satiety. Treatment interruptions can occur for various reasons, including supply issues, side effects, illness, or personal circumstances.
When Wegovy treatment is stopped for four weeks or longer, the body's adaptation to the medication diminishes. The drug has a half-life of approximately one week, and semaglutide may remain in circulation for around seven weeks after the last dose. After four weeks without treatment, exposure to semaglutide is markedly reduced, requiring careful consideration when restarting.
Understanding the implications of treatment gaps is crucial for both patients and healthcare professionals. A four-week interruption represents a significant break that requires careful consideration when restarting. The gastrointestinal system, which had adapted to the medication's effects on gastric motility, returns to its pre-treatment state. Similarly, the appetite-suppressing effects wear off, and patients may experience return of previous hunger patterns.
Common reasons for treatment interruptions include:
Medication supply shortages or availability issues
Intolerable gastrointestinal side effects requiring a break
Acute illness or surgical procedures
Pregnancy or planning pregnancy (note: Wegovy must be discontinued at least 2 months before planned conception)
Funding or prescription access changes
Travel or lifestyle disruptions
Recognising why the interruption occurred helps inform the restart strategy and prevents future discontinuations.
According to the Wegovy Summary of Product Characteristics (SmPC), if Wegovy has been discontinued for more than two consecutive doses during the dose escalation phase, or more than two consecutive doses at any maintenance dose, treatment should generally be reinitiated at a lower dose (often 0.25 mg once weekly) and re-titrated according to clinical judgement. This recommendation is based on pharmacokinetic data and clinical safety considerations.
After a four-week gap, clinicians may advise restarting at the initial 0.25 mg dose depending on the patient's tolerance and prior experience. This approach minimises the risk of gastrointestinal adverse effects, which are significantly more common when higher doses are resumed without proper titration. The gastrointestinal tract loses its tolerance to semaglutide during the interruption period, making patients more susceptible to side effects.
NICE Technology Appraisal (TA875) on semaglutide for weight management specifies that within the NHS, Wegovy should be prescribed by specialist weight management services and used for a maximum of 2 years. Eligible adults typically have:
A BMI ≥35 kg/m² and at least one weight-related comorbidity, or
A BMI between 30–34.9 kg/m² when meeting specialist referral criteria (lower thresholds may apply for some ethnic groups)
When restarting after an extended break, healthcare providers should:
Reassess the patient's current weight and comorbidities
Review the reasons for treatment interruption
Ensure contraindications have not developed during the break
Discuss realistic expectations for weight loss trajectory
Reinforce dietary and lifestyle modification strategies
Patients should be counselled that restarting at the lowest dose is a safety measure, not a setback. The dose escalation schedule will follow the same four-weekly increments used initially: 0.25 mg, 0.5 mg, 1 mg, 1.7 mg, and finally 2.4 mg maintenance dose. This process typically takes 16-20 weeks to reach the therapeutic dose again.
Documentation of the treatment interruption and restart plan in medical records ensures continuity of care and appropriate monitoring throughout the re-titration period.
The standard dose escalation schedule for restarting Wegovy after a four-week interruption follows the same protocol as initial treatment, as specified in the SmPC. Patients generally begin with 0.25 mg once weekly for four weeks, allowing the body to readjust to the medication's effects on gastric emptying and appetite regulation. This gradual approach is essential for tolerability and treatment adherence.
The complete re-titration schedule proceeds as follows:
Weeks 1-4: 0.25 mg once weekly
Weeks 5-8: 0.5 mg once weekly
Weeks 9-12: 1 mg once weekly
Weeks 13-16: 1.7 mg once weekly
Week 17 onwards: 2.4 mg once weekly (maintenance dose)
Each dose increase should occur only if the current dose is well tolerated. If patients experience significant gastrointestinal side effects at any stage, the dose escalation may be delayed by an additional four weeks at the current dose level. This flexibility allows individualised treatment whilst maintaining safety.
Injection technique remains important when restarting. Wegovy is administered subcutaneously in the abdomen, thigh, or upper arm. Patients should rotate injection sites to reduce local reactions and ensure consistent absorption. The injection should be given on the same day each week, though the day can be changed if necessary, provided there is a minimum interval of 3 days between doses.
Some patients may question whether a faster titration is possible, particularly if they previously tolerated higher doses well. However, the SmPC does not support accelerated dose escalation after treatment interruptions. The risk of severe nausea, vomiting, and treatment discontinuation increases substantially when proper titration is not followed.
Patients who were previously on lower maintenance doses (such as 1.7 mg) due to tolerability issues should discuss their target dose with their prescriber when restarting. The goal remains achieving the highest tolerated dose for optimal weight management outcomes.
Gastrointestinal side effects are the most common adverse reactions when restarting Wegovy, occurring in a similar pattern to initial treatment. According to the SmPC and STEP clinical trials, nausea affects approximately 44% of patients, whilst vomiting, diarrhoea, constipation, and abdominal pain are also frequently reported. These effects typically peak during the first few days after each dose increase and generally diminish over 1-2 weeks as the body adapts.
To minimise gastrointestinal symptoms when restarting treatment, patients should implement several practical strategies:
Eat smaller, more frequent meals throughout the day
Avoid high-fat, greasy, or heavily spiced foods
Stay well hydrated, sipping water regularly
Eat slowly and stop when feeling comfortably satisfied
Avoid lying down immediately after eating
Consider anti-emetics if prescribed by a healthcare professional
If nausea becomes problematic, patients may discuss anti-emetic medications with their GP. However, lifestyle and dietary modifications should be the first-line approach. Persistent vomiting that prevents adequate fluid intake requires medical attention to prevent dehydration.
Constipation management is equally important, as reduced gastric motility can lead to uncomfortable bowel changes. Increasing dietary fibre gradually, maintaining hydration, and regular physical activity help maintain bowel regularity. If constipation persists, bulk-forming laxatives such as ispaghula husk may be appropriate.
Some patients experience injection site reactions, including redness, itching, or mild swelling. These are usually mild and resolve spontaneously. Proper injection technique and site rotation minimise these reactions.
Rarely, more serious adverse effects may occur, including:
Acute pancreatitis (severe abdominal pain radiating to the back)
Gallbladder problems (right upper quadrant pain, particularly after meals)
Hypoglycaemia (in patients taking concomitant diabetes medications)
Acute kidney injury (usually secondary to severe dehydration)
Worsening of diabetic retinopathy (in people with diabetes)
Thyroid symptoms (persistent hoarseness, neck mass, difficulty swallowing)
Patients should be educated about these warning signs and instructed to seek immediate medical attention if they occur.
Patients restarting Wegovy after a four-week interruption should maintain regular contact with their healthcare provider throughout the re-titration process. An initial consultation before restarting is essential to review the treatment plan, assess any changes in health status, and ensure the medication remains appropriate.
Immediate medical attention is required if any of the following occur:
Severe, persistent abdominal pain, particularly if radiating to the back (possible pancreatitis)
Persistent vomiting preventing fluid intake for more than 24 hours
Signs of dehydration: dark urine, dizziness, reduced urination, extreme thirst
Symptoms of gallbladder disease: right upper abdominal pain, fever, jaundice
Allergic reactions: rash, difficulty breathing, facial swelling
For people with diabetes: worsening vision or diabetic retinopathy symptoms
Symptoms of hypoglycaemia: shakiness, confusion, sweating, rapid heartbeat
Pregnancy or suspected pregnancy (Wegovy is contraindicated in pregnancy)
Patients should contact their GP or prescriber within a few days if they experience:
Intolerable nausea or vomiting that persists beyond the first week of a new dose
Severe constipation unresponsive to dietary changes and over-the-counter remedies
Persistent diarrhoea lasting more than a few days
Unusual or concerning weight loss patterns
Mood changes, depression, or suicidal thoughts
Thyroid symptoms: persistent hoarseness, lump in the neck, difficulty swallowing
Concerns about medication interactions
Routine follow-up appointments should be scheduled at regular intervals during re-titration, typically:
Before restarting treatment (baseline assessment)
After 8-12 weeks (mid-titration review)
After reaching maintenance dose
Every 3-6 months thereafter for ongoing monitoring
These appointments allow monitoring of weight loss progress, assessment of side effects, review of dietary and lifestyle modifications, and evaluation of cardiovascular risk factors. Blood pressure, heart rate, and relevant blood tests (such as HbA1c in diabetic patients) should be monitored according to individual clinical needs.
Patients should never adjust their dose independently or skip the titration schedule without medical guidance.
Preventing future treatment interruptions is crucial for optimal weight management outcomes. Studies from the STEP clinical trial programme demonstrate that continuous treatment with semaglutide produces superior weight loss compared to interrupted therapy. When treatment is stopped, weight regain commonly occurs, with patients typically regaining approximately two-thirds of lost weight within one year of discontinuation.
To maintain treatment continuity, patients should:
Plan ahead for repeat prescriptions, requesting at least one week before running out
Communicate with their pharmacy about potential supply issues
Discuss funding or access concerns with their healthcare provider promptly
Set reminders for weekly injections to establish a consistent routine
Store medication properly: refrigerate at 2-8°C before first use, do not freeze. Before first use, a pen may be kept unrefrigerated for up to 28 days at temperatures ≤30°C. After first use, it can be stored for up to 6 weeks at ≤30°C or refrigerated, with the cap on to protect from light.
Lifestyle modifications remain fundamental to long-term success, even when medication is temporarily interrupted. Wegovy is licensed as an adjunct to a reduced-calorie diet and increased physical activity, not as monotherapy. Patients should continue implementing healthy eating patterns and regular exercise during any treatment gaps to minimise weight regain.
The NHS weight management framework emphasises a holistic approach combining pharmacotherapy with behavioural interventions. Patients may benefit from:
Referral to specialist weight management services
Dietitian consultations for personalised nutrition advice
Psychological support for emotional eating or body image concerns
Structured physical activity programmes
Peer support groups or digital health platforms
Long-term treatment planning should address realistic expectations. Within the NHS, NICE guidance (TA875) specifies that Wegovy should be prescribed by specialist weight management services for a maximum of 2 years. When restarting after interruption, patients should discuss with their healthcare provider how this affects their overall treatment duration.
Patients should understand that weight maintenance strategies will be important, as evidence from clinical trials suggests that discontinuation leads to weight regain in most individuals. Discussions about treatment duration, stopping criteria, and weight maintenance strategies should occur regularly between patients and healthcare providers.
Establishing strong communication channels, realistic goals, and comprehensive support systems maximises the likelihood of successful long-term weight management, whether treatment is continuous or requires restarting after interruption.
Yes, according to UK prescribing guidance, if Wegovy has been discontinued for more than two consecutive doses, treatment should generally be reinitiated at 0.25 mg once weekly and gradually re-titrated to minimise gastrointestinal side effects and ensure safety.
The complete re-titration process typically takes 16-20 weeks to reach the 2.4 mg maintenance dose, following monthly dose increases through 0.25 mg, 0.5 mg, 1 mg, and 1.7 mg stages.
The most common side effects when restarting include nausea (affecting approximately 44% of patients), vomiting, diarrhoea, constipation, and abdominal discomfort. These typically peak after dose increases and diminish over 1-2 weeks as the body readapts to the medication.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.