
Skin reactions to Mounjaro (tirzepatide) are among the most commonly reported side effects of this once-weekly injectable treatment for type 2 diabetes. These localised responses—including redness, swelling, itching, and bruising at the injection site—are typically mild and self-limiting, resolving within days. Understanding what to expect, why these reactions occur, and how to manage or prevent them empowers patients to use Mounjaro safely and confidently. This article provides evidence-based guidance aligned with UK clinical practice, helping you distinguish normal injection site responses from those requiring medical attention.
Quick Answer: Skin reactions to Mounjaro are common, typically mild injection site responses including redness, swelling, itching, and bruising that usually resolve within 24–72 hours without specific treatment.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMounjaro (tirzepatide) is a once-weekly injectable medication used for the treatment of type 2 diabetes mellitus in the UK. As with many subcutaneous injections, skin reactions at the injection site are among the most frequently reported adverse effects. Understanding these reactions helps patients distinguish between expected, self-limiting responses and those requiring medical attention.
The most common skin reactions include:
Injection site erythema (redness) – localised redness around the injection area, typically resolving within hours to days
Injection site pruritus (itching) – mild to moderate itching that may accompany redness
Injection site swelling – localised oedema or a small raised area at the injection site
Injection site pain or tenderness – discomfort ranging from mild sensitivity to moderate pain
Bruising (ecchymosis) – small bruises caused by minor capillary damage during injection
According to the Mounjaro Summary of Product Characteristics (SmPC), injection site reactions are classified as 'common' adverse effects. These reactions are generally mild to moderate in severity and tend to diminish with continued use as the body adapts to the medication. Most resolve spontaneously within 24–72 hours without specific intervention.
Less common but notable skin reactions may include nodules or small lumps under the skin, particularly if injection sites are not rotated adequately. Rarely, patients may develop allergic-type reactions characterised by more extensive redness, warmth, or hives extending beyond the immediate injection area.
Any signs of infection—such as increasing pain, warmth, pus, or fever—warrant prompt medical assessment, as these are not typical reactions to tirzepatide itself. If you experience symptoms of a severe allergic reaction (difficulty breathing, facial swelling, dizziness), call 999 or attend A&E immediately.
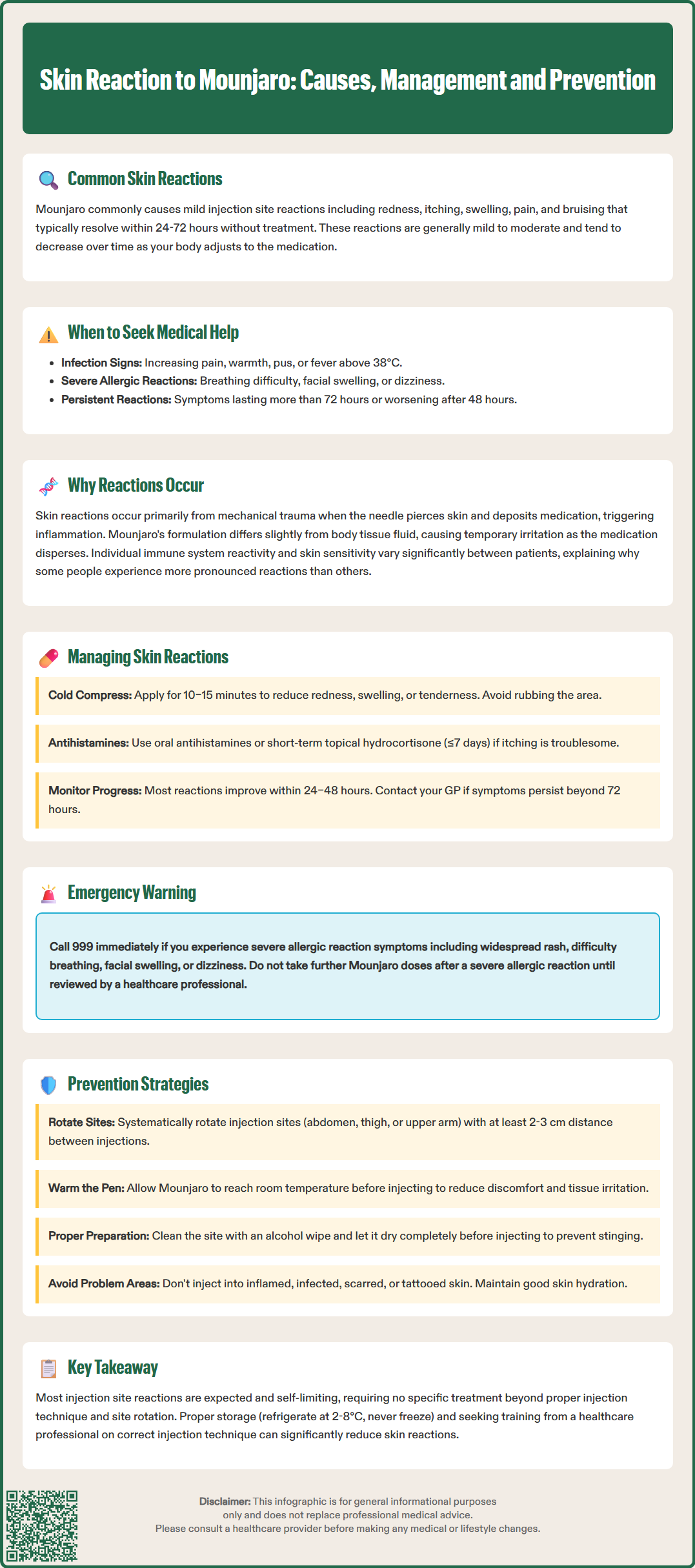
Understanding the underlying mechanisms behind skin reactions to Mounjaro helps contextualise why these effects occur and reassures patients that most reactions represent normal physiological responses rather than serious complications.
Mechanical trauma from injection is the primary cause of localised skin reactions. The act of piercing the skin and depositing medication into subcutaneous tissue inevitably causes minor tissue disruption. This mechanical injury triggers a localised inflammatory response, characterised by the release of histamine and other inflammatory mediators. These substances increase local blood flow (causing redness), promote fluid accumulation (causing swelling), and stimulate nerve endings (causing pain or itching). The needle itself may also damage small blood vessels, resulting in bruising.
The medication's formulation also contributes to local reactions. Mounjaro contains tirzepatide as the active pharmaceutical ingredient, along with various excipients. The solution, whilst designed to be as physiologically compatible as possible, may still differ slightly from surrounding tissue fluid. This difference can cause transient irritation as the medication disperses through subcutaneous tissue. The volume injected creates temporary distension of tissue, which may be perceived as discomfort or tightness.
Individual immune responses vary considerably between patients. Some individuals have more reactive immune systems or sensitive skin, predisposing them to more pronounced local reactions. It's important to note that systemic hypersensitivity reactions (including anaphylaxis and angioedema) are recognised in the SmPC as potential, though rare, adverse effects. If these occur, urgent medical attention is required and further doses should be withheld pending medical review.
Factors such as injection technique and site selection influence the degree of tissue trauma and subsequent reaction severity.
Most skin reactions to Mounjaro are self-limiting and require only conservative management. However, knowing appropriate strategies can improve comfort and help patients identify when professional medical advice is needed.
For mild injection site reactions (redness, swelling, tenderness):
Apply a cold compress – use a clean cloth with ice or a cold pack for 10–15 minutes to reduce inflammation and numb discomfort. Avoid applying ice directly to skin.
Avoid rubbing or scratching – this can worsen inflammation and increase the risk of introducing infection.
Monitor the reaction – most reactions should begin improving within 24–48 hours. Take photographs if helpful for tracking progression.
Over-the-counter relief – oral antihistamines (such as cetirizine 10 mg once daily) may help with itching, though this is rarely necessary. Topical hydrocortisone 1% cream may be applied sparingly if itching is troublesome, but only for short-term use (≤7 days), avoiding the face and broken skin. Consult a pharmacist before using.
For bruising:
Allow bruises to resolve naturally over 7–14 days
Do not stop prescribed antiplatelet or anticoagulant medicines, though be aware these may increase bruising
Arnica gel may be applied topically, though evidence for efficacy is limited
When to contact your GP or diabetes specialist nurse:
Reactions lasting more than 72 hours or worsening after 48 hours
Signs of infection: increasing pain, warmth, red streaking, pus, or fever >38°C
Large areas of swelling (>5 cm diameter) or severe pain
Persistent nodules or lumps that do not resolve
When to seek urgent medical attention:
Symptoms of severe allergic reaction: widespread rash, difficulty breathing, facial swelling, or dizziness – call 999 or attend A&E immediately
For other concerning symptoms outside normal GP hours, contact NHS 111
If severe allergic symptoms occur, do not take further doses until reviewed by a healthcare professional. For non-emergency concerns, contact your prescriber before making any changes to your treatment regimen.
Whilst some degree of injection site reaction may be unavoidable, evidence-based injection techniques and practical strategies can significantly reduce both frequency and severity of skin reactions.
Proper injection technique is fundamental:
Rotate injection sites systematically – use different areas of the abdomen, thigh, or upper arm for each injection. Upper arm injections should only be given by someone else. Maintain at least 2–3 cm distance from the previous injection site. Consider keeping a simple diary or using a body map to track rotation.
Allow medication to reach room temperature – remove the Mounjaro pen from the refrigerator and allow it to warm naturally before injection, following the specific timing in the Patient Information Leaflet (PIL). Cold medication causes more discomfort and tissue irritation.
Clean the injection site – use an alcohol wipe and allow the skin to dry completely before injecting. Injecting through wet alcohol can cause stinging.
Follow the pen's Instructions for Use – place the pen flat against clean skin, press and hold until the indicator shows completion, then wait the specified time before removing.
Do not attempt to reuse the pen – Mounjaro comes in a single-use pre-filled pen that automatically disables after use.
Additional preventive measures:
Avoid injecting into areas with existing skin conditions – do not inject into inflamed, infected, scarred, or tattooed skin
Maintain good skin hydration – well-hydrated skin may be more resilient to injection trauma
Review medications that increase bruising risk – discuss with your GP if you take anticoagulants or antiplatelet agents
Ensure proper storage – store Mounjaro in the refrigerator (2–8°C), do not freeze, and protect from light; follow the PIL for permitted time at room temperature
Patients should receive initial training from a healthcare professional on proper injection technique. Many diabetes specialist nurses offer refresher training if reactions become problematic.
Suspected adverse reactions to Mounjaro should be reported via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk), contributing to ongoing medication safety monitoring. Following the specific instructions in the Mounjaro PIL ensures safe and effective administration.
Most injection site reactions to Mounjaro resolve spontaneously within 24–72 hours without specific intervention. If reactions persist beyond 72 hours or worsen after 48 hours, contact your GP or diabetes specialist nurse for assessment.
Oral antihistamines such as cetirizine 10 mg once daily may help with itching, though this is rarely necessary. Topical hydrocortisone 1% cream may be applied sparingly for short-term use (≤7 days), avoiding the face and broken skin; consult a pharmacist before using.
Seek immediate emergency care by calling 999 or attending A&E if you experience symptoms of severe allergic reaction, including widespread rash, difficulty breathing, facial swelling, or dizziness. Do not take further doses until reviewed by a healthcare professional.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.