
Tirzepatide (Mounjaro) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for type 2 diabetes mellitus. Whilst clinical trials have demonstrated substantial improvements in glycaemic control and weight reduction, questions have emerged regarding thyroid safety—specifically, a theoretical risk of medullary thyroid carcinoma (MTC) identified in rodent studies. This article examines the evidence linking tirzepatide and thyroid cancer, reviews UK regulatory guidance from the MHRA and NICE, and outlines contraindications, monitoring protocols, and warning signs for patients and healthcare professionals.
Quick Answer: Tirzepatide carries a theoretical thyroid cancer risk based on rodent studies showing medullary thyroid carcinoma, but no confirmed link has been established in humans.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereTirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus under the brand name Mounjaro. It represents the first dual incretin receptor agonist approved by the Medicines and Healthcare products Regulatory Agency (MHRA).
The medication works through a dual mechanism of action. By activating both GIP and GLP-1 receptors, tirzepatide enhances glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriately elevated glucagon secretion, and slows gastric emptying. These combined effects lead to improved glycaemic control in patients with type 2 diabetes. Additionally, tirzepatide acts on appetite-regulating centres in the brain, promoting satiety and reducing food intake, which contributes to significant weight loss.
Tirzepatide is administered once weekly via subcutaneous injection, typically in the abdomen, thigh, or upper arm. The dosing follows a specific titration schedule: starting with 2.5 mg once weekly for 4 weeks as an initiation dose, then increasing to 5 mg. Further dose increases to 7.5 mg, 10 mg, 12.5 mg and 15 mg may be considered at intervals of at least 4 weeks, depending on individual response and tolerability. Clinical trials have demonstrated substantial reductions in HbA1c levels and body weight compared to other diabetes medications and GLP-1 receptor agonists.
It is important to note that tirzepatide is not indicated for the treatment of type 1 diabetes or diabetic ketoacidosis.
As with all incretin-based therapies, questions have been raised regarding potential thyroid safety concerns, particularly the theoretical risk of medullary thyroid carcinoma (MTC). This concern stems from preclinical animal studies and has led to specific warnings in the prescribing information, warranting careful consideration of patient selection and ongoing monitoring.
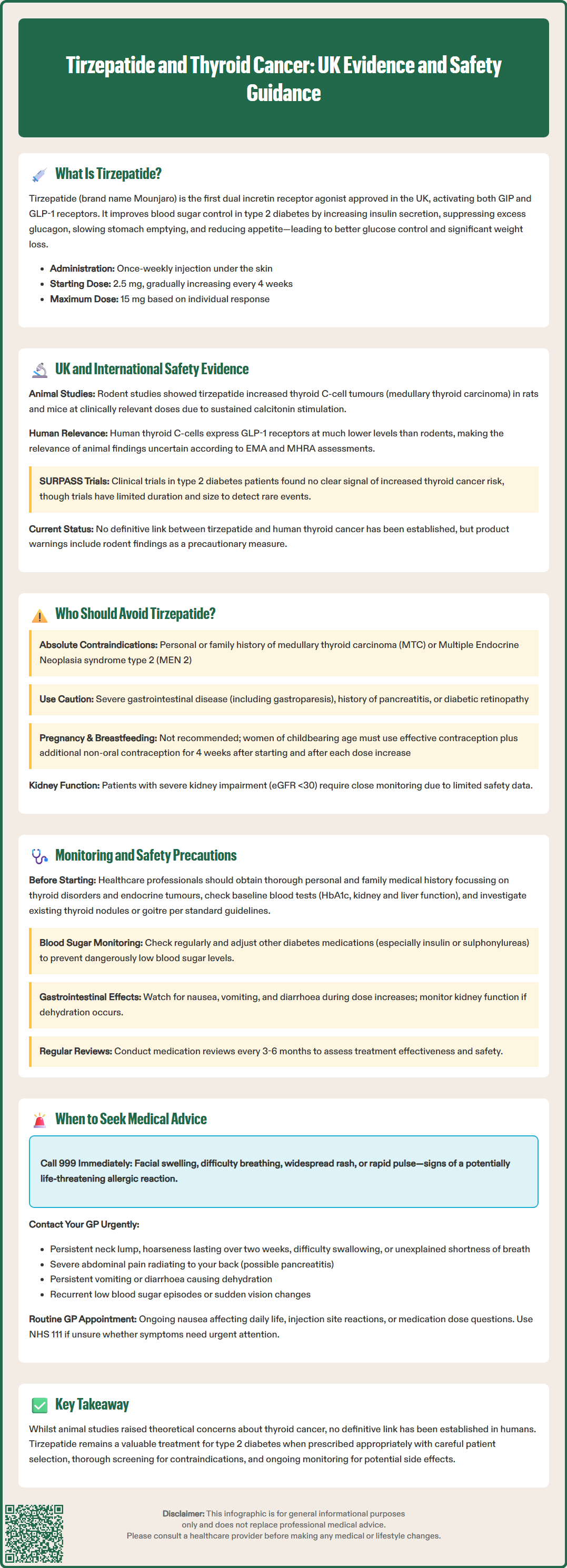
The relationship between tirzepatide and thyroid cancer has been evaluated through preclinical studies, clinical trials, and post-marketing surveillance. In rodent studies conducted during drug development, GLP-1 receptor agonists, including tirzepatide, were associated with an increased incidence of thyroid C-cell tumours (medullary thyroid carcinoma) in rats and mice. These findings occurred at clinically relevant exposures and are thought to result from sustained stimulation of calcitonin release from thyroid C-cells, which express GLP-1 receptors in rodents.
However, the relevance of these animal findings to humans remains uncertain. Thyroid C-cells in humans express GLP-1 receptors at substantially lower levels compared to rodents, and the physiological response to GLP-1 receptor stimulation differs significantly between species. The European Medicines Agency (EMA) and MHRA have acknowledged this species-specific difference in their risk assessments, noting in the Summary of Product Characteristics (SmPC) that the human relevance of rodent C-cell tumours is unknown.
In the comprehensive SURPASS clinical trial programme, which evaluated tirzepatide in patients with type 2 diabetes, no clear signal for increased thyroid cancer risk was identified during the study period. However, clinical trials have limited duration and participant numbers for detecting rare events. The evidence from observational studies of other GLP-1 receptor agonists has been mixed, with some studies showing no increased risk while others suggest a possible small increase in thyroid cancer diagnoses, though causality remains uncertain.
NICE guidance on tirzepatide for type 2 diabetes (TA924) acknowledges the theoretical thyroid cancer risk based on animal data but notes the limited evidence for increased risk in humans. The SmPC for tirzepatide includes specific warnings regarding the rodent findings in section 4.4 (Special warnings and precautions for use). While no definitive link between tirzepatide use and thyroid cancer in humans has been established, the precautionary principle guides current prescribing recommendations.
According to the UK Summary of Product Characteristics (SmPC), tirzepatide is contraindicated in patients with hypersensitivity to the active substance or to any of the excipients.
Special warnings and precautions apply to several patient groups, including:
Personal or family history of medullary thyroid carcinoma (MTC): The SmPC advises that tirzepatide should not be used in patients with a personal or family history of MTC due to the theoretical risk identified in animal studies, despite the lack of confirmed human evidence.
Multiple endocrine neoplasia syndrome type 2 (MEN 2): This inherited condition significantly increases MTC risk, making tirzepatide use inappropriate.
Additional patient groups requiring careful consideration or alternative treatment options include those with severe gastrointestinal disease, including gastroparesis, as tirzepatide delays gastric emptying. Patients with a history of pancreatitis should be counselled about potential risks, though causality remains unestablished.
Tirzepatide is not recommended during pregnancy or breastfeeding due to insufficient safety data. Women of childbearing potential should use effective contraception while taking tirzepatide. Importantly, tirzepatide may reduce the exposure of oral contraceptives taken concurrently due to delayed gastric emptying. Women using oral contraceptives should consider additional non-oral or barrier contraception for 4 weeks after initiation and for 4 weeks after each dose increase.
Patients with diabetic retinopathy require careful monitoring, particularly if rapid glycaemic improvement occurs, as this has been associated with temporary worsening of retinopathy with other diabetes medications. Those with severe renal impairment (eGFR <30 mL/min/1.73m²) should be monitored closely due to limited clinical trial data in this population.
Before initiating tirzepatide, healthcare professionals should conduct a thorough personal and family medical history, specifically enquiring about thyroid disorders and any family history of endocrine tumours. Patients with existing thyroid nodules or goitre should be investigated according to standard clinical pathways (as per NICE NG12 and British Thyroid Association guidance) based on clinical features, though routine thyroid screening is not currently recommended for all patients prior to starting treatment.
Appropriate monitoring and safety precautions are essential for patients prescribed tirzepatide to ensure early detection of potential adverse effects and optimise treatment outcomes. While routine thyroid monitoring is not mandated for all patients, healthcare professionals should maintain vigilance for thyroid-related symptoms throughout treatment.
Baseline assessment should include:
Comprehensive medical history focusing on personal and family history of thyroid disease and endocrine tumours
Current medications review to identify potential drug interactions
Baseline HbA1c, renal function, and liver function tests
Assessment of diabetic complications, particularly retinopathy
Discussion of gastrointestinal symptoms and previous tolerance of incretin-based therapies
Ongoing monitoring recommendations include:
Regular review of glycaemic control and adjustment of concomitant diabetes medications to prevent hypoglycaemia, particularly if used with insulin or sulphonylureas
Monitoring for gastrointestinal adverse effects (nausea, vomiting, diarrhoea), which are most common during dose escalation
Assessment of weight loss trajectory and nutritional status
Periodic renal function monitoring, especially in patients experiencing significant gastrointestinal side effects that may lead to dehydration
Vigilance for symptoms suggestive of pancreatitis (persistent severe abdominal pain) – if pancreatitis is suspected, tirzepatide should be discontinued immediately and not restarted if pancreatitis is confirmed
Awareness of gallbladder disease risk, which may be increased with GLP-1 receptor agonists and significant weight loss – patients should report right upper quadrant pain, fever, jaundice or other biliary symptoms
Thyroid-specific precautions include educating patients about symptoms that warrant medical attention, such as a neck lump, hoarseness, dysphagia, or dyspnoea. If a thyroid nodule is detected during treatment, standard investigation protocols should be followed, including thyroid function tests, ultrasound imaging, and consideration of fine-needle aspiration cytology if indicated by size or suspicious features.
Patients should be advised to report any new or worsening symptoms promptly. Healthcare professionals should document discussions about theoretical thyroid risks in medical records and ensure patients understand both the precautionary nature of warnings and the absence of confirmed human cases. Regular medication reviews, ideally every 3–6 months, allow for assessment of treatment efficacy, tolerability, and ongoing appropriateness of therapy in line with NICE guidance on diabetes management (NG28).
Patients taking tirzepatide should be educated about specific warning signs and symptoms that require prompt medical attention. While serious adverse events are uncommon, early recognition and appropriate action can prevent complications and ensure patient safety.
Thyroid-related symptoms requiring urgent GP consultation include:
A palpable lump or swelling in the neck that persists or enlarges
Persistent hoarseness or voice changes lasting more than two weeks
Difficulty swallowing (dysphagia) or a sensation of pressure in the neck
Unexplained shortness of breath or stridor
Persistent cough without other respiratory symptoms
These symptoms may indicate thyroid pathology requiring investigation, though they are not specific to medullary thyroid carcinoma and may have benign causes. GPs may use urgent suspected cancer referral pathways (NICE NG12) for persistent neck lumps, unexplained hoarseness, or other concerning features. Patients should be reassured that prompt reporting enables early detection of any thyroid abnormalities.
Other serious symptoms warranting immediate medical assessment include:
Severe abdominal pain: Persistent, severe pain radiating to the back may indicate pancreatitis and requires same-day assessment or emergency department attendance.
Signs of allergic reaction: Facial swelling, difficulty breathing, widespread rash, or rapid pulse suggest anaphylaxis requiring emergency treatment (call 999).
Severe gastrointestinal symptoms: Persistent vomiting or diarrhoea leading to dehydration, dizziness, or reduced urine output requires medical review.
Hypoglycaemia symptoms: If taking tirzepatide with insulin or sulphonylureas, recurrent episodes of sweating, tremor, confusion, or loss of consciousness require medication adjustment.
Visual changes: Sudden vision deterioration, floaters, or flashing lights may indicate diabetic retinopathy progression.
Gallbladder symptoms: Right upper quadrant pain, fever, jaundice, pale stools or dark urine may indicate gallbladder disease, which requires prompt assessment.
Routine concerns suitable for scheduled GP appointments include persistent nausea affecting quality of life, injection site reactions, or questions about dose adjustments. Patients should maintain regular contact with their diabetes care team and attend scheduled monitoring appointments. The NHS 111 service can provide guidance on urgency if patients are uncertain whether symptoms require immediate attention.
Patients are encouraged to report any suspected side effects to the MHRA Yellow Card scheme, which helps monitor the safety of medicines. Clear communication between patients and healthcare providers ensures optimal safety throughout tirzepatide treatment.
No confirmed link between tirzepatide and thyroid cancer in humans has been established. Rodent studies showed thyroid C-cell tumours, but human thyroid cells express GLP-1 receptors at much lower levels, and the relevance of animal findings remains uncertain.
Tirzepatide should not be used in patients with a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2 (MEN 2), as these conditions significantly increase thyroid cancer risk.
Report any persistent neck lump, hoarseness lasting more than two weeks, difficulty swallowing, unexplained shortness of breath, or persistent cough to your GP promptly for investigation.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.