
Mounjaro (tirzepatide) is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes and weight management. As with any medication affecting gastrointestinal function, patients may wonder about potential nutritional impacts, including vitamin B12 status. Whilst there is currently no established link between Mounjaro and vitamin B12 deficiency, understanding the role of this essential vitamin and recognising deficiency symptoms remains important for anyone taking medications that influence appetite, gastric function, or nutrient absorption. This article examines the relationship between vitamin B12 and Mounjaro, helping you make informed decisions about your health.
Quick Answer: There is currently no established clinical link between Mounjaro (tirzepatide) and vitamin B12 deficiency, and routine supplementation is not recommended unless individual risk factors are present.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMounjaro (tirzepatide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus and, more recently, for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. It must be used as an adjunct to a reduced-calorie diet and increased physical activity. Mounjaro belongs to a novel class of medications known as dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonists.
The mechanism of action involves mimicking two naturally occurring incretin hormones that regulate blood glucose and appetite. When administered as a once-weekly subcutaneous injection, tirzepatide enhances insulin secretion in response to elevated blood glucose levels, suppresses inappropriate glucagon release, slows gastric emptying, and promotes satiety through central appetite regulation. These combined effects lead to improved glycaemic control and significant weight reduction in clinical trials.
Mounjaro is typically initiated at 2.5 mg weekly for 4 weeks, then increased to 5 mg for at least 4 weeks. Further increases can be made in 2.5 mg increments (to 7.5, 10, 12.5, and 15 mg) at intervals of at least 4 weeks based on clinical response and tolerability. This gradual titration helps minimise gastrointestinal side effects, which are the most commonly reported adverse reactions.
Important safety considerations include an increased risk of hypoglycaemia when used with insulin or sulfonylureas (dose reductions of these medications may be needed), potential risk of pancreatitis (seek urgent medical attention for severe, persistent abdominal pain), gallbladder disease, and risk of dehydration or acute kidney injury with severe gastrointestinal events. Mounjaro is not recommended during pregnancy or breastfeeding and should be discontinued if pregnancy occurs or is planned.
Patients prescribed Mounjaro should receive comprehensive counselling about injection technique, storage requirements, and the importance of adhering to dietary and lifestyle modifications alongside pharmacotherapy. The medication is not suitable for individuals with type 1 diabetes or diabetic ketoacidosis, and careful consideration is required in those with a history of pancreatitis or severe gastrointestinal disease.
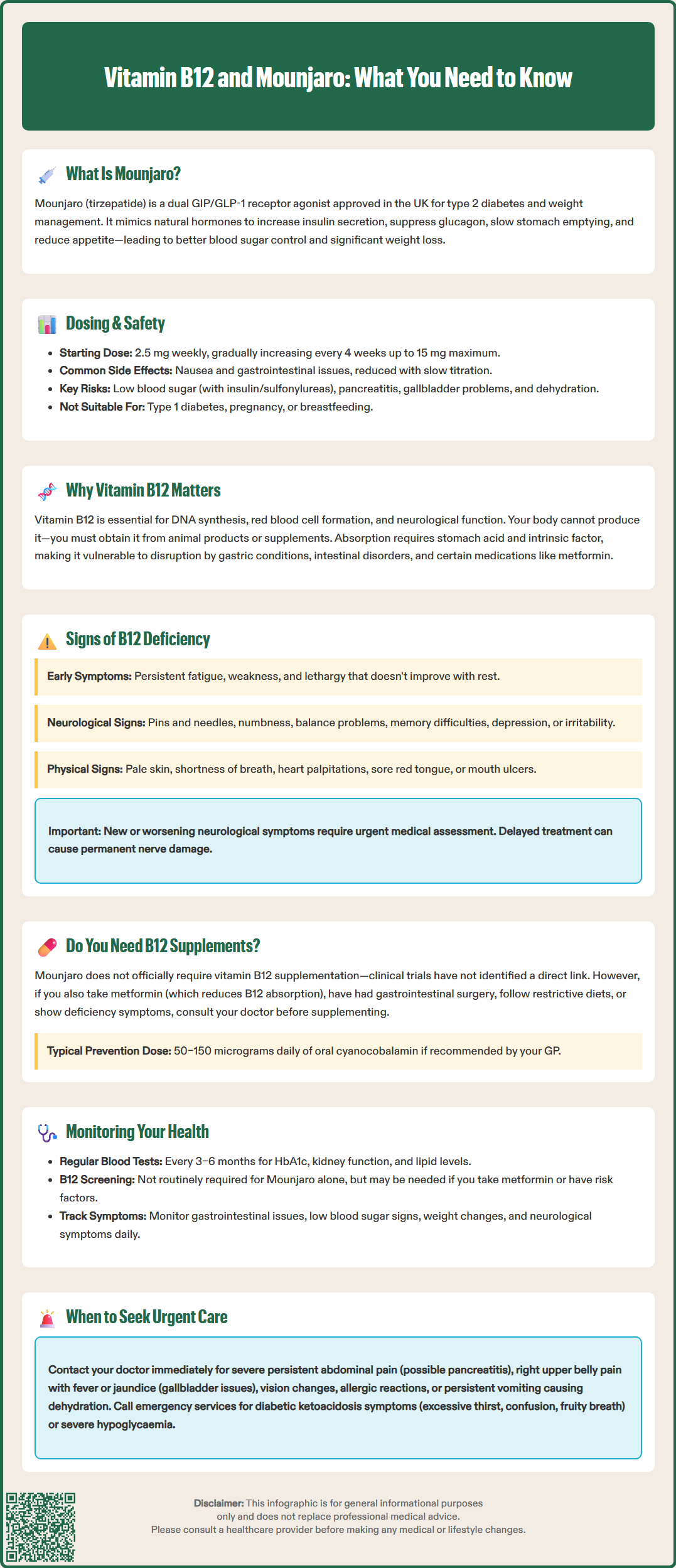
Vitamin B12 (cobalamin) is an essential water-soluble vitamin that plays critical roles in numerous physiological processes. It is fundamental for DNA synthesis, red blood cell formation, neurological function, and the metabolism of fatty acids and amino acids. The body cannot synthesise vitamin B12, so it must be obtained through dietary sources—primarily animal products such as meat, fish, dairy, and eggs—or through supplementation.
Absorption of vitamin B12 is a complex process requiring adequate stomach acid and intrinsic factor, a glycoprotein produced by gastric parietal cells. In the stomach, hydrochloric acid releases B12 from food proteins, after which it binds to intrinsic factor and travels to the terminal ileum for absorption. This intricate mechanism means that various factors can impair B12 absorption, including conditions affecting gastric acid production, intestinal disorders, and certain medications.
The liver stores substantial reserves of vitamin B12, typically sufficient for several years. However, when intake or absorption is compromised, deficiency can develop gradually. Neurological consequences of B12 deficiency can be particularly serious and may include peripheral neuropathy, subacute combined degeneration of the spinal cord, cognitive impairment, and mood disturbances. Haematological manifestations include macrocytic anaemia, which develops when impaired DNA synthesis affects rapidly dividing cells in the bone marrow.
Certain populations are at higher risk of vitamin B12 deficiency, including older adults (due to reduced gastric acid production), individuals following strict vegan or vegetarian diets, those with pernicious anaemia (an autoimmune condition affecting intrinsic factor production), patients who have undergone gastric or ileal surgery (including bariatric procedures), and those taking medications that affect gastric acid secretion (such as proton pump inhibitors or H2 antagonists) or intestinal absorption (including metformin). People with gastrointestinal disorders such as Crohn's disease or coeliac disease are also at increased risk.
Recognising vitamin B12 deficiency early is crucial, as neurological damage may become irreversible if left untreated. The clinical presentation can be insidious, with symptoms developing gradually over months or years. Common early symptoms include persistent fatigue, weakness, and lethargy that doesn't improve with rest. Many patients report feeling unusually tired despite adequate sleep, which can significantly impact daily functioning and quality of life.
Neurological symptoms are particularly concerning and may include paraesthesia (pins and needles) in the hands and feet, numbness, difficulty walking or balance problems, and muscle weakness. Some individuals experience cognitive changes such as memory difficulties, confusion, or difficulty concentrating—symptoms that can sometimes be mistaken for dementia in older adults. Mood disturbances, including depression and irritability, are also recognised manifestations of B12 deficiency.
Haematological signs include pallor, shortness of breath, and palpitations related to anaemia. Some patients develop a sore, red tongue (glossitis) or mouth ulcers. In severe cases, individuals may experience visual disturbances or more profound neuropsychiatric symptoms.
It is important to note that there is no official established link between Mounjaro and vitamin B12 deficiency in the current evidence base. However, patients taking medications that affect gastrointestinal function should remain vigilant for deficiency symptoms. If you experience any of these symptoms whilst taking Mounjaro or any other medication, contact your GP promptly.
New or worsening neurological symptoms (such as progressive numbness, ataxia, or significant cognitive changes) warrant urgent assessment and should not be ignored, as delayed treatment may result in permanent nerve damage. In cases of suspected B12 deficiency with neurological involvement, treatment should often begin promptly, even before test results are available. Blood tests including serum B12 levels can diagnose deficiency, and in some cases, additional tests such as intrinsic factor antibodies (to identify pernicious anaemia) may be appropriate.
The question of whether vitamin B12 supplementation is necessary when taking Mounjaro requires careful consideration of the available evidence and individual patient factors. Currently, there is no official clinical guidance recommending routine vitamin B12 supplementation specifically for patients prescribed tirzepatide. The prescribing information for Mounjaro does not list vitamin B12 deficiency as a recognised adverse effect, and clinical trials have not identified a direct mechanistic link between the medication and B12 status.
However, it is worth noting that another medication in the incretin-based therapy class—metformin—is well-established to reduce vitamin B12 absorption in some patients through effects on calcium-dependent ileal uptake mechanisms. The MHRA advises that metformin commonly reduces B12 levels and recommends testing if deficiency is suspected (for example, in patients with anaemia or neuropathy) and considering periodic monitoring in people with risk factors such as higher doses, longer duration of treatment, or other risk factors for deficiency. Many patients with type 2 diabetes take metformin alongside newer agents like Mounjaro, which may increase their overall risk of B12 deficiency.
The gastrointestinal effects of Mounjaro—including nausea, reduced appetite, and delayed gastric emptying—may theoretically affect nutritional intake and absorption, though this has not been specifically demonstrated for vitamin B12. Patients experiencing significant dietary restriction due to appetite suppression should ensure adequate nutritional intake across all essential vitamins and minerals.
Before starting any supplementation, discuss your individual circumstances with your GP or prescribing clinician. They can assess your risk factors for deficiency (including dietary patterns, concurrent medications, and medical history) and arrange baseline blood tests if appropriate. Unnecessary supplementation is not recommended, as it provides no additional benefit in individuals with adequate B12 status. If supplementation is advised, oral cyanocobalamin at doses of 50–150 micrograms daily is typically used for diet-related deficiency prevention, while intramuscular hydroxocobalamin is the standard treatment in the UK for pernicious anaemia or malabsorption conditions.
Comprehensive health monitoring is essential for all patients prescribed Mounjaro to ensure treatment safety and effectiveness whilst identifying any potential complications early. Your healthcare team will establish a monitoring schedule tailored to your individual needs, medical history, and treatment goals.
Regular blood tests form a cornerstone of monitoring. For patients with type 2 diabetes, HbA1c (glycated haemoglobin) measurements every 3–6 months assess glycaemic control and guide dose adjustments. Renal function tests are important, as GLP-1 receptor agonists can occasionally affect kidney function, particularly in patients with pre-existing renal impairment or those experiencing severe gastrointestinal side effects leading to dehydration. Lipid profiles may be monitored as weight loss often improves cardiovascular risk markers.
Whilst routine vitamin B12 screening is not standard for patients on Mounjaro alone, your GP may include this in monitoring if you have additional risk factors such as concurrent metformin use, a history of gastrointestinal surgery, strict dietary restrictions, or symptoms suggestive of deficiency. A full blood count can identify macrocytic anaemia, whilst serum B12 levels can help confirm deficiency. More specialised tests such as methylmalonic acid or homocysteine may be arranged by specialists if results are equivocal, though availability varies across UK laboratories.
Patient self-monitoring is equally important. Keep track of any new or worsening symptoms, particularly gastrointestinal disturbances, signs of hypoglycaemia (especially if taking insulin or sulfonylureas), or neurological symptoms. Maintain a record of your weight, blood glucose readings (if applicable), and any side effects. Report persistent nausea or vomiting to your healthcare provider, as severe symptoms may require dose adjustment or temporary treatment interruption.
When to seek urgent medical attention: Contact your GP promptly if you develop severe, persistent abdominal pain (which could indicate pancreatitis), right upper quadrant pain, fever or jaundice (possible gallbladder disease), visual changes, signs of allergic reaction, or persistent vomiting leading to dehydration. Seek immediate medical help if you experience symptoms of diabetic ketoacidosis (excessive thirst, frequent urination, confusion, fruity-smelling breath) or severe hypoglycaemia. Regular engagement with your healthcare team, adherence to monitoring schedules, and prompt reporting of concerns will optimise your treatment outcomes and safety whilst taking Mounjaro.
If you suspect an adverse reaction to Mounjaro or any other medication, you can report this through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
There is currently no established clinical evidence linking Mounjaro (tirzepatide) to vitamin B12 deficiency. The prescribing information does not list B12 deficiency as a recognised adverse effect, and clinical trials have not identified a direct mechanistic link between the medication and B12 status.
Routine vitamin B12 supplementation is not recommended for patients taking Mounjaro unless you have additional risk factors for deficiency or symptoms suggestive of low B12 levels. Discuss your individual circumstances with your GP, who can assess whether testing or supplementation is appropriate for you.
Key symptoms include persistent fatigue, paraesthesia (pins and needles) in hands or feet, numbness, difficulty walking or balance problems, memory difficulties, mood changes, and pallor. New or worsening neurological symptoms warrant prompt medical assessment, as delayed treatment may result in permanent nerve damage.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.