
Glucagon-like peptide-1 (GLP-1) receptor agonists are established treatments for type 2 diabetes mellitus and obesity in the UK, typically administered via subcutaneous injection. Whilst transdermal patch formulations represent an area of ongoing pharmaceutical research, no GLP-1 patches are currently licensed by the Medicines and Healthcare products Regulatory Agency (MHRA) or approved by the National Institute for Health and Care Excellence (NICE) for use in the United Kingdom. This article examines the theoretical application sites and best practices for GLP-1 patches, should such formulations become available, drawing on established principles for transdermal medication delivery systems used in UK clinical practice.
Quick Answer: No GLP-1 patches are currently licensed for use in the UK by the MHRA or approved by NICE.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereThe theoretical mechanism of a GLP-1 patch would involve delivering the active pharmaceutical ingredient through the skin (transdermally) into the systemic circulation. GLP-1 receptor agonists work by mimicking the action of endogenous incretin hormones, which are released from the gut in response to food intake. These agents enhance glucose-dependent insulin secretion from pancreatic beta cells, suppress inappropriate glucagon release, slow gastric emptying, and promote satiety through central nervous system pathways. This multifaceted mechanism helps improve glycaemic control and can support weight reduction, as outlined in NICE guideline NG28 for type 2 diabetes management.
Transdermal delivery systems could potentially offer advantages over subcutaneous injections, including improved patient acceptability and reduced injection-site reactions. However, the large molecular size of GLP-1 analogues presents significant formulation challenges for transdermal delivery. Any future GLP-1 patch would require robust clinical trial evidence demonstrating efficacy, safety, and pharmacokinetic profiles comparable to existing injectable formulations before regulatory approval could be granted. Patients should only use medications prescribed by their healthcare professional and should not attempt to source unlicensed transdermal products, in line with MHRA guidance on buying medicines safely.
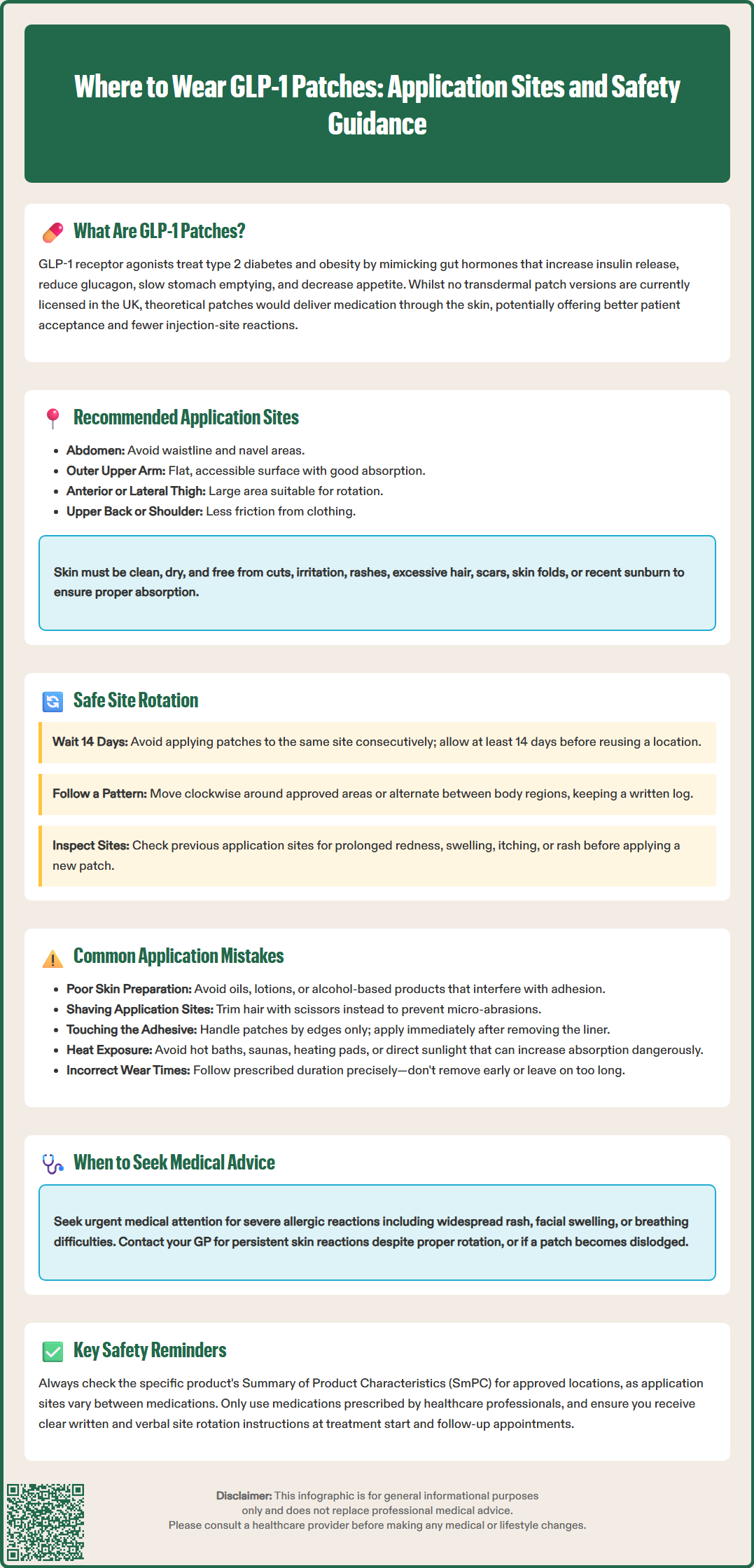
Although GLP-1 patches are not currently available in the UK, understanding optimal application sites for transdermal medication delivery is important for healthcare professionals and patients who may encounter such products in the future or in research settings. Transdermal patches generally require application to areas of skin that provide consistent drug absorption whilst minimising irritation and mechanical disruption.
Typical anatomical sites for transdermal patches may include:
Abdomen: The abdominal area (avoiding the waistline and navel) offers a relatively large, flat surface with consistent subcutaneous tissue and good blood supply.
Upper arm: The outer aspect of the upper arm provides an accessible site with adequate skin surface area and is commonly used for various patch medications.
Thigh: The anterior or lateral thigh offers another large application area with relatively consistent skin characteristics.
Upper back or shoulder area: These sites may be appropriate for patches requiring less frequent patient access, though they can be difficult for self-application.
It is important to note that permitted application sites vary significantly between different transdermal medications. For example, the rivastigmine patch (Exelon®) SmPC specifies application to the upper or lower back, upper arm, or chest, while certain hormone replacement therapy patches have different site recommendations.
When selecting an application site, several factors must be considered. The skin should be clean, dry, and free from cuts, irritation, rashes, or excessive hair. Areas with significant skin folds, scars, or recent sunburn should be avoided. The site should not be subject to excessive friction from clothing or movement, as this may compromise patch adhesion or drug delivery.
Patients should always follow the specific instructions provided with any licensed transdermal medication, as optimal sites will vary depending on the formulation's characteristics and the manufacturer's validated application protocols as detailed in the product's Summary of Product Characteristics (SmPC) and Patient Information Leaflet (PIL).
Site rotation is a fundamental principle in the administration of any medication requiring repeated application to the skin, whether transdermal patches or subcutaneous injections. Proper rotation helps prevent local skin complications, maintains consistent drug absorption, and improves treatment tolerability over time.
Key principles of site rotation include:
Avoid reusing the same site consecutively: The interval before reapplying a patch to the same location varies by product. For example, the rivastigmine patch SmPC recommends a minimum of 14 days before reusing the same site. Always follow the specific rotation schedule in the product's SmPC and PIL.
Maintain a systematic rotation pattern: Patients should develop a consistent rotation schedule, such as moving clockwise around permitted application areas or alternating between different approved body regions. Keeping a written log or using a smartphone application can help track application sites.
Inspect previous sites regularly: Before applying a new patch, examine previous application sites for signs of skin reaction, including persistent redness, swelling, itching, or rash. Mild, transient erythema immediately after patch removal is common, but prolonged or severe reactions warrant medical review.
Use different areas within approved sites: When applying patches to the same general area (such as the abdomen), use a different location within that area for each application, following product-specific guidance.
Patients should seek urgent medical attention if they experience signs of a severe allergic reaction (such as widespread rash, facial or tongue swelling, or breathing difficulties) or extensive skin reactions. For less severe but persistent skin reactions, despite appropriate site rotation, patients should contact their GP or specialist nurse. In some cases, skin reactions may indicate contact dermatitis or adhesive sensitivity, which may require alternative treatment approaches.
Healthcare professionals should provide clear written and verbal instructions on site rotation during treatment initiation and reinforce these principles at follow-up appointments. Suspected adverse reactions to any medicine should be reported via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Understanding potential errors in patch application is essential for optimising therapeutic outcomes and minimising adverse effects. Although GLP-1 patches are not currently licensed in the UK, the following guidance applies broadly to transdermal medication systems and would be relevant should such products become available.
Application to inappropriate skin areas: Patients may inadvertently apply patches to sites with excessive hair, active skin conditions, or areas prone to friction. Hair can interfere with adhesion and drug absorption; if hair removal is necessary, patients should use scissors to trim rather than shaving, which can cause micro-abrasions. Never apply patches over broken, irritated, or diseased skin.
Inadequate skin preparation: Failing to properly clean and dry the application site is a frequent error. Skin should be washed with mild soap and water, then thoroughly dried. Avoid using oils, lotions, or alcohol-based products immediately before application, as these can interfere with patch adhesion or alter drug absorption rates.
Incorrect patch handling: Touching the adhesive surface excessively or the medication-containing side of the patch can reduce adhesion and potentially affect drug delivery. Patients should handle patches by their edges and apply them immediately after removing the protective liner. Patches should never be cut unless specifically permitted by the product's PIL.
Applying heat to the patch site: Exposure to external heat sources (hot baths, saunas, heating pads, or direct sunlight) can increase drug absorption rates unpredictably, potentially leading to adverse effects. The MHRA has issued Drug Safety Updates highlighting this risk with various transdermal products. Patients should be counselled to avoid such exposures unless the product information specifically states otherwise.
Premature patch removal or extended wear time: Removing a patch before the prescribed duration or leaving it on beyond the recommended time can compromise treatment effect. If a patch becomes dislodged, patients should follow the specific guidance provided with their medication or contact their healthcare provider for advice.
Healthcare professionals should provide comprehensive patient education at treatment initiation, including written instructions and, where possible, practical demonstration. Regular follow-up allows identification and correction of application errors, supporting treatment adherence and optimal clinical outcomes. Additional adhesive tapes or occlusive dressings should only be used if specifically permitted by the product information.
No, there are currently no GLP-1 patches licensed by the MHRA or approved by NICE for use in the United Kingdom. Patients should only use licensed GLP-1 medications prescribed by their healthcare professional.
Common sites for transdermal patches include the abdomen (avoiding waistline and navel), outer upper arm, anterior or lateral thigh, and upper back or shoulder area. Specific permitted sites vary by product and must follow the manufacturer's Summary of Product Characteristics.
Site rotation intervals vary by product, but typically a minimum of 14 days should elapse before reapplying a patch to the same location. Patients should follow a systematic rotation pattern and maintain a written log to track application sites and prevent skin complications.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.