
Mounjaro (tirzepatide) is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus. Whilst effective for glycaemic control, constipation is a common adverse effect, occurring in 1–10% of patients. This digestive symptom arises primarily because Mounjaro slows gastric emptying and reduces intestinal motility, allowing increased water reabsorption from stools. Understanding why Mounjaro causes constipation—and how to manage it—helps patients maintain treatment adherence whilst minimising discomfort. This article explores the mechanisms, risk factors, and evidence-based strategies for preventing and managing constipation during tirzepatide therapy.
Quick Answer: Mounjaro causes constipation by slowing gastric emptying and reducing intestinal motility through GLP-1 and GIP receptor activation, which increases water reabsorption from stools and results in harder, more difficult-to-pass bowel movements.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMounjaro (tirzepatide) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Whilst its primary therapeutic action involves improving glycaemic control, the medication exerts significant effects on the gastrointestinal system that can lead to various digestive symptoms.
The drug works by mimicking naturally occurring incretin hormones that regulate blood glucose levels and appetite. When administered, Mounjaro slows gastric emptying—the rate at which food moves from the stomach into the small intestine. This delayed gastric emptying is a key mechanism through which the medication helps patients feel fuller for longer periods, thereby reducing overall caloric intake.
This alteration in normal digestive transit has downstream consequences throughout the gastrointestinal tract. The slowing of gut motility primarily affects the stomach but may also affect intestinal transit, where the movement of digestive contents can become less efficient. This reduced intestinal motility may contribute to constipation, as waste material moves more slowly through the colon, allowing more water to be absorbed and resulting in harder, more difficult-to-pass stools.
Additionally, Mounjaro influences the enteric nervous system—the complex network of nerves governing digestive function. By modulating gut-brain signalling pathways, the medication can alter normal peristaltic movements (the wave-like muscle contractions that propel contents through the digestive tract), further contributing to changes in bowel habits that many patients experience during treatment.
Importantly, the UK SmPC notes that Mounjaro is not recommended in patients with severe gastrointestinal disease, including severe gastroparesis, due to its effects on digestive function.
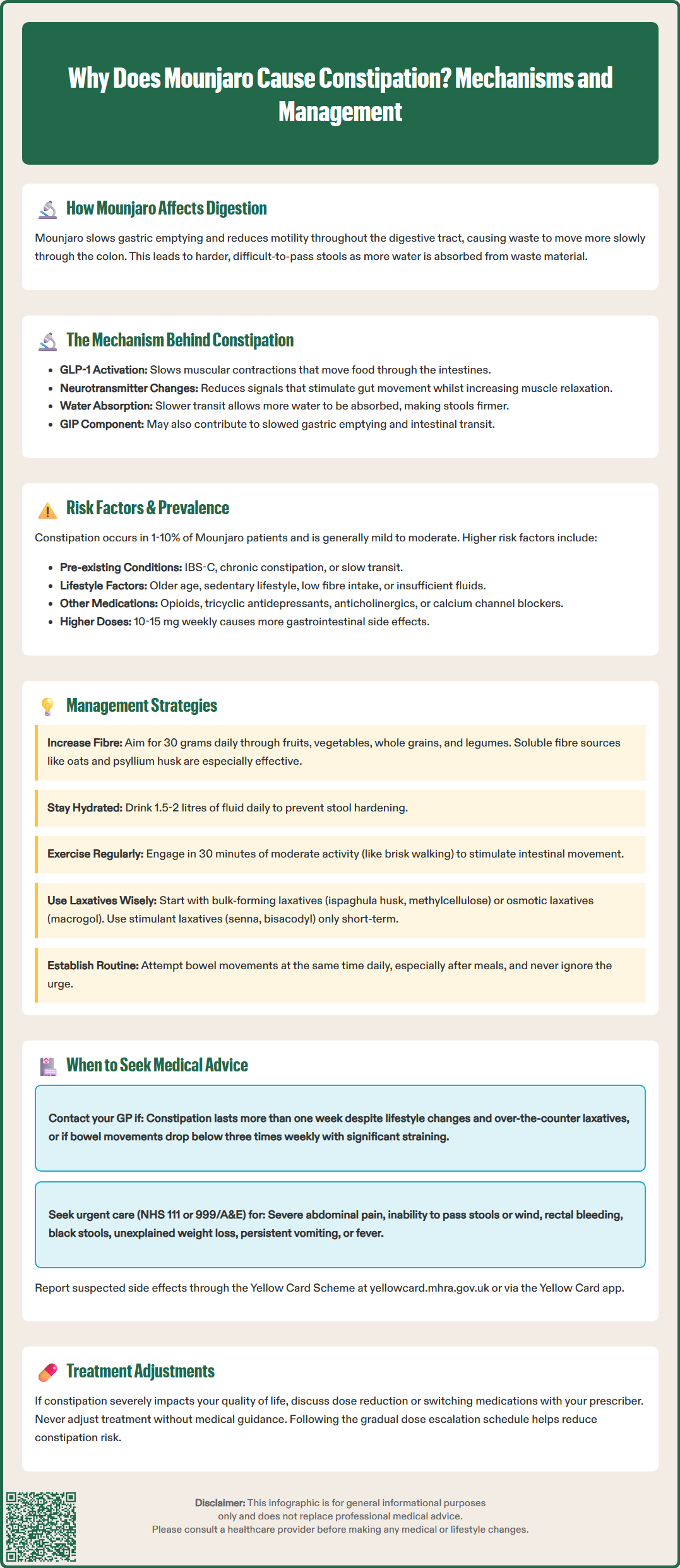
Understanding the pharmacological mechanisms by which Mounjaro causes constipation requires examining how GIP and GLP-1 receptor activation affects intestinal physiology. GLP-1 receptor agonists are well-documented to reduce gastrointestinal motility, particularly gastric emptying, with variable effects on intestinal transit.
When tirzepatide binds to GLP-1 receptors located throughout the gastrointestinal tract, it triggers a cascade of cellular responses that ultimately slow the coordinated muscular contractions responsible for moving digestive contents forward. This occurs through several pathways: the medication may reduce the release of certain neurotransmitters that stimulate gut motility, whilst simultaneously enhancing inhibitory signals that relax intestinal smooth muscle. The net effect is a generalised slowing of transit time, particularly in the upper gastrointestinal tract.
The GIP component of Mounjaro's action adds another layer of complexity. Whilst GIP's effects on gut motility are less extensively studied than those of GLP-1, research suggests that GIP receptor activation may also influence gastric emptying and intestinal transit, though the precise contribution to constipation remains under investigation.
The prolonged contact time between stool and the colonic mucosa allows for increased water reabsorption, contributing to firmer stool consistency. These mechanisms collectively explain why constipation is classified as a 'common' adverse effect in the UK SmPC for tirzepatide.
It's worth noting that the effects on gastric emptying may demonstrate some tachyphylaxis (diminishing response) with continued therapy, though the impact of this on constipation symptoms varies between individuals.
According to the UK SmPC for Mounjaro, constipation is classified as a 'common' adverse effect, occurring in between 1% and 10% of patients. Clinical trial data from the SURPASS programme, which evaluated tirzepatide across multiple studies, consistently identified constipation as one of the frequent gastrointestinal adverse events, though it was generally classified as mild to moderate in severity.
Several patient-specific factors appear to increase the likelihood of developing constipation whilst taking Mounjaro. Pre-existing gastrointestinal conditions, particularly irritable bowel syndrome with constipation (IBS-C) or chronic constipation, significantly elevate risk. Patients with a history of slow gut transit are more vulnerable to the additional motility-slowing effects of the medication. Age is another consideration, as older adults naturally experience reduced intestinal motility and may be more susceptible to medication-induced constipation.
Dietary habits play a crucial role in determining individual risk. Patients consuming diets low in dietary fibre are at substantially higher risk, as adequate fibre intake is essential for maintaining normal bowel function. Similarly, insufficient fluid intake compounds the problem, as hydration status directly affects stool consistency. The appetite-suppressing effects of Mounjaro may inadvertently lead some patients to reduce their overall food and fluid intake, creating a perfect storm for constipation development.
Concomitant medications must also be considered. Patients taking other drugs known to cause constipation—such as opioid analgesics, tricyclic antidepressants, anticholinergic medicines (including some first-generation antihistamines), or calcium channel blockers—face compounded risk. Dose escalation patterns influence constipation prevalence as well; higher doses of Mounjaro (10 mg and 15 mg weekly) are associated with increased rates of gastrointestinal adverse effects compared to lower starting doses. Following the gradual dose escalation schedule recommended in the SmPC can help mitigate these effects. Physical activity levels matter too, as sedentary lifestyles independently contribute to sluggish bowel function.
Effective management of Mounjaro-related constipation begins with proactive lifestyle modifications that should ideally commence at treatment initiation. Increasing dietary fibre intake to approximately 30 grams daily (as recommended by the Scientific Advisory Committee on Nutrition) is fundamental; this can be achieved through consuming more fruits, vegetables, whole grains, legumes, and pulses. Soluble fibre sources such as oats, psyllium husk, and linseeds are particularly beneficial as they help soften stools and promote regular bowel movements.
Adequate hydration is equally critical. Patients should aim for 1.5-2 litres of fluid daily (unless contraindicated by other medical conditions), as proper hydration prevents excessive stool hardening. Water is the optimal choice, though herbal teas and diluted fruit juices can contribute to fluid intake. Regular physical activity—even moderate exercise such as 30 minutes of brisk walking daily—stimulates intestinal motility and can significantly improve bowel regularity.
When lifestyle measures prove insufficient, pharmacological interventions may be warranted. Bulk-forming laxatives such as ispaghula husk (Fybogel) or methylcellulose are generally considered first-line options for simple constipation, as they work by increasing stool mass and stimulating peristalsis. These should be taken with adequate water to prevent paradoxical worsening of constipation and are not recommended when fluid intake is poor or in opioid-induced constipation. Osmotic laxatives like macrogol (Movicol, Laxido) are effective alternatives that work by drawing water into the bowel, softening stools and easing passage.
For more resistant cases, stimulant laxatives such as senna or bisacodyl may be used short-term or intermittently; longer-term use should only be under medical supervision. Stool softeners like docusate sodium can be helpful adjuncts. Patients should consult their pharmacist or GP before combining multiple laxatives.
Establishing a regular toileting routine—attempting to open bowels at the same time each day, particularly after meals when the gastrocolic reflex is strongest—can help retrain bowel habits. Patients should never ignore the urge to defecate, as delaying can worsen constipation over time.
Whilst mild constipation during Mounjaro treatment can often be managed with self-care measures, certain symptoms warrant prompt medical evaluation. Patients should contact their GP or diabetes specialist nurse if constipation persists for more than one week despite implementing lifestyle modifications and over-the-counter laxatives, or if bowel movements become increasingly infrequent (fewer than three times weekly with significant straining).
Red flag symptoms requiring urgent medical attention include severe abdominal pain, particularly if accompanied by distension or rigidity; complete inability to pass stools or wind (which may indicate bowel obstruction); rectal bleeding or passage of black, tarry stools; unexplained weight loss beyond that expected from Mounjaro's therapeutic effects; persistent nausea and vomiting; or fever accompanying constipation. These symptoms could indicate serious complications such as bowel obstruction, perforation, or other gastrointestinal pathology requiring immediate investigation. Patients should call NHS 111 or seek emergency care (999/A&E) if they suspect bowel obstruction or have severe acute abdominal symptoms.
Patients experiencing severe or intolerable constipation that significantly impacts quality of life should discuss treatment options with their prescriber. In some cases, dose reduction may be appropriate, or switching to an alternative glucose-lowering medication might be considered if symptoms prove unmanageable. However, such decisions should always be made in consultation with healthcare professionals, weighing the benefits of glycaemic control against the burden of adverse effects.
It is important to note that new-onset constipation in patients previously having regular bowel habits, or a sudden change in established bowel patterns, should always be evaluated medically. Whilst Mounjaro is a likely culprit in patients taking the medication, other causes must be excluded. NICE guidance (NG12) recommends that persistent changes in bowel habit, particularly in patients aged 60 or over, should prompt consideration of appropriate investigations, including possible faecal immunochemical testing (FIT), to rule out colorectal cancer. Patients should maintain open communication with their healthcare team throughout treatment, reporting any concerning symptoms promptly.
Patients are encouraged to report suspected adverse reactions to Mounjaro via the Yellow Card Scheme at yellowcard.mhra.gov.uk or via the Yellow Card app.
According to the UK SmPC, constipation is classified as a common adverse effect of Mounjaro, occurring in between 1% and 10% of patients. Clinical trial data from the SURPASS programme consistently identified constipation as a frequent gastrointestinal adverse event, though it was generally mild to moderate in severity.
Increasing dietary fibre intake to approximately 30 grams daily, maintaining adequate hydration of 1.5–2 litres of fluid daily, and engaging in regular physical activity such as 30 minutes of brisk walking can significantly help prevent and manage constipation. Establishing a regular toileting routine after meals is also beneficial.
Contact your GP if constipation persists for more than one week despite self-care measures, or if you experience red flag symptoms including severe abdominal pain, complete inability to pass stools or wind, rectal bleeding, black tarry stools, unexplained weight loss, persistent vomiting, or fever. These may indicate serious complications requiring urgent medical evaluation.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.