Many patients prescribed glucagon-like peptide-1 (GLP-1) receptor agonists for type 2 diabetes or weight management wonder why their medication doesn't seem to be working as expected. GLP-1 medications—including semaglutide, liraglutide, and dulaglutide—work by mimicking a natural hormone that regulates blood glucose and appetite. However, treatment response varies considerably between individuals, and several factors can influence effectiveness. These include dosage and administration technique, realistic timeframes for results, lifestyle factors, concurrent medications, and underlying medical conditions. Understanding why your GLP-1 therapy may not be delivering anticipated results is essential for working with your healthcare team to optimise treatment outcomes and achieve your therapeutic goals.
Quick Answer: GLP-1 medications may not work as expected due to inadequate dosage, incorrect administration technique, insufficient treatment duration, lifestyle factors, concurrent medications, advanced beta-cell dysfunction, or unrealistic expectations about timeframes and outcomes.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists are increasingly prescribed for type 2 diabetes management and, in some cases, weight management. These medications work by mimicking the action of the naturally occurring GLP-1 hormone, which stimulates insulin secretion, suppresses glucagon release, slows gastric emptying, and reduces appetite. However, some patients report that their GLP-1 medication does not appear to be working as anticipated.
Several factors can contribute to perceived treatment failure. Individual variation in drug response is significant—biological differences in GLP-1 receptor expression and function may contribute to why some patients naturally respond more robustly than others, though this is not routinely assessed in clinical practice. Secondly, unrealistic expectations about the speed or magnitude of results can lead to premature conclusions about efficacy. Weight loss with GLP-1 therapy is typically gradual rather than dramatic, and glycaemic improvements may take several weeks to become apparent.
Lifestyle factors play a crucial role in treatment outcomes. GLP-1 medications are designed to work alongside dietary modifications and increased physical activity, not as standalone solutions. Patients who continue high-calorie diets or remain sedentary may experience limited benefits. Additionally, certain medications can counteract GLP-1 effects—for example, corticosteroids can raise blood glucose levels, whilst some psychiatric medications may increase appetite or promote weight gain.
It is also worth noting that 'not working' can mean different things to different patients—some may focus on weight changes, others on blood glucose readings, and some on symptom relief. Clarifying treatment goals with your healthcare provider ensures that progress is measured appropriately and that expectations align with clinical evidence.
Importantly, GLP-1 receptor agonists are not indicated for type 1 diabetes or diabetic ketoacidosis, and should not be co-prescribed with DPP-4 inhibitors (such as sitagliptin or linagliptin). In the UK, only specific GLP-1 medications at certain doses are licensed for weight management (liraglutide 3mg and semaglutide 2.4mg), while others are approved solely for type 2 diabetes.
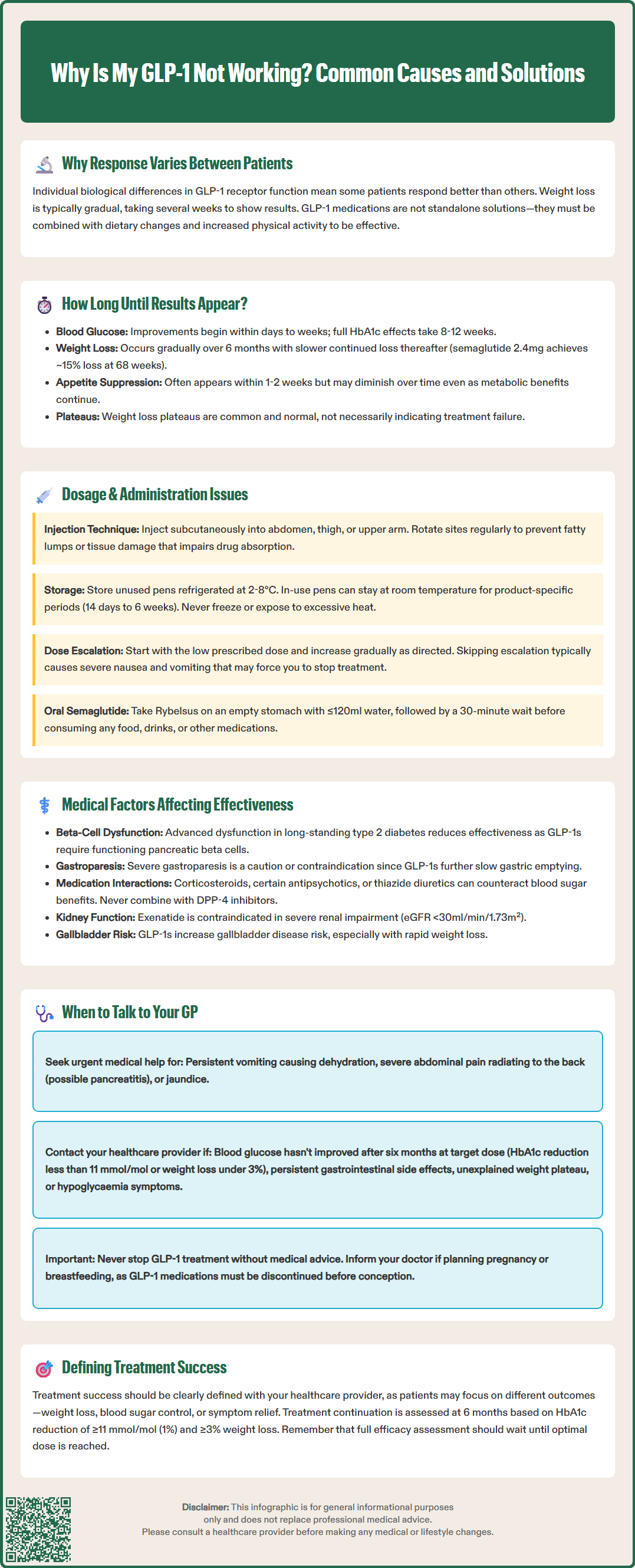
Understanding the expected timeline for GLP-1 medication effects is essential for setting realistic expectations and avoiding premature discontinuation. The pharmacological action of these drugs begins shortly after administration, but clinically meaningful outcomes develop over different timeframes depending on the specific measure being assessed.
For glycaemic control in type 2 diabetes, patients may notice improvements in blood glucose levels within the first few days to weeks of treatment. However, the full effect on HbA1c—the standard measure of long-term glucose control—typically requires 8 to 12 weeks to become apparent. This is because HbA1c reflects average blood glucose over the preceding two to three months. According to NICE guidance (NG28), the continuation of GLP-1 receptor agonist therapy in type 2 diabetes should be assessed after six months, with treatment continued only if there is a reduction in HbA1c of at least 11 mmol/mol (1%) and, where applicable, a weight loss of at least 3% of initial body weight.
Weight loss outcomes follow a more gradual trajectory. Clinical trials demonstrate that most weight reduction occurs over the first six months of treatment, with continued but slower loss thereafter. The magnitude of weight loss varies considerably by product and dose. For example, semaglutide 2.4mg (Wegovy) has demonstrated approximately 15% weight loss at 68 weeks in clinical trials, while liraglutide 3mg (Saxenda) typically achieves around 8% at 56 weeks. GLP-1 medications at doses licensed for diabetes often produce more modest weight loss of 2-6kg. It is important to recognise that weight loss is rarely linear—plateaus are common and do not necessarily indicate treatment failure.
Appetite suppression and satiety effects are often noticed more quickly, sometimes within the first week or two of treatment. However, these subjective effects can diminish over time as the body adapts, even whilst the medication continues to exert metabolic benefits. Dose escalation, which is standard practice with most GLP-1 medications, helps to optimise therapeutic effects whilst minimising gastrointestinal side effects. Patience during this titration period is crucial, as premature judgement of efficacy may occur before the optimal dose has been reached.
Proper administration technique and consistent adherence are fundamental to achieving optimal outcomes with GLP-1 medications. These injectable therapies require specific handling and administration methods, and errors in technique can significantly compromise efficacy.
Injection technique matters considerably. GLP-1 medications are administered subcutaneously (under the skin) into areas with adequate subcutaneous fat—typically the abdomen, thigh, or upper arm. Injecting into muscle rather than subcutaneous tissue can alter absorption rates and reduce effectiveness. The injection site should be rotated regularly to prevent lipohypertrophy (fatty lumps) or lipoatrophy (fat loss), both of which can impair drug absorption. Patients should ensure they are using the correct needle length and injection angle as demonstrated by their practice nurse or diabetes specialist.
Storage and handling requirements must be followed meticulously. Unused GLP-1 pens should be refrigerated between 2°C and 8°C, whilst in-use pens can typically be kept at room temperature (below 30°C) for a product-specific period. This varies considerably: dulaglutide (Trulicity) for 14 days, liraglutide (Victoza/Saxenda) for 30 days, and semaglutide (Ozempic/Wegovy) for 6 weeks. Some pens are single-use only. Always follow the specific storage instructions in your medication's patient information leaflet. Exposure to excessive heat or freezing temperatures can denature the protein-based medication, rendering it ineffective. Always check the expiry date and inspect the solution for discolouration or particles before use.
Adherence to the prescribed schedule is critical. For weekly formulations, the specific guidance for missed doses and changing administration day varies by product. Most require a minimum of 3 days between doses, and missed-dose windows range from 3-5 days depending on the specific medication. For daily formulations, consistent timing is important. Always follow the specific guidance provided in your medication's patient information leaflet or SmPC (Summary of Product Characteristics).
Dose escalation protocols exist for good reason. Most GLP-1 therapies begin at a low dose and gradually increase over several weeks. This titration minimises gastrointestinal side effects whilst allowing the body to adapt. Some patients or prescribers may be tempted to accelerate this process, but doing so often leads to intolerable nausea and vomiting, potentially causing treatment discontinuation before therapeutic doses are reached.
For oral semaglutide (Rybelsus), administration requirements are particularly strict. It must be taken on an empty stomach with a small sip of water (no more than 120ml), followed by at least 30 minutes without food, drink or other oral medications. Failure to follow these instructions can significantly reduce absorption and effectiveness.
Various underlying medical conditions and physiological factors can influence how well GLP-1 medications work for individual patients. Understanding these variables helps to identify potential barriers to treatment success and guides appropriate management strategies.
Advanced beta-cell dysfunction in long-standing type 2 diabetes can limit GLP-1 efficacy. These medications work partly by enhancing glucose-dependent insulin secretion from pancreatic beta cells. In patients with significant beta-cell failure—often those who have had diabetes for many years—there may be insufficient insulin-secreting capacity remaining for GLP-1 agonists to stimulate effectively. In such cases, combination therapy with basal insulin or other agents may be necessary, or alternative treatment approaches might be more appropriate.
Gastrointestinal conditions can affect both drug absorption and tolerability. Severe gastroparesis (delayed gastric emptying) is a caution or contraindication for some GLP-1 medications, as these drugs further slow gastric emptying and may exacerbate symptoms. Conversely, conditions causing rapid gastric transit or malabsorption might theoretically affect drug uptake, though this is less well-documented given the subcutaneous route of administration for most GLP-1 therapies. Inflammatory bowel disease, previous gastric surgery, or other structural gastrointestinal abnormalities may also influence treatment response.
Concurrent medications can interact with GLP-1 therapy in various ways. Drugs that raise blood glucose (such as corticosteroids, certain antipsychotics, or thiazide diuretics) may counteract glycaemic benefits. Medications that slow gastric emptying or affect gastrointestinal motility might compound GLP-1-related nausea. The delayed gastric emptying caused by GLP-1 medications can affect the absorption of oral medications, particularly those requiring rapid absorption or those with narrow therapeutic windows. This is especially relevant for immediate-release exenatide, where timing with other oral medicines may need adjustment. GLP-1 receptor agonists should not be co-prescribed with DPP-4 inhibitors, as this combination is not recommended in UK practice.
Renal and hepatic function may influence treatment outcomes. Most GLP-1 medications do not require dose adjustment in mild to moderate renal or hepatic impairment. However, exenatide is contraindicated in severe renal impairment (eGFR <30ml/min/1.73m²). Severe gastrointestinal side effects from any GLP-1 medication can cause dehydration, potentially leading to acute kidney injury, so prompt medical review is advised if persistent vomiting occurs.
Gallbladder disease risk is increased with GLP-1 receptor agonists, particularly with substantial or rapid weight loss. Symptoms such as persistent right upper quadrant pain, fever, or jaundice should prompt urgent medical assessment. This risk may affect treatment continuation in some patients.
Knowing when to seek medical advice about your GLP-1 therapy is essential for optimising treatment outcomes and ensuring patient safety. Whilst some degree of trial and adjustment is normal, certain situations warrant prompt discussion with your healthcare provider.
You should contact your GP or diabetes care team if:
No improvement in blood glucose control after six months at the target maintenance dose, particularly if HbA1c reduction is less than 11 mmol/mol (1%) and weight loss is less than 3% where applicable (NICE NG28 continuation criteria for type 2 diabetes)
Persistent or severe gastrointestinal side effects (nausea, vomiting, diarrhoea, or abdominal pain) that do not improve with time or dose adjustment, as these may indicate intolerance requiring treatment modification
Persistent vomiting or inability to keep fluids down, which can lead to dehydration and acute kidney injury requiring urgent assessment
Unexplained weight loss plateau or weight regain after initial success, which might suggest the need for dose optimisation, lifestyle review, or investigation of other contributing factors
Signs of hypoglycaemia (shakiness, sweating, confusion, rapid heartbeat), especially if you are taking GLP-1 medication alongside insulin or sulfonylureas
Symptoms of pancreatitis, including severe, persistent abdominal pain radiating to the back, often accompanied by nausea and vomiting—stop the medication immediately and seek urgent medical assessment (call 999 or go to A&E if symptoms are severe)
Persistent right upper quadrant pain, fever or jaundice, which could indicate gallbladder problems
Changes in vision or symptoms of diabetic retinopathy, as rapid improvements in glucose control can occasionally worsen existing eye disease
Difficulty with injection technique or concerns about proper medication storage and handling
Planning pregnancy or breastfeeding, as GLP-1 receptor agonists are not recommended during pregnancy or lactation and should be discontinued in advance of conception
Your healthcare provider can assess multiple factors that might be affecting treatment response, including adherence patterns, injection technique, concurrent medications, and lifestyle factors. They may recommend dose adjustments, additional investigations (such as C-peptide levels to assess beta-cell function), combination therapy with other diabetes medications, or switching to an alternative GLP-1 formulation or drug class.
Regular monitoring is part of good diabetes care. Even if you feel your medication is not working optimally, do not stop treatment without medical advice. Abrupt discontinuation can lead to deterioration in glycaemic control. Your GP can work with you to develop a revised treatment plan that addresses your concerns whilst maintaining safety and working towards your therapeutic goals. Remember that diabetes management is a partnership between you and your healthcare team, and open communication about treatment effectiveness is crucial for achieving the best possible outcomes.
If you experience any suspected side effects from your GLP-1 medication, you can report these through the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk, which helps monitor medication safety across the UK.
You should allow at least 8–12 weeks to assess glycaemic improvements and up to six months for full evaluation of both blood glucose control and weight outcomes. NICE guidance recommends formal assessment at six months, with continuation criteria including HbA1c reduction of at least 11 mmol/mol and weight loss of at least 3% where applicable.
Yes, injection technique significantly affects GLP-1 effectiveness. The medication must be injected subcutaneously (under the skin) rather than into muscle, using proper needle length and angle. Rotating injection sites prevents lipohypertrophy or lipoatrophy, both of which impair drug absorption and reduce treatment efficacy.
Contact your GP or diabetes care team for assessment. They can evaluate adherence, injection technique, lifestyle factors, concurrent medications, and whether dose optimisation or combination therapy is needed. Do not stop treatment without medical advice, as abrupt discontinuation can worsen glycaemic control.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.