Accidentally taking a double dose of Ozempic (semaglutide) is a concerning but usually manageable situation that requires prompt attention and monitoring. Ozempic is a glucagon-like peptide-1 (GLP-1) receptor agonist prescribed for type 2 diabetes management in the UK. Whilst an accidental double dose is not typically life-threatening, it significantly increases the risk of adverse effects, particularly gastrointestinal symptoms and low blood sugar. Understanding what to expect, when to seek medical help, and how to prevent future incidents is essential for anyone using this medication. This article provides comprehensive guidance on managing an accidental Ozempic overdose safely.
Quick Answer: An accidental double dose of Ozempic increases the risk of gastrointestinal symptoms and low blood sugar but is rarely life-threatening, requiring close monitoring and medical advice.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist prescribed for type 2 diabetes management in the UK. The medication works by mimicking the action of the naturally occurring hormone GLP-1, which stimulates insulin secretion, suppresses glucagon release, slows gastric emptying, and reduces appetite. When administered at the prescribed dose—typically starting at 0.25 mg weekly and titrating up to a maintenance dose of 0.5 mg, 1 mg, or 2 mg weekly—Ozempic is generally well tolerated.
Taking an accidental double dose of Ozempic means you have administered twice your prescribed weekly amount in a single injection. Whilst this is not typically life-threatening, it significantly increases your risk of experiencing adverse effects, particularly gastrointestinal symptoms. The severity of symptoms depends on several factors, including your current dose level, how long you have been taking the medication, your individual tolerance, and your overall health status.
Key considerations following a double dose:
The medication cannot be removed from your system once injected
Effects may persist for up to several weeks due to Ozempic's long half-life (approximately one week)
Your blood glucose levels may drop lower than usual, particularly if you also take insulin or sulphonylureas
Gastrointestinal side effects are likely to be more pronounced
It is important to understand that whilst an accidental double dose is concerning, most patients experience manageable symptoms that resolve without serious complications. However, monitoring yourself closely and knowing when to seek medical advice is essential for your safety.
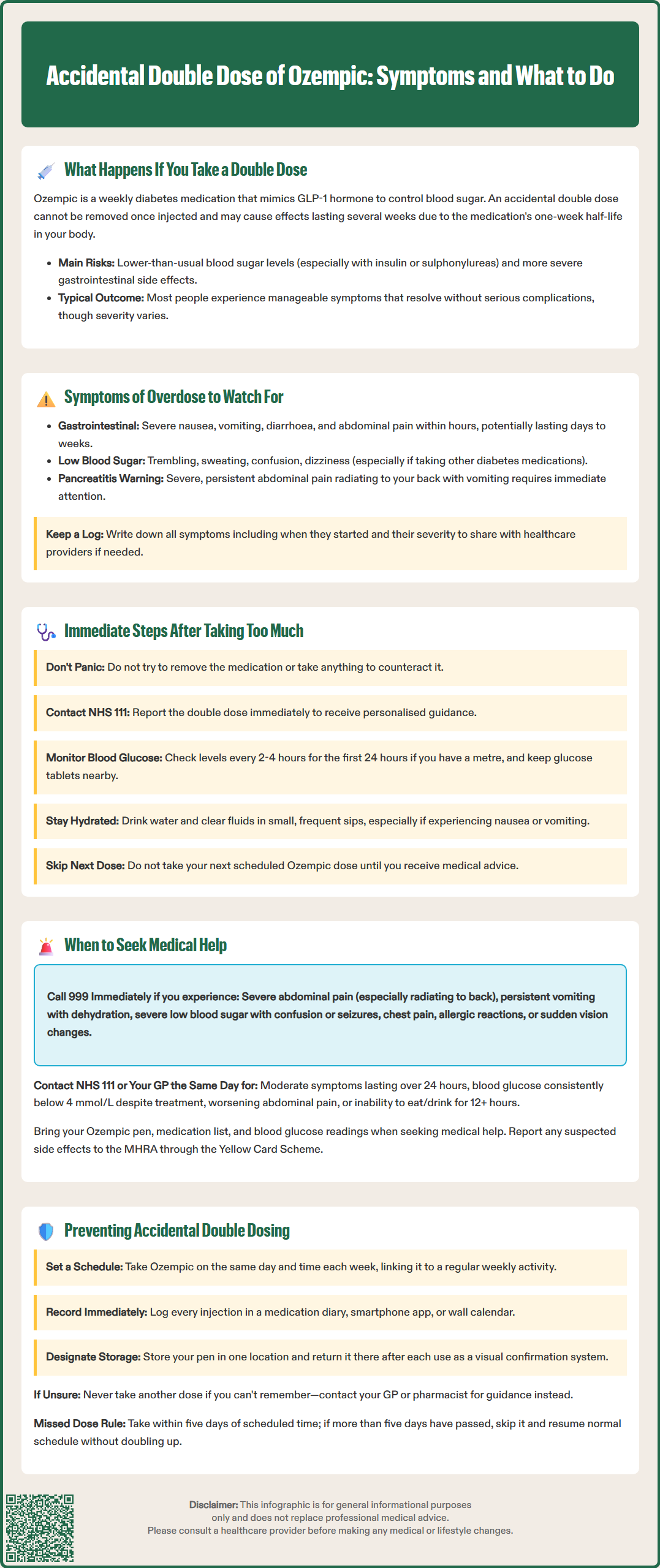
Following an accidental double dose of Ozempic, you should monitor yourself carefully for symptoms that may develop within hours and potentially persist for several days to weeks. The most common symptoms relate to the medication's mechanism of action and typically involve the gastrointestinal system and blood glucose regulation.
Gastrointestinal symptoms are the most frequently reported adverse effects and may include:
Nausea and vomiting – often severe and persistent, potentially leading to dehydration and, in some cases, acute kidney injury (particularly if you have existing kidney problems)
Abdominal pain or discomfort – ranging from mild cramping to significant pain
Diarrhoea – which may be frequent and watery
Loss of appetite – more pronounced than usual
Bloating and indigestion – due to delayed gastric emptying
Hypoglycaemia (low blood sugar) is another concern, particularly if you are taking other diabetes medications such as insulin or sulphonylureas. The risk is much lower if Ozempic is your only diabetes medication. Warning signs include:
Trembling or shakiness
Sweating and palpitations
Confusion or difficulty concentrating
Dizziness or light-headedness
Hunger and irritability
Pale skin and weakness
Additional symptoms may include headache, fatigue, increased heart rate, and general malaise. In rare cases, severe complications such as acute pancreatitis may occur, characterised by severe, persistent abdominal pain that may radiate to the back, often accompanied by vomiting.
The intensity and duration of symptoms vary considerably between individuals. Some patients may experience only mild discomfort, whilst others may have more pronounced reactions requiring medical intervention. Keep a written record of any symptoms you experience, including their onset time and severity, as this information will be valuable if you need to contact healthcare services.
If you realise you have accidentally administered a double dose of Ozempic, taking prompt and appropriate action can help minimise potential complications and ensure your safety. Remain calm—whilst the situation requires attention, panic is counterproductive.
Immediate actions to take:
1. Do not attempt to remove the medication. Once Ozempic has been injected subcutaneously, it cannot be extracted or neutralised. Do not take extra medication to 'counteract' the semaglutide, but continue your usual prescribed diabetes medicines (including insulin) unless advised otherwise by a healthcare professional.
2. Contact NHS 111 or your GP surgery for advice. Explain clearly what has happened, including your usual dose, the amount you have taken, when you administered it, and any symptoms you are experiencing. They will provide personalised guidance based on your circumstances.
3. Monitor your blood glucose levels if you have a glucose meter at home, particularly if you also take insulin or sulphonylureas. If you're at risk of hypoglycaemia, check your levels every 2–4 hours for the first 24 hours, and continue regular monitoring for several days. Keep a record of your readings.
4. Stay well hydrated. Drink plenty of water and clear fluids, particularly if you experience nausea, vomiting, or diarrhoea. Small, frequent sips may be better tolerated than large amounts at once. Be alert for signs of dehydration such as dark urine or reduced urination, especially if you have kidney problems.
5. Eat small, bland meals if you can tolerate food. This helps maintain blood glucose levels and may reduce nausea. Avoid fatty, spicy, or heavy foods that could exacerbate gastrointestinal symptoms.
6. Keep fast-acting carbohydrates readily available (such as glucose tablets, fruit juice, or sugary drinks) in case you develop hypoglycaemia. If you experience symptoms of low blood sugar, follow your usual hypoglycaemia management plan.
7. Avoid your next scheduled dose until you have received medical advice about when to resume your normal dosing schedule.
Whilst many cases of accidental double dosing can be managed at home with telephone guidance from healthcare professionals, certain symptoms warrant immediate medical attention. Understanding when to escalate your care is crucial for preventing serious complications.
Seek emergency medical help (call 999 or attend A&E) if you experience:
Severe, persistent abdominal pain, especially if it radiates to your back—this could indicate pancreatitis, a rare but serious complication
Persistent vomiting that prevents you from keeping down fluids, leading to signs of dehydration (dark urine, dizziness when standing, dry mouth, reduced urination)
Severe hypoglycaemia with confusion, loss of consciousness, seizures, or inability to treat yourself
Chest pain, severe palpitations, or difficulty breathing
Signs of an allergic reaction, including facial swelling, difficulty swallowing, or widespread rash
Severe weakness or inability to function normally
Sudden visual changes, particularly if you have pre-existing diabetic retinopathy
Contact NHS 111 or your GP urgently (same day) if you have:
Moderate to severe nausea and vomiting lasting more than 24 hours
Persistent diarrhoea with signs of dehydration
Blood glucose readings consistently below 4 mmol/L despite treatment
Abdominal pain that is worsening or not improving
Inability to eat or drink for more than 12 hours
Reduced urine output, especially if you have kidney disease
Any symptoms causing significant concern
Routine GP contact is appropriate if you have mild symptoms that are manageable but you need advice about resuming your normal dosing schedule or if you have questions about preventing future incidents.
When seeking medical help, bring your Ozempic pen, a list of all your medications, and your blood glucose readings if available. This information helps healthcare professionals assess your situation accurately and provide appropriate treatment. Remember that healthcare services would rather assess you and find no serious problem than have you delay seeking help when it is needed.
You can also report any suspected side effects to the MHRA through the Yellow Card Scheme at yellowcard.mhra.gov.uk or via the Yellow Card app.
Preventing accidental double dosing requires establishing reliable systems and habits around your medication administration. Most dosing errors are preventable with proper planning and attention to detail.
Practical strategies to prevent double dosing:
Establish a consistent routine. Administer your Ozempic injection on the same day each week, at approximately the same time. Many patients find it helpful to link their injection day to a specific weekly activity or event (e.g., "every Sunday morning before breakfast"). Consider writing your 'dose day' on the pen or carton.
Use a medication diary or tracking system. Record each injection immediately after administration, noting the date, time, and dose. Smartphone apps designed for medication tracking can send reminders and maintain an automatic log. Alternatively, mark injections on a wall calendar or use a paper diary kept with your medication.
Store your Ozempic pen in a designated location and return it there immediately after each use. Some patients use a small box or container that also holds their tracking diary, creating a visual system that confirms whether the weekly dose has been taken.
Set a weekly alarm or reminder on your phone or other device. When the alarm sounds, check your diary before administering the injection. If you are unsure whether you have already taken your dose, do not inject—contact your GP or pharmacist for advice.
Understand the pen mechanism. Familiarise yourself with how the Ozempic pen works, including the dose counter. After injection, the dose counter should return to zero, providing visual confirmation that the dose has been delivered.
Involve family members or carers if appropriate. They can help remind you about your injection day or verify whether you have already administered your dose.
If you miss a dose, follow the official UK guidance: if fewer than five days have passed since your missed dose, take it as soon as you remember. If more than five days have passed, skip the missed dose and take the next dose on your usual day. Do not take a double dose to make up for a missed dose.
Regular medication reviews with your GP or practice nurse provide opportunities to discuss any difficulties with your injection routine and receive additional support or training if needed.
Whilst an accidental double dose of Ozempic is not typically life-threatening, it can cause serious complications such as severe hypoglycaemia, dehydration from persistent vomiting, or rarely acute pancreatitis. Most patients experience manageable symptoms, but medical advice should always be sought promptly.
Due to Ozempic's long half-life of approximately one week, effects from a double dose may persist for several days to weeks. Symptoms typically peak within the first 24–72 hours but can continue as the medication gradually clears from your system.
Do not take your next scheduled dose until you have received medical advice from NHS 111, your GP, or pharmacist. They will provide personalised guidance on when to safely resume your normal dosing schedule based on your individual circumstances.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.