
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed exclusively for subcutaneous injection into fatty tissue beneath the skin. Accidental intravenous administration is extremely rare when using the pre-filled pen device correctly, but if it occurs, the medication would enter the bloodstream immediately rather than being absorbed gradually. This could theoretically increase the risk of adverse effects. The Medicines and Healthcare products Regulatory Agency (MHRA) and Summary of Product Characteristics explicitly prohibit intravenous use. If you suspect accidental intravenous injection—indicated by blood at the injection site or unusual immediate symptoms—seek prompt medical advice from your GP, NHS 111, or attend A&E if symptoms are severe.
Quick Answer: Accidental intravenous injection of Ozempic is extremely unlikely with correct technique but would cause immediate bloodstream entry rather than gradual absorption, potentially increasing adverse effect risk.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed for subcutaneous administration only. It is specifically formulated and approved for injection into the fatty tissue beneath the skin, not for intravenous use. The pharmacokinetic profile of semaglutide has been established based on subcutaneous delivery, which allows for gradual absorption and sustained therapeutic effect over several days, with a long half-life of approximately one week.
If Ozempic were accidentally injected directly into a vein, the medication would enter the bloodstream immediately rather than being absorbed slowly from subcutaneous tissue. This could theoretically result in a rapid spike in serum semaglutide concentration, potentially increasing the risk of adverse effects. However, published human data on intravenous semaglutide administration are limited. The Medicines and Healthcare products Regulatory Agency (MHRA) and the Summary of Product Characteristics (SmPC) for Ozempic explicitly prohibit intravenous or intramuscular administration.
It is important to note that accidental intravenous injection is very unlikely when Ozempic is administered correctly using the pre-filled pen device into appropriate subcutaneous sites (abdomen, thigh, or upper arm). The short needle length (typically 4 mm) and recommended injection sites are designed to minimise this risk. Nonetheless, if there is concern that the medication may have been injected into a vein—such as if blood is visible at the needle tip or injection site, or unusual immediate symptoms occurred—medical advice should be sought promptly. If intravenous administration is suspected, this should be managed as a potential overdose with appropriate supportive care and monitoring.
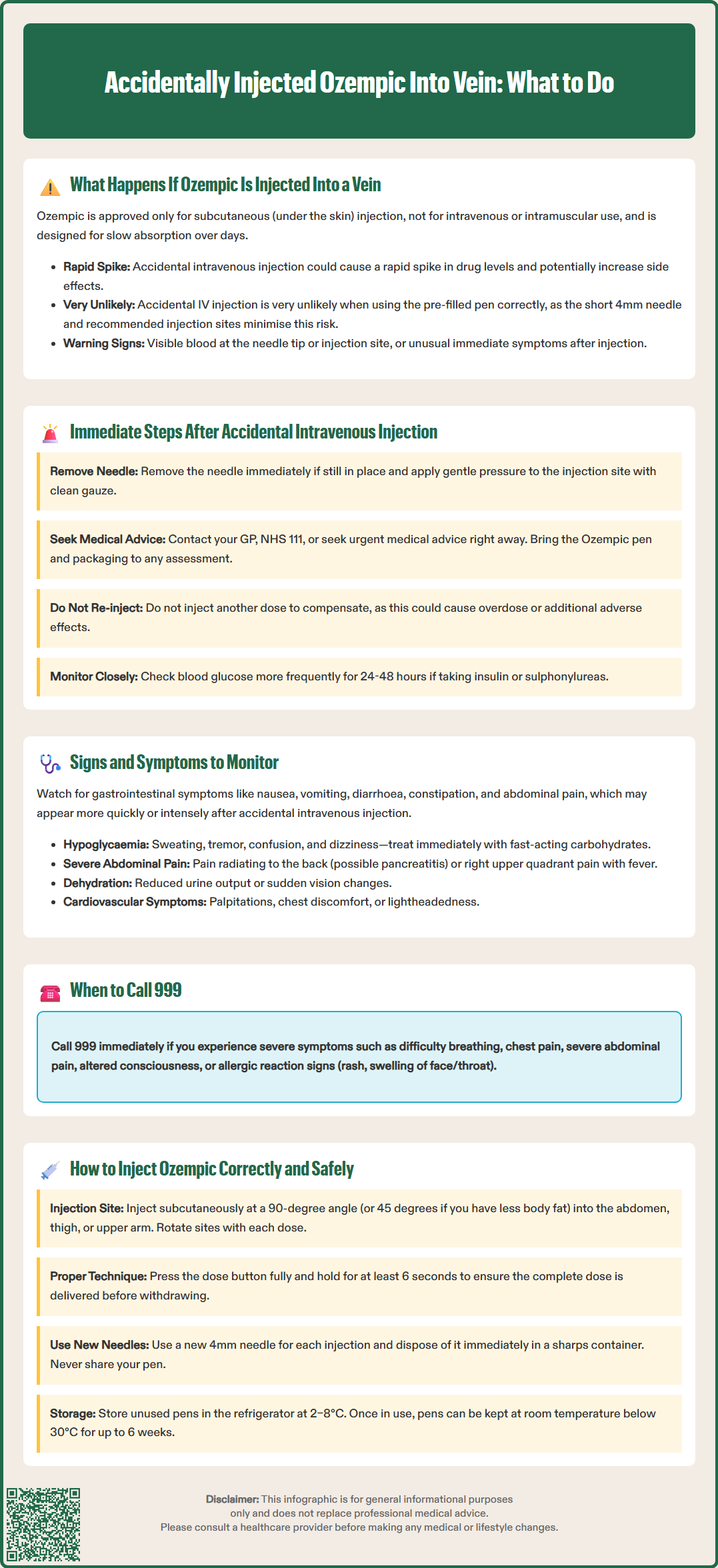
If you suspect that Ozempic has been accidentally injected into a vein, it is essential to remain calm and take prompt action. The first step is to remove the needle immediately if it is still in place and apply gentle pressure to the injection site with a clean gauze or tissue to minimise bleeding or bruising.
Contact your GP, NHS 111, or seek urgent medical advice as soon as possible. Explain clearly what has happened, including:
The dose of Ozempic administered
The injection site and any unusual observations (e.g., blood visible at the needle tip or injection site, immediate pain, or rapid onset of symptoms)
Your current symptoms, if any
Your medical history and any other medications you are taking
Take the Ozempic pen and packaging (with batch number) with you to any medical assessment. Healthcare professionals may advise you to attend an urgent care centre, A&E department, or arrange a same-day assessment depending on the clinical context and your symptoms. Do not attempt to administer another dose to compensate, as this could lead to overdose or compounded adverse effects.
It is also advisable to monitor yourself closely for any unusual symptoms over the following days, given semaglutide's long half-life. If you are also taking insulin or sulphonylureas, more frequent blood glucose monitoring is recommended for 24-48 hours, and you should seek advice about potential dose adjustments of these medications. Maintain adequate hydration, especially if gastrointestinal symptoms occur, and seek immediate care if you are unable to keep fluids down.
If you experience severe symptoms such as difficulty breathing, chest pain, severe abdominal pain, or altered consciousness, call 999 immediately.
Any suspected adverse reactions can be reported via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Following a suspected accidental intravenous injection of Ozempic, it is important to be vigilant for symptoms that may indicate an adverse reaction or exaggerated pharmacological effect. While the specific effects of intravenous semaglutide administration in humans are not well documented, awareness of the known side effects of Ozempic can guide monitoring.
Gastrointestinal symptoms are the most common adverse effects associated with Ozempic and include:
Nausea and vomiting
Diarrhoea or constipation
Abdominal pain or discomfort
Loss of appetite
These symptoms may theoretically be more pronounced or occur more rapidly if the medication enters the bloodstream directly. Hypoglycaemia (low blood sugar) is another important consideration, particularly in patients using Ozempic alongside insulin or sulphonylureas (hypoglycaemia is uncommon with semaglutide monotherapy). Warning signs include sweating, tremor, palpitations, confusion, dizziness, and hunger. If you experience symptoms of hypoglycaemia, check your blood glucose if possible and consume a fast-acting carbohydrate (e.g., glucose tablets, sugary drink) as per your diabetes management plan.
Important red flags that require immediate medical attention include:
Severe, persistent abdominal pain (possibly radiating to the back) with or without vomiting, which may suggest acute pancreatitis
Right upper quadrant pain, fever, or yellowing of the skin/eyes, which could indicate gallbladder disease
Reduced urine output or marked dehydration from persistent gastrointestinal symptoms
Sudden changes in vision, particularly in those with diabetic retinopathy
Cardiovascular symptoms such as palpitations, chest discomfort, or lightheadedness should prompt immediate medical review. Although rare, allergic reactions (including anaphylaxis) can occur with semaglutide; watch for rash, itching, swelling (especially of the face or throat), or difficulty breathing.
Additionally, monitor the injection site for signs of local reaction, bruising, or swelling. If symptoms are severe, worsening, or persist beyond a couple of days, contact your healthcare provider or NHS 111 for further guidance. Keeping a symptom diary can be helpful for clinical assessment.
Correct injection technique is essential to ensure the safe and effective use of Ozempic and to minimise the risk of complications, including accidental intravenous administration. Ozempic is supplied in a pre-filled, single-patient-use pen designed for subcutaneous injection. The following steps, based on the manufacturer's Instructions for Use and the SmPC, outline best practice:
Preparation:
Wash your hands thoroughly with soap and water
Check the Ozempic pen label to confirm the correct medication and dose
Inspect the solution—it should be clear and colourless; do not use if cloudy or discoloured
Attach a new needle to the pen for each injection
Perform a flow check before the first use of a new pen (not required before every dose)
Injection technique:
Select an appropriate injection site: abdomen (avoiding the area around the navel), front of the thigh, or upper arm (may require assistance)
Rotate injection sites with each dose to reduce local skin reactions
Clean the skin with an alcohol wipe if recommended by your healthcare team, and allow to dry
Pinch the skin gently to lift the subcutaneous tissue
Insert the needle at a 90-degree angle (or 45 degrees if you have less subcutaneous fat)
Press the dose button fully and hold for at least 6 seconds to ensure complete delivery
Withdraw the needle and dispose of it safely in a sharps container
Important safety points:
A 4 mm pen needle is generally recommended for adults unless advised otherwise by a healthcare professional
Aspiration (pulling back on the plunger) is not possible with the Ozempic pen device and is not necessary for subcutaneous injections
Never share your pen with others, even if the needle is changed
Store unused pens in the refrigerator (2–8°C); do not freeze
Once in use, pens may be kept at room temperature (below 30°C) for up to 6 weeks
Keep the pen cap on when not in use to protect from light
If you are uncertain about your injection technique, ask your GP, practice nurse, or diabetes specialist nurse for a demonstration and supervised practice. Patient education is a cornerstone of safe self-administration.
No, Ozempic is licensed only for subcutaneous injection and must not be administered intravenously or intramuscularly. The MHRA and Summary of Product Characteristics explicitly prohibit intravenous use.
Apply gentle pressure with clean gauze to stop bleeding, then contact your GP or NHS 111 immediately to report the incident. If you develop severe symptoms such as difficulty breathing or chest pain, call 999.
Use the correct injection technique: inject at a 90-degree angle into subcutaneous tissue (abdomen, thigh, or upper arm), rotate sites with each dose, and use the 4 mm pen needle as recommended. Ask your practice nurse for a demonstration if unsure.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.