Are weight loss injections painful? This is one of the most common concerns for patients considering glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) or liraglutide (Saxenda) for weight management. Most patients report minimal discomfort, typically describing the sensation as a brief pinch rather than significant pain. These medications are administered subcutaneously using very fine needles (30–32 gauge), similar to insulin devices. Pain perception varies between individuals and depends on injection technique, site selection, and personal pain threshold. Understanding what to expect and learning proper administration techniques can significantly reduce anxiety and improve treatment adherence. This article explores the factors influencing injection discomfort and provides practical guidance for UK patients.
Quick Answer: Weight loss injections such as semaglutide and liraglutide typically cause minimal pain, with most patients describing a brief pinch sensation due to very fine needles.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWeight loss injections, particularly glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have become increasingly prescribed for weight management in the UK. These medications are administered subcutaneously, meaning they are injected into the fatty tissue just beneath the skin rather than into muscle or veins. For many patients considering these treatments, concerns about pain represent a significant barrier to starting therapy.
Pain perception during injections is highly individual and influenced by multiple factors including needle gauge, injection technique, anatomical site, and personal pain threshold. Most patients report that weight loss injections cause minimal discomfort, often describing the sensation as a brief pinch or pressure rather than significant pain. The needles used for these medications are typically very fine (30-32 gauge), similar to those used for insulin administration, which helps reduce tissue trauma and associated discomfort.
It is important to distinguish between the momentary sensation of needle insertion and other forms of discomfort that may occur with weight loss injections. Some patients experience injection site reactions such as redness, swelling, or tenderness that develops after the injection itself. Additionally, the medication volume and formulation can influence comfort levels. Understanding what to expect can significantly reduce anxiety and improve treatment adherence, as fear of pain often proves more distressing than the actual injection experience. Healthcare professionals should provide training and demonstration injections following the manufacturer's instructions before patients begin self-administration, as recommended in NICE guidance (NG215) on obesity management.
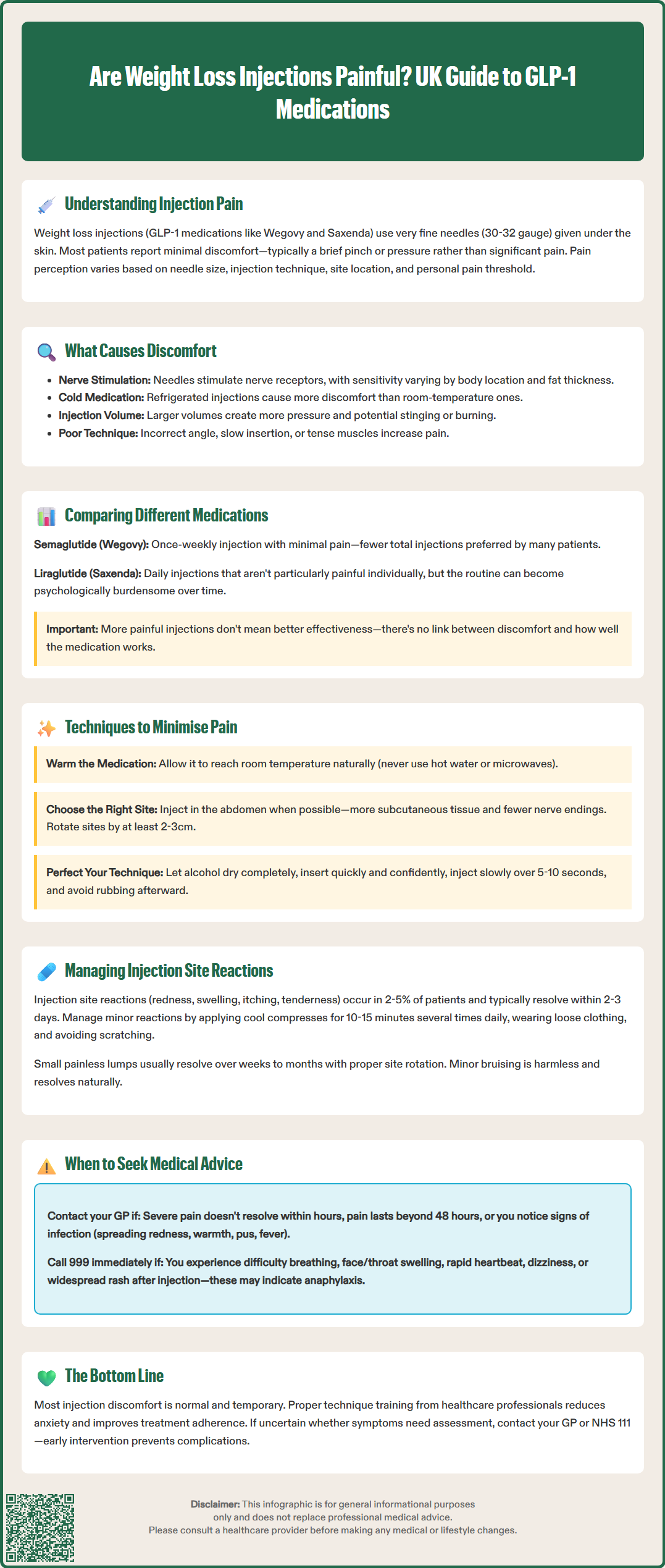
Several physiological and technical factors contribute to discomfort experienced during weight loss injections. The primary cause of pain is mechanical stimulation of nociceptors (pain receptors) in the skin and subcutaneous tissue as the needle penetrates these layers. The density of nerve endings varies across different body sites, which explains why some injection locations are more sensitive than others. Areas with thinner subcutaneous fat layers or higher concentrations of nerve fibres typically produce more noticeable sensations.
The medication formulation itself can contribute to post-injection discomfort. GLP-1 receptor agonists are typically formulated in slightly acidic or neutral pH solutions, and the introduction of this fluid into subcutaneous tissue can cause temporary stinging or burning sensations. The volume of medication administered also matters—larger volumes may cause more pressure-related discomfort than smaller volumes. Cold medication injected directly from refrigerated storage can intensify discomfort, as the temperature differential between the solution and body tissue stimulates additional sensory receptors.
Injection technique significantly influences pain levels. Rapid needle insertion, incorrect injection angles (typically 90 degrees for subcutaneous injections, though this may be 45 degrees in very lean patients), or injecting into areas with insufficient subcutaneous fat can all increase discomfort. Tense muscles during injection create resistance that makes needle penetration more difficult and painful. Furthermore, repeated injections in the same site can lead to lipohypertrophy (thickening of fatty tissue) or scarring, which may alter sensation and increase discomfort with subsequent injections. Proper site rotation, as recommended by NICE guidance, helps prevent these complications.
Different weight loss injection medications vary in their associated pain profiles, though all are generally well-tolerated. Semaglutide (Wegovy), administered once weekly, uses a pre-filled pen device with a fine needle and relatively small injection volumes in the initial titration phases. Most patients report minimal pain with semaglutide injections, rating discomfort as 2-3 on a 10-point scale. The once-weekly dosing schedule also means fewer injection experiences overall, which many patients prefer.
Liraglutide (Saxenda) requires daily subcutaneous injections, which means more frequent needle insertions. However, the daily injection volume is smaller than weekly alternatives, and the pen device uses similarly fine needles. Patient surveys suggest that whilst the injection itself is not particularly painful, the daily routine can become psychologically burdensome for some individuals. The cumulative experience of daily injections may amplify awareness of minor discomfort that might otherwise be dismissed with less frequent dosing schedules.
Tirzepatide (Mounjaro), a dual GIP/GLP-1 receptor agonist currently authorised in the UK for type 2 diabetes treatment but not yet for weight management, demonstrates a pain profile comparable to other GLP-1 medications. The medication is administered weekly using an auto-injector device that conceals the needle, which can reduce anticipatory anxiety in needle-phobic patients. According to clinical trial data and SmPC information, injection site reactions occur in approximately 2-5% of patients across these medications, with most reactions being mild and self-limiting.
There is no official link between medication efficacy and injection pain—a more painful injection does not indicate better drug delivery or effectiveness. The MHRA-approved devices for these medications are specifically designed to optimise patient comfort whilst ensuring reliable subcutaneous delivery. Patients who find one formulation particularly uncomfortable should discuss alternative options with their prescriber, as individual responses vary considerably.
Proper injection technique is fundamental to minimising discomfort and can be learned through healthcare professional demonstration and practice. Before injecting, allow the medication to reach room temperature by removing it from the refrigerator approximately 30 minutes beforehand (as specified in the product SmPC), as cold solutions cause more stinging. Never attempt to warm medication artificially using hot water or microwaves, as this can degrade the active pharmaceutical ingredients.
Site selection and rotation are crucial for comfort. The recommended injection sites for subcutaneous weight loss medications include the abdomen (avoiding a 5cm radius around the navel), front and outer thighs, and upper outer arms. The abdomen typically offers the most comfortable injection experience due to abundant subcutaneous tissue and relatively fewer nerve endings in this area. Rotate injection sites systematically, maintaining at least 2-3cm distance from previous injection locations to prevent tissue changes that increase sensitivity.
Before injection, clean the site with an alcohol wipe and allow it to dry completely—injecting through wet alcohol causes stinging. Pinch the skin gently to create a firm surface and ensure subcutaneous rather than intramuscular injection. Insert the needle swiftly and confidently in one smooth motion rather than slowly pushing it through the skin, as hesitant insertion prolongs discomfort. Keep muscles relaxed throughout the procedure; tension increases resistance and pain.
After inserting the needle, inject the medication slowly and steadily according to device instructions (typically over 5-10 seconds). Rapid injection increases pressure-related discomfort. Once complete, withdraw the needle at the same angle it entered, then apply gentle pressure with a clean cotton wool ball if needed. Avoid rubbing the injection site, as this can increase irritation and potentially affect medication absorption. Always dispose of used needles in an approved sharps container following local NHS guidelines. Some patients find that applying a cold compress (not ice directly on skin) for a few minutes after injection helps reduce any residual stinging or swelling.
Whilst the injection itself typically causes minimal pain, injection site reactions are common side effects reported in clinical trials of GLP-1 receptor agonists. These reactions usually manifest as mild redness (erythema), swelling, itching, or tenderness at the injection site. Such reactions typically appear within hours of injection and resolve spontaneously within 2-3 days without specific treatment. They occur more frequently during the initial weeks of therapy and often diminish as the body adapts to the medication.
To manage minor injection site reactions, avoid touching or scratching the affected area, as this can introduce bacteria and increase inflammation. If itching is bothersome, consult a pharmacist about suitable over-the-counter antihistamines, as these may provide relief but could interact with other medications. Cool compresses applied for 10-15 minutes several times daily can reduce swelling and provide symptomatic relief. Loose-fitting clothing prevents friction against sensitive injection sites.
Some patients develop small, painless lumps (nodules) at injection sites, particularly with repeated use of the same location. These represent localised lipohypertrophy or inflammatory responses and usually resolve over weeks to months with proper site rotation. However, persistent or enlarging lumps warrant medical assessment to exclude other causes such as infection or, rarely, allergic reactions.
Bruising occasionally occurs if the needle punctures a small blood vessel during injection. Whilst alarming in appearance, minor bruising is harmless and resolves naturally. Patients taking anticoagulant medications or with clotting disorders may bruise more readily. Applying firm pressure immediately after injection can minimise bruising risk. If bruising is extensive, painful, or accompanied by other symptoms, contact your healthcare provider. The NHS advises that most injection site reactions require only observation and basic comfort measures, but persistent or worsening symptoms should prompt professional review. Suspected adverse reactions should be reported via the MHRA Yellow Card Scheme, which helps monitor medication safety.
Most injection-related discomfort is normal and self-limiting, but certain symptoms warrant prompt medical attention. Contact your GP or prescribing clinician if you experience severe pain during or after injection that does not resolve within a few hours, as this may indicate incorrect injection technique or, rarely, inadvertent intramuscular administration. Persistent pain lasting beyond 48 hours or pain that progressively worsens requires professional assessment.
Signs of infection at injection sites necessitate urgent medical review. Seek advice if you develop increasing redness spreading beyond the immediate injection site, warmth, swelling, pus or discharge, red streaks extending from the injection site, or fever. These symptoms may indicate cellulitis or abscess formation requiring antibiotic therapy. Immunocompromised patients or those with diabetes should be particularly vigilant, as they face higher infection risks.
Allergic reactions to weight loss injections are uncommon but potentially serious. Immediate medical attention (call 999) is required if you experience symptoms of anaphylaxis including difficulty breathing, swelling of face or throat, rapid heartbeat, dizziness, or widespread rash developing shortly after injection. Less severe allergic reactions such as localised hives, persistent itching, or recurring injection site reactions should be discussed with your prescriber, who may recommend antihistamine prophylaxis or alternative treatments.
Unusual symptoms such as severe abdominal pain, persistent nausea and vomiting, or visual changes should prompt immediate medical contact, as these may represent rare but serious adverse effects unrelated to injection technique. NICE guidance emphasises the importance of patient education regarding both expected and concerning symptoms. Your healthcare team should provide clear written information about when to seek help and emergency contact details. Never hesitate to contact your GP surgery or NHS 111 if you are uncertain whether symptoms require professional assessment—early intervention prevents complications and provides reassurance.
This information is intended for educational purposes only and does not replace professional medical advice. Always consult your healthcare provider for guidance specific to your individual circumstances.
Most patients report minimal pain, typically describing the sensation as a brief pinch or pressure. The fine needles (30–32 gauge) used for these subcutaneous injections cause less discomfort than many anticipate, and proper technique further reduces any sensation.
Allow medication to reach room temperature before injecting, rotate injection sites systematically, ensure the alcohol wipe has dried completely, relax your muscles, and insert the needle swiftly in one smooth motion. Injecting slowly and steadily also reduces pressure-related discomfort.
Seek medical advice if you experience severe pain lasting beyond a few hours, persistent pain beyond 48 hours, signs of infection (spreading redness, warmth, fever, pus), or symptoms of allergic reactions such as difficulty breathing or facial swelling.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.