Concerns about medications and cognitive health are understandable, particularly for those managing long-term conditions such as type 2 diabetes. If you're taking or considering Ozempic (semaglutide), you may wonder whether it affects dementia risk. Current evidence provides reassurance: there is no established link between Ozempic and increased dementia risk. In fact, emerging research suggests GLP-1 receptor agonists like Ozempic may have potential neuroprotective properties. This article examines the evidence, explores the relationship between diabetes and cognitive health, and explains when to seek medical advice.
Quick Answer: No, Ozempic does not cause dementia; current evidence shows no increased dementia risk and suggests potential neuroprotective effects.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a prescription medication licensed in the UK for the treatment of type 2 diabetes mellitus. It belongs to a class of drugs called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone in the body.
The mechanism of action involves several key processes:
Stimulating insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning insulin is only released when blood sugar levels are elevated
Suppressing glucagon release, which reduces glucose production by the liver
Slowing gastric emptying, helping patients feel fuller for longer and reducing post-meal blood sugar spikes
Acting on appetite centres in the brain, particularly in the hypothalamus, to reduce hunger and food intake
Ozempic is administered as a once-weekly subcutaneous injection and is typically prescribed when diet, exercise, and oral medications such as metformin have not achieved adequate glycaemic control. The Medicines and Healthcare products Regulatory Agency (MHRA) approved semaglutide for type 2 diabetes in 2018, and NICE guidelines (NG28) support its use in specific clinical scenarios.
Beyond glucose control, clinical trials (such as SUSTAIN-6) have demonstrated that Ozempic can lead to significant weight loss and showed cardiovascular benefits, including reduced risk of major adverse cardiovascular events in people with established cardiovascular disease. It's important to note that in the UK, Ozempic is licensed specifically for glycaemic control in type 2 diabetes, not for weight management (for which the higher-dose semaglutide product Wegovy is licensed) or cardiovascular risk reduction.
Hypoglycaemia (low blood sugar) is uncommon with Ozempic when used alone, but the risk increases when combined with sulfonylureas or insulin.
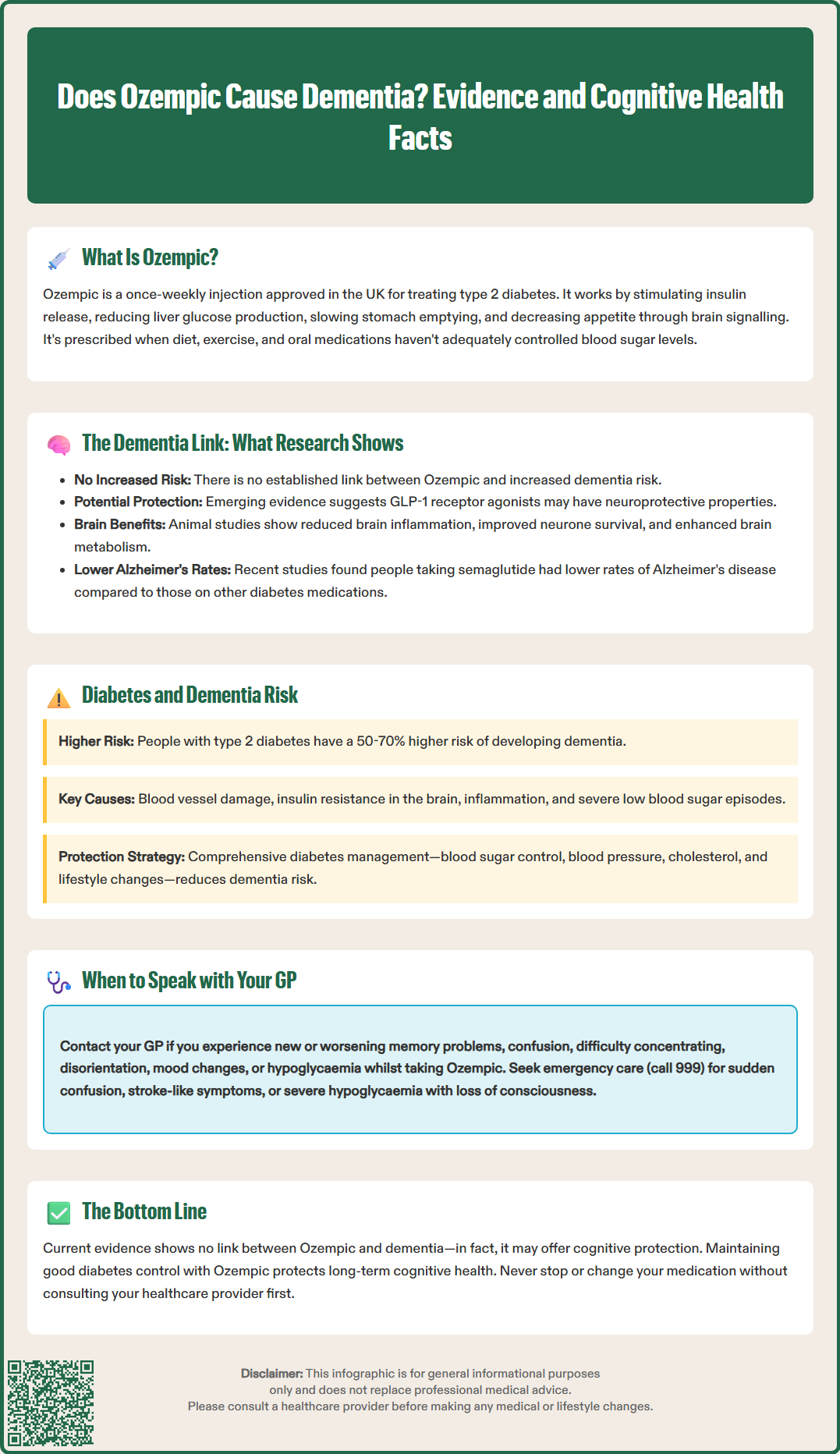
Research into the neurological effects of GLP-1 receptor agonists has yielded intriguing but preliminary findings. Importantly, there is no official link established between Ozempic and an increased risk of dementia. In fact, emerging evidence suggests these medications may have potential neuroprotective properties, though this is not a licensed indication.
GLP-1 receptors are present throughout the central nervous system, including regions involved in memory and cognition such as the hippocampus. Preclinical studies in animal models have suggested that GLP-1 receptor activation may have several effects on the brain, though these findings require confirmation in human studies:
Potential reduction in neuroinflammation
Possible promotion of neuronal survival
Effects on synaptic plasticity
Potential improvements in cerebral metabolism
Several observational studies in humans have examined cognitive outcomes in people with type 2 diabetes taking GLP-1 receptor agonists. A 2020 systematic review published in Diabetes, Obesity and Metabolism (Gejl et al.) found that these medications were associated with either neutral or potentially beneficial effects on cognitive function, with no evidence of increased dementia risk.
More recently, researchers have investigated whether semaglutide might affect the risk of Alzheimer's disease. A retrospective cohort study suggested that people with type 2 diabetes taking semaglutide had a lower incidence of Alzheimer's disease compared to those on other diabetes medications, though these findings require confirmation through prospective randomised controlled trials specifically designed to assess cognitive outcomes.
It is crucial to note that correlation does not equal causation, and much of the current evidence comes from observational data rather than definitive clinical trials. Semaglutide is not licensed for the prevention or treatment of dementia or cognitive impairment.
People with type 2 diabetes have an approximately 50–70% increased risk of developing dementia compared to those without diabetes, according to research cited by Diabetes UK and the Alzheimer's Society. Understanding this relationship is essential when considering any potential cognitive effects of diabetes medications.
Key mechanisms linking diabetes to dementia include:
Chronic hyperglycaemia (persistently elevated blood sugar), which can damage blood vessels in the brain and contribute to vascular dementia
Insulin resistance in the brain, which may impair neuronal glucose metabolism and contribute to Alzheimer's pathology
Microvascular complications, including damage to small blood vessels that supply the brain
Increased inflammation and oxidative stress associated with poor metabolic control
Hypoglycaemic episodes (particularly severe ones), which may cause acute neuronal injury
Additional risk factors that commonly coexist with type 2 diabetes include:
Hypertension and cardiovascular disease
Obesity and physical inactivity
Dyslipidaemia (abnormal cholesterol levels)
Depression and social isolation
Smoking and excessive alcohol consumption
NICE guidance (NG28) emphasises the importance of comprehensive diabetes management to reduce long-term complications, including potential cognitive decline. This includes maintaining good glycaemic control with individualised HbA1c targets (typically around 48 mmol/mol if not at risk of hypoglycaemia, or around 53 mmol/mol when on medications that can cause hypoglycaemia), managing cardiovascular risk factors (blood pressure, lipids), encouraging smoking cessation, and promoting physical activity.
The relationship between diabetes medications and dementia risk is complex. Some older studies suggested that certain medications might influence cognitive outcomes, but optimising blood sugar control itself appears to be protective against dementia. Therefore, effective diabetes treatment—potentially including medications like Ozempic—may actually reduce rather than increase dementia risk by addressing the underlying metabolic dysfunction.
If you are taking Ozempic or considering it as a treatment option, it is important to maintain open communication with your healthcare team about any concerns, including those related to cognitive health. Based on current evidence, there is no reason to discontinue Ozempic due to dementia concerns, but certain situations warrant medical review.
You should contact your GP or diabetes specialist nurse if you experience:
Memory problems or confusion that is new, worsening, or interfering with daily activities
Difficulty concentrating or making decisions that represents a change from your usual cognitive function
Disorientation regarding time, place, or familiar people
Mood changes, including depression, anxiety, or personality alterations
Hypoglycaemia, particularly if you are also taking sulfonylureas or insulin with Ozempic
Seek urgent medical attention (call 999) if you experience:
Sudden confusion or disorientation (delirium)
Stroke-like symptoms (face drooping, arm weakness, speech difficulties - remember FAST)
Severe hypoglycaemia with loss of consciousness
For less urgent concerns, NHS 111 can provide advice.
It is worth noting that common side effects of Ozempic according to the SmPC include nausea, diarrhoea, vomiting, and decreased appetite. These gastrointestinal symptoms can sometimes affect concentration and mental clarity, particularly when starting treatment or increasing the dose. These effects are typically temporary and resolve as your body adjusts to the medication.
During your consultation, your GP may:
Review your overall diabetes control and medication regimen
Assess for other potential causes of cognitive symptoms, including vitamin B12 deficiency (which can occur with long-term metformin use), thyroid dysfunction, or depression
Arrange cognitive screening if appropriate
Discuss the balance of benefits and risks for your individual circumstances
Refer you to specialist services if significant cognitive impairment is suspected, such as a memory clinic or older adults mental health services
Remember that maintaining good diabetes control is one of the most important steps you can take to protect your long-term cognitive health. If Ozempic is helping you achieve your glycaemic targets and is well-tolerated, the benefits likely outweigh any theoretical risks. Never stop or alter your prescribed medication without consulting your healthcare professional first.
If you suspect any adverse effects from your medication, you can report them through the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
No, there is no established link between Ozempic and increased dementia risk. Emerging evidence suggests GLP-1 receptor agonists like Ozempic may actually have potential neuroprotective properties, though this requires further research through prospective clinical trials.
People with type 2 diabetes have approximately 50–70% increased dementia risk due to chronic hyperglycaemia damaging brain blood vessels, insulin resistance affecting neuronal metabolism, microvascular complications, increased inflammation, and potential hypoglycaemic episodes causing neuronal injury.
No, you should not stop Ozempic without consulting your healthcare professional. Current evidence shows no dementia risk, and maintaining good diabetes control with Ozempic may actually protect cognitive health by addressing underlying metabolic dysfunction.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.