
Glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide and liraglutide are widely prescribed in the UK for type 2 diabetes and weight management. Whilst highly effective, these medications can cause gastrointestinal side effects including nausea, vomiting, and diarrhoea, potentially leading to fluid and electrolyte losses. Understanding when and how to use electrolyte powders safely during GLP-1 treatment is important for maintaining wellbeing. This article examines the evidence for electrolyte supplementation, identifies key minerals to consider, and provides guidance on selecting appropriate products whilst highlighting when medical advice is essential.
Quick Answer: The best electrolyte powder for GLP-1 users contains balanced sodium, potassium, magnesium, and chloride without excessive sugar, though supplementation is only needed for those experiencing significant gastrointestinal losses or inadequate intake.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists, including semaglutide (Ozempic, Wegovy) and liraglutide (Saxenda, Victoza), are increasingly prescribed for type 2 diabetes management and weight loss in the UK. These medications work by mimicking the natural GLP-1 hormone, which enhances insulin secretion, suppresses glucagon release, slows gastric emptying, and reduces appetite. Whilst these mechanisms contribute to improved glycaemic control and weight reduction, they can also affect fluid and electrolyte balance.
The most common adverse effects of GLP-1 medications are gastrointestinal in nature, including nausea, vomiting, and diarrhoea. These symptoms are particularly prevalent during the initial titration phase and can lead to significant fluid losses. When vomiting or diarrhoea occurs, the body loses not only water but also essential electrolytes such as sodium, potassium, magnesium, and chloride. In severe cases, this can lead to dehydration and acute kidney injury, particularly in vulnerable patients.
Additionally, the appetite suppression and early satiety caused by GLP-1 agonists may result in reduced food and fluid intake, further compromising electrolyte status. It's important to note that not all patients will require electrolyte supplementation – this is primarily indicated for those experiencing significant gastrointestinal losses or inadequate intake, rather than as routine for all GLP-1 users.
Patients should be aware that severe, persistent abdominal pain with vomiting could indicate pancreatitis, a rare but serious adverse effect of GLP-1 medications that requires immediate medical attention. Similarly, symptoms of gallbladder disease can occur with weight loss and may require urgent assessment.
The decision to use electrolyte powders should be individualised and, ideally, discussed with a healthcare professional, particularly for those with pre-existing kidney conditions, heart failure, or those taking medications that affect fluid balance.
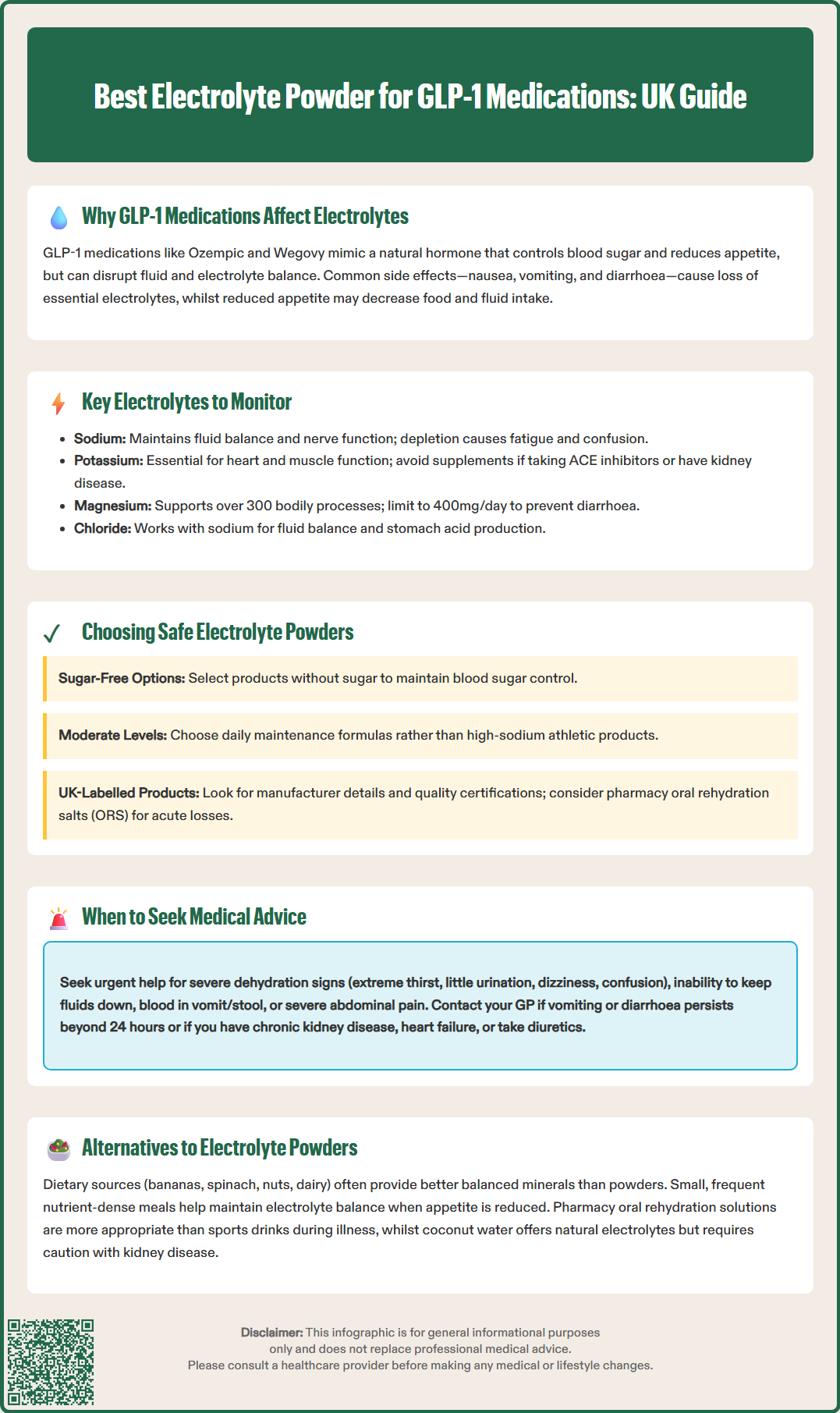
When considering electrolyte supplementation during GLP-1 treatment, it is essential to understand which minerals are most commonly depleted and their physiological roles. Sodium is the primary extracellular electrolyte, crucial for maintaining fluid balance, nerve function, and muscle contraction. Losses through vomiting or diarrhoea can lead to hyponatraemia, causing fatigue, confusion, and in severe cases, seizures.
Potassium is vital for cardiac function, muscle contraction, and nerve transmission. Gastrointestinal losses can result in hypokalaemia, which may manifest as muscle weakness, cramps, cardiac arrhythmias, and constipation. Importantly, patients taking medications that increase potassium levels, such as ACE inhibitors, angiotensin receptor blockers (ARBs), or potassium-sparing diuretics, should avoid potassium supplements unless specifically advised by their healthcare provider. This is particularly crucial for those with chronic kidney disease, as they have reduced ability to excrete excess potassium.
Magnesium supports over 300 enzymatic reactions, including energy production, protein synthesis, and muscle and nerve function. Deficiency can cause muscle cramps, fatigue, and cardiac irregularities. While magnesium may influence insulin sensitivity, supplementation should be based on deficiency rather than for diabetes management. Note that supplemental magnesium has an upper safe limit (typically 400mg/day for adults) and higher doses can cause diarrhoea.
Chloride works closely with sodium to maintain fluid balance and is a component of stomach acid. Losses through vomiting can disrupt acid-base balance. Calcium is important for bone health, muscle function, and nerve signalling, though it is less commonly depleted through gastrointestinal losses.
A balanced electrolyte product should contain appropriate amounts of these minerals based on individual needs. However, excessive supplementation can be harmful. For instance, too much potassium can cause hyperkalaemia, particularly in patients with kidney disease. Therefore, patients should be aware of their total daily intake from all sources, including food and other supplements, and follow product labelling for appropriate use.
Selecting an appropriate electrolyte product requires careful consideration of several factors, particularly for individuals taking GLP-1 medications. Sugar content is a primary concern, especially for patients using these medications for diabetes management. Many commercial electrolyte drinks and powders contain significant amounts of sugar, which can counteract glycaemic control efforts. Look for products that are sugar-free or use non-nutritive sweeteners, though be aware that some artificial sweeteners and sugar alcohols (polyols like sorbitol or xylitol) may exacerbate gastrointestinal symptoms in sensitive individuals.
Electrolyte composition and concentration should be appropriate for maintenance rather than extreme athletic performance. Products designed for endurance athletes often contain very high sodium levels that may not be suitable for everyday use, particularly for individuals with hypertension or cardiovascular conditions. For acute gastrointestinal losses, medically formulated oral rehydration salts (ORS) available from pharmacies are more appropriate than sports drinks.
Additives and excipients warrant attention. Some products contain artificial colours, flavours, or preservatives that may trigger sensitivities or worsen gastrointestinal symptoms. Individuals experiencing nausea from GLP-1 medications may prefer unflavoured or naturally flavoured options. Additionally, check for potential allergens if you have known sensitivities.
Regulatory status is important in the UK context. Most electrolyte powders are classified as food supplements, while some oral rehydration products are licensed as medicines or medical devices. Food supplements are not subject to the same rigorous testing as pharmaceuticals. Look for UK-labelled products with manufacturer details and recognised quality certification. Be cautious of products making exaggerated health claims, as these are not permitted under UK regulations.
Finally, consider cost-effectiveness and practicality. Some products require multiple servings daily, which can become expensive. Assess whether the product fits your lifestyle and budget for sustained use.
Whilst mild electrolyte fluctuations may not cause noticeable symptoms, significant imbalances can be serious and require medical attention. Patients taking GLP-1 medications should be aware of warning signs that warrant consultation with healthcare services.
Seek urgent medical help if you experience signs of severe dehydration (extreme thirst, dry mouth/skin, little or no urination, dizziness, confusion, or rapid heartbeat), inability to keep fluids down, blood in vomit or stool, severe abdominal pain, or chest pain. For less urgent concerns, contact your GP or NHS 111.
Persistent gastrointestinal symptoms should not be ignored. If you're unable to maintain adequate fluid intake, or experience vomiting or diarrhoea that doesn't improve within 24 hours, contact your healthcare provider. These symptoms can lead to dehydration and electrolyte depletion, particularly in vulnerable individuals. Your doctor may need to temporarily adjust or pause your GLP-1 medication.
Be alert to specific GLP-1 medication red flags: severe, persistent abdominal pain (especially radiating to the back) with or without vomiting could indicate pancreatitis. If this occurs, stop taking your GLP-1 medication and seek immediate medical assessment. Similarly, symptoms of gallbladder disease (severe upper abdominal pain, especially after eating fatty foods) require prompt evaluation.
Patients with pre-existing medical conditions need closer monitoring. If you have chronic kidney disease, heart failure, liver disease, or take medications that affect electrolyte balance (such as diuretics, ACE inhibitors, or NSAIDs), discuss electrolyte supplementation with your doctor before starting. These conditions increase the risk of dangerous electrolyte imbalances.
Routine laboratory testing is not required for all patients before using electrolyte supplements. However, if you're experiencing symptoms or have risk factors, your GP may recommend checking your electrolyte levels and kidney function. Regular monitoring may be advised for some patients, especially during the initial months of GLP-1 treatment when side effects are most common.
If you experience any suspected side effects from your GLP-1 medication, report them through the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Whilst electrolyte powders can be convenient, they are not the only option for maintaining electrolyte balance during GLP-1 treatment. For many patients, dietary approaches and lifestyle modifications may be sufficient and more cost-effective.
Dietary sources of electrolytes are often preferable as they provide minerals in a natural, balanced form alongside other beneficial nutrients. Potassium-rich foods include bananas, oranges, potatoes, spinach, avocados, and beans. Magnesium is abundant in nuts, seeds, whole grains, leafy green vegetables, and legumes. Sodium needs can typically be met through a normal diet, though individuals experiencing significant losses may benefit from adding a small amount of salt to meals or consuming broth-based soups. Calcium is found in dairy products, fortified plant milks, leafy greens, and tinned fish with bones.
For patients struggling with reduced appetite due to GLP-1 medications, focusing on nutrient-dense foods becomes particularly important. Small, frequent meals that include electrolyte-rich options can help maintain balance whilst accommodating reduced gastric capacity. Smoothies can be an excellent vehicle for incorporating fruits, vegetables, and even a pinch of salt if needed.
Adequate hydration is fundamental. Plain water is essential, but for those experiencing acute gastrointestinal symptoms, oral rehydration solutions (ORS) available from pharmacies provide a medically formulated balance of electrolytes and glucose. These are particularly useful during episodes of vomiting or diarrhoea and are more appropriate than sports drinks, which often contain excessive sugar.
Coconut water provides potassium, magnesium, and sodium, though it contains natural sugars that should be considered in diabetes management. It can be high in potassium and should be used cautiously by those with chronic kidney disease or taking medications that increase potassium levels. Herbal teas with a small pinch of salt can provide gentle hydration for those struggling with nausea, though adding honey should be approached cautiously in diabetes.
It's worth noting that magnesium and calcium supplements can reduce the absorption of certain medications, including levothyroxine and some antibiotics. If you take these medicines, space doses by 2-4 hours.
Ultimately, the best approach is individualised. Some patients may manage well with dietary adjustments alone, whilst others experiencing persistent symptoms may benefit from occasional use of electrolyte products. Working with a registered dietitian can help develop a personalised nutrition plan that supports both your GLP-1 treatment goals and overall electrolyte balance.
Not all patients require electrolyte supplementation. It is primarily indicated for those experiencing significant gastrointestinal losses (vomiting or diarrhoea) or inadequate food and fluid intake, rather than routine use for all GLP-1 users.
Look for balanced amounts of sodium, potassium, magnesium, and chloride. Choose sugar-free products and avoid high-potassium formulations if you have kidney disease or take ACE inhibitors, ARBs, or potassium-sparing diuretics.
Seek urgent help for severe dehydration, inability to keep fluids down, blood in vomit or stool, or severe abdominal pain. Contact your GP for persistent gastrointestinal symptoms lasting over 24 hours or if you have pre-existing kidney, heart, or liver conditions.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.