Tirzepatide (Mounjaro) is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes and weight management in adults with obesity or overweight with comorbidities. Whilst clinical trials demonstrate significant efficacy, individual responses vary considerably. If tirzepatide isn't working as expected, several factors may be responsible—including inadequate dosing, lifestyle factors, unrealistic timelines, or underlying medical conditions. Understanding these variables and working closely with your healthcare provider can help optimise treatment outcomes. This article explores why tirzepatide may appear ineffective and what steps you can take to improve your response.
Quick Answer: Tirzepatide may not work effectively due to inadequate dosing, poor adherence, lifestyle factors counteracting its effects, or underlying medical conditions interfering with its mechanism of action.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist. In the UK, it is licensed as Mounjaro for the treatment of type 2 diabetes mellitus and, where applicable, for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with weight-related comorbidities. Whilst clinical trials have demonstrated significant efficacy in glycaemic control and weight reduction, individual responses can vary considerably.
If you feel tirzepatide is not working as expected, it is important to understand that several factors may influence treatment outcomes. The perception that tirzepatide "isn't working" may stem from unrealistic expectations about the speed or magnitude of results, inadequate dosing, lifestyle factors that counteract the medication's effects, or underlying medical conditions that interfere with its mechanism of action. In some cases, what appears to be treatment failure may actually represent a slower-than-expected response that will improve with time and dose optimisation.
Understanding your treatment goals is essential. For diabetes management, success is measured by improvements in HbA1c levels and fasting glucose, whilst for weight management, response is typically evaluated after reaching a maintenance dose for several months. Healthcare providers may assess whether you've achieved a clinically meaningful weight reduction (often defined as 5% or more of baseline weight) according to NICE guidance and the product's SmPC. If you are not achieving expected targets, a thorough review with your healthcare provider is warranted.
Important safety note: Do not use tirzepatide if you are pregnant or planning pregnancy. Seek urgent medical attention if you experience severe, persistent abdominal pain (which may indicate pancreatitis) or symptoms of gallbladder disease. If you take insulin or sulfonylureas alongside tirzepatide, be aware of the increased risk of hypoglycaemia.
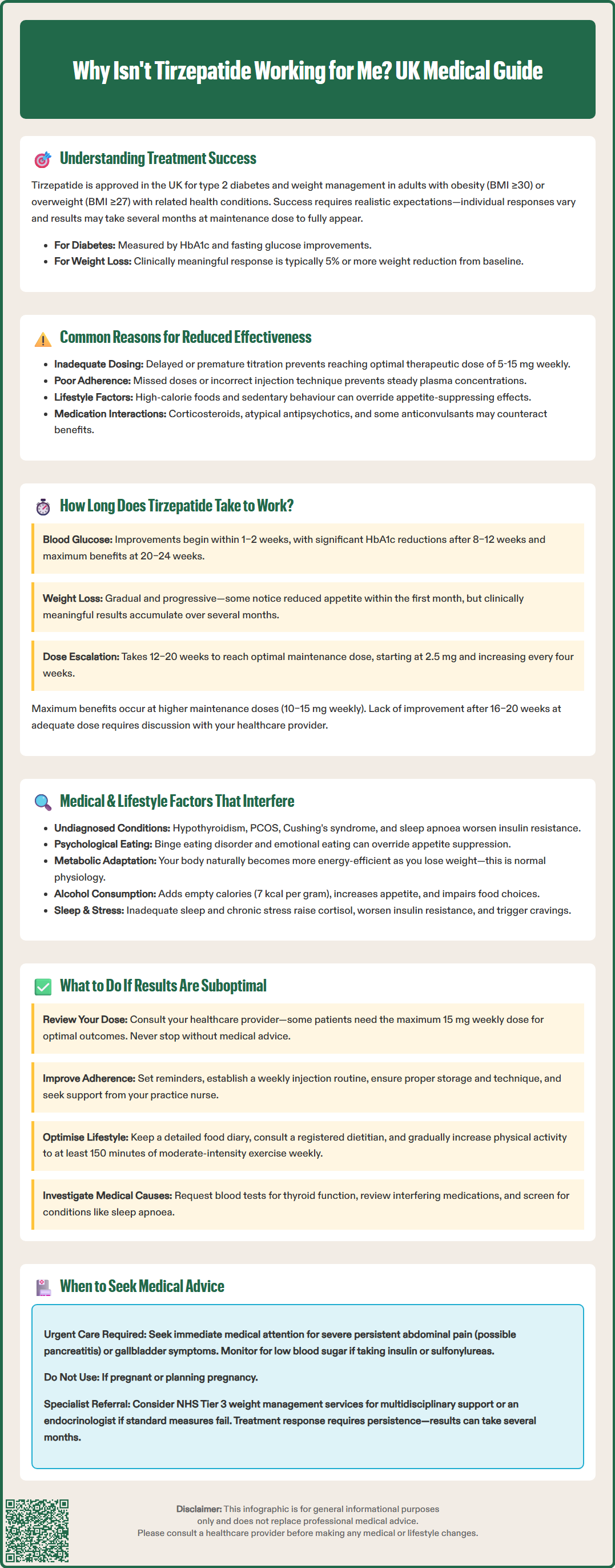
Several factors can contribute to suboptimal response to tirzepatide therapy. Inadequate dosing is among the most common reasons for apparent treatment failure. According to the MHRA SmPC, tirzepatide is initiated at a low dose (2.5 mg once weekly) and gradually titrated upwards at four-week intervals to minimise gastrointestinal side effects. Some patients may not reach their optimal therapeutic dose if titration is delayed or stopped prematurely due to side effects. The maintenance dose typically ranges from 5 mg to 15 mg weekly, depending on individual response and tolerability.
Poor medication adherence significantly impacts treatment outcomes. Missing doses or inconsistent administration can prevent tirzepatide from achieving steady-state plasma concentrations necessary for optimal efficacy. The once-weekly injection schedule is designed to improve adherence compared to daily medications, but patients may still struggle with remembering doses or experience injection site reactions that discourage regular use. Proper storage (refrigeration before first use), handling, and injection technique are also important for maintaining efficacy.
Dietary habits and lifestyle factors can substantially diminish tirzepatide's effectiveness. Whilst the medication reduces appetite and slows gastric emptying, consuming high-calorie, energy-dense foods in excess can override these effects. Similarly, a sedentary lifestyle limits the metabolic benefits of weight loss and glycaemic improvement. Tirzepatide works best when combined with a reduced-calorie diet and increased physical activity, as recommended by NICE guidance.
Concurrent medications may also interfere with tirzepatide's action. Certain drugs, particularly corticosteroids, atypical antipsychotics, and some anticonvulsants, can promote weight gain or worsen insulin resistance, counteracting tirzepatide's benefits. Additionally, tirzepatide itself delays gastric emptying, which may affect the absorption of concomitant oral medications, particularly those requiring rapid onset of action or specific blood concentrations.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereUnderstanding the expected timeline for tirzepatide's effects is crucial for setting realistic expectations and avoiding premature discontinuation. For glycaemic control in type 2 diabetes, improvements in blood glucose levels typically begin within the first few weeks of treatment. Based on clinical trial data (SURPASS programme), fasting glucose may start to decline within 1–2 weeks, whilst more substantial reductions in HbA1c become apparent after 8–12 weeks of therapy. Maximum glycaemic benefits are generally observed after 20–24 weeks, particularly as the dose is titrated to optimal levels.
For weight management, the timeline is somewhat longer. Whilst some patients notice reduced appetite and early weight loss within the first month, clinically significant weight reduction typically occurs over several months. According to the SURMOUNT trials, meaningful weight loss continues to accumulate over time, with greater effects seen at higher maintenance doses (10–15 mg weekly). It is important to note that weight loss with tirzepatide is gradual and progressive rather than immediate.
The dose escalation schedule also influences how quickly you experience benefits. Since treatment begins at a sub-therapeutic dose (2.5 mg) and increases every four weeks, it may take 12–20 weeks to reach your optimal maintenance dose. During this titration period, effects will be less pronounced than at higher doses. If you experience significant side effects, your healthcare provider may slow the titration schedule, which can delay reaching full therapeutic effect. Patience during this phase is essential, as premature judgement of efficacy can lead to unnecessary treatment changes.
Individual variation means some patients respond more quickly than others. Factors such as baseline weight, metabolic health, insulin sensitivity, and adherence to lifestyle modifications all influence the speed and magnitude of response. If you have not noticed any improvement after 16–20 weeks at an adequate dose, this warrants discussion with your healthcare provider.
Beyond the common reasons for suboptimal response, several specific factors can actively reduce tirzepatide's effectiveness. Underlying medical conditions may blunt treatment response. Hypothyroidism, polycystic ovary syndrome (PCOS), Cushing's syndrome, and other endocrine disorders can make weight loss more difficult and affect glucose metabolism. Sleep apnoea, which is common in obesity, can worsen insulin resistance and limit metabolic improvements. If these conditions are undiagnosed or inadequately treated, tirzepatide's benefits may be diminished.
Psychological factors and eating behaviours play a significant role. Binge eating disorder, emotional eating, and other disordered eating patterns can override the appetite-suppressing effects of tirzepatide. Whilst the medication reduces physiological hunger, it does not address psychological drivers of food consumption. Patients with these patterns may benefit from psychological support through NHS Talking Therapies or referral to specialist weight management services (Tier 3) as outlined in NICE guidance (CG189).
Metabolic adaptation can occur with significant weight loss. As body weight decreases, metabolic rate naturally declines, and the body becomes more efficient at conserving energy. This adaptive thermogenesis can slow weight loss progress over time, creating the impression that the medication has stopped working. This is a normal physiological response rather than true treatment failure.
Alcohol consumption can significantly impact results. Alcohol provides empty calories (7 kcal per gram) and can stimulate appetite whilst impairing judgement around food choices. Regular or excessive alcohol intake can substantially reduce the caloric deficit necessary for weight loss. Additionally, inadequate sleep and chronic stress elevate cortisol levels, promote insulin resistance, and increase cravings for high-calorie foods, all of which can counteract tirzepatide's metabolic benefits.
Important safety note: Seek urgent medical attention if you experience severe abdominal pain, persistent vomiting leading to dehydration, or symptoms of gallbladder disease, as these may represent serious complications requiring immediate assessment.
If you believe tirzepatide is not providing the expected benefits, do not discontinue treatment without consulting your healthcare provider. There are several steps you and your clinician can take to optimise your response. First, review your current dose and titration schedule. If you are still on a low dose or have not completed the full titration to a maintenance dose, continuing to increase the dose as tolerated may improve outcomes. Some patients require the maximum dose (15 mg weekly) to achieve optimal results.
Assess medication adherence honestly with your healthcare team. If you have missed doses or struggled with the injection schedule, discuss strategies to improve adherence, such as setting reminders, linking injections to a weekly routine, or addressing any injection-related concerns. Your practice nurse or diabetes specialist nurse can provide additional support with injection technique and site rotation to minimise discomfort. Ensure you're following the correct storage requirements (refrigeration before first use) and missed-dose instructions as per the SmPC.
Evaluate lifestyle factors comprehensively. Keep a detailed food diary for at least one week to identify hidden sources of excess calories or patterns of emotional eating. Consider referral to a registered dietitian for personalised nutritional guidance. Increase physical activity gradually, aiming for at least 150 minutes of moderate-intensity exercise weekly, as recommended by the UK Chief Medical Officers' Physical Activity Guidelines. Even modest increases in activity can enhance tirzepatide's effects.
Investigate potential underlying causes. Your healthcare provider may recommend blood tests to check thyroid function (TSH, free T4) or other investigations based on clinical suspicion. Review any medications that might interfere with weight loss or glycaemic control. If you have symptoms of sleep apnoea (loud snoring, daytime fatigue, witnessed breathing pauses), discuss screening with your GP.
Consider specialist referral if standard measures are unsuccessful. NHS Tier 3 weight management services can provide multidisciplinary support including psychological intervention, specialist dietetic input, and structured lifestyle programmes. For diabetes management, referral to an endocrinologist may be appropriate if glycaemic targets remain unmet despite optimised tirzepatide therapy.
Important safety considerations: If tirzepatide is used with insulin or sulfonylureas, dose adjustments of these medications may be needed to prevent hypoglycaemia. Do not use tirzepatide with other GLP-1 receptor agonists or DPP-4 inhibitors. If you experience side effects, report them through the MHRA Yellow Card scheme. Remember that treatment response can take several months, and persistence with therapy alongside lifestyle optimisation offers the best chance of success.
Clinically significant weight loss with tirzepatide typically occurs over several months, with meaningful reductions usually evident after reaching maintenance doses (10–15 mg weekly). Whilst some patients notice reduced appetite within the first month, full therapeutic effects generally develop over 16–24 weeks as the dose is gradually titrated upwards.
Yes, consuming high-calorie foods in excess, maintaining a sedentary lifestyle, regular alcohol consumption, inadequate sleep, and chronic stress can all substantially reduce tirzepatide's effectiveness. The medication works best when combined with a reduced-calorie diet and increased physical activity as recommended by NICE guidance.
Do not discontinue treatment without consulting your healthcare provider. Discuss dose optimisation, review medication adherence, evaluate lifestyle factors comprehensively, and investigate potential underlying conditions such as thyroid disorders or sleep apnoea. Your GP may recommend specialist referral to NHS Tier 3 weight management services or an endocrinologist for further assessment and support.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.