Rybelsus (semaglutide) is an oral GLP-1 receptor agonist licensed in the UK for type 2 diabetes management. Whilst effective in improving glycaemic control, evidence links GLP-1 therapies to an increased risk of gallbladder and biliary disorders. Can Rybelsus cause gallbladder problems? Clinical data confirm that Rybelsus may contribute to conditions such as cholecystitis and cholelithiasis, primarily through rapid weight loss and altered gallbladder function. The Rybelsus Summary of Product Characteristics lists gallbladder disorders as uncommon adverse reactions. Understanding these risks, recognising symptoms early, and knowing when to seek medical attention are essential for safe diabetes management. This article examines the evidence, risk factors, and clinical guidance for UK patients and healthcare professionals.
Quick Answer: Rybelsus can cause gallbladder problems, with gallbladder disorders listed as uncommon adverse reactions affecting between 1 in 100 and 1 in 1,000 patients.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereRybelsus (semaglutide) is an oral glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Whilst Rybelsus is generally well-tolerated and effective in improving glycaemic control, there is established evidence linking GLP-1 receptor agonists to an increased risk of gallbladder and biliary disorders.
The mechanism by which Rybelsus may contribute to gallbladder problems is multifactorial. Rapid weight loss, a common effect of GLP-1 therapy, is a well-established risk factor for gallstone formation (cholelithiasis). When weight is lost quickly, the liver secretes extra cholesterol into bile, whilst the gallbladder's motility may be reduced, creating conditions favourable for stone development. Additionally, GLP-1 receptor agonists may directly affect gallbladder contractility and bile composition, though the precise pathophysiology requires further investigation.
Clinical trial data and post-marketing surveillance have identified cases of cholecystitis (gallbladder inflammation), cholelithiasis, and cholangitis in patients treated with semaglutide. According to the Rybelsus Summary of Product Characteristics (SmPC), gallbladder disorders are listed as uncommon adverse reactions (affecting between 1 in 100 and 1 in 1,000 patients). Meta-analyses suggest a modest increased relative risk of gallbladder disease with GLP-1 receptor agonists, with the absolute risk remaining small at doses used for type 2 diabetes.
The Medicines and Healthcare products Regulatory Agency (MHRA) and the European Medicines Agency (EMA) have acknowledged these risks in their assessments. Patients prescribed Rybelsus should be informed about this potential risk and advised to report symptoms suggestive of gallbladder pathology promptly. Healthcare professionals should maintain clinical vigilance, particularly in those with additional risk factors for biliary disease.
Suspected adverse reactions to Rybelsus, including gallbladder problems, should be reported via the MHRA Yellow Card Scheme.
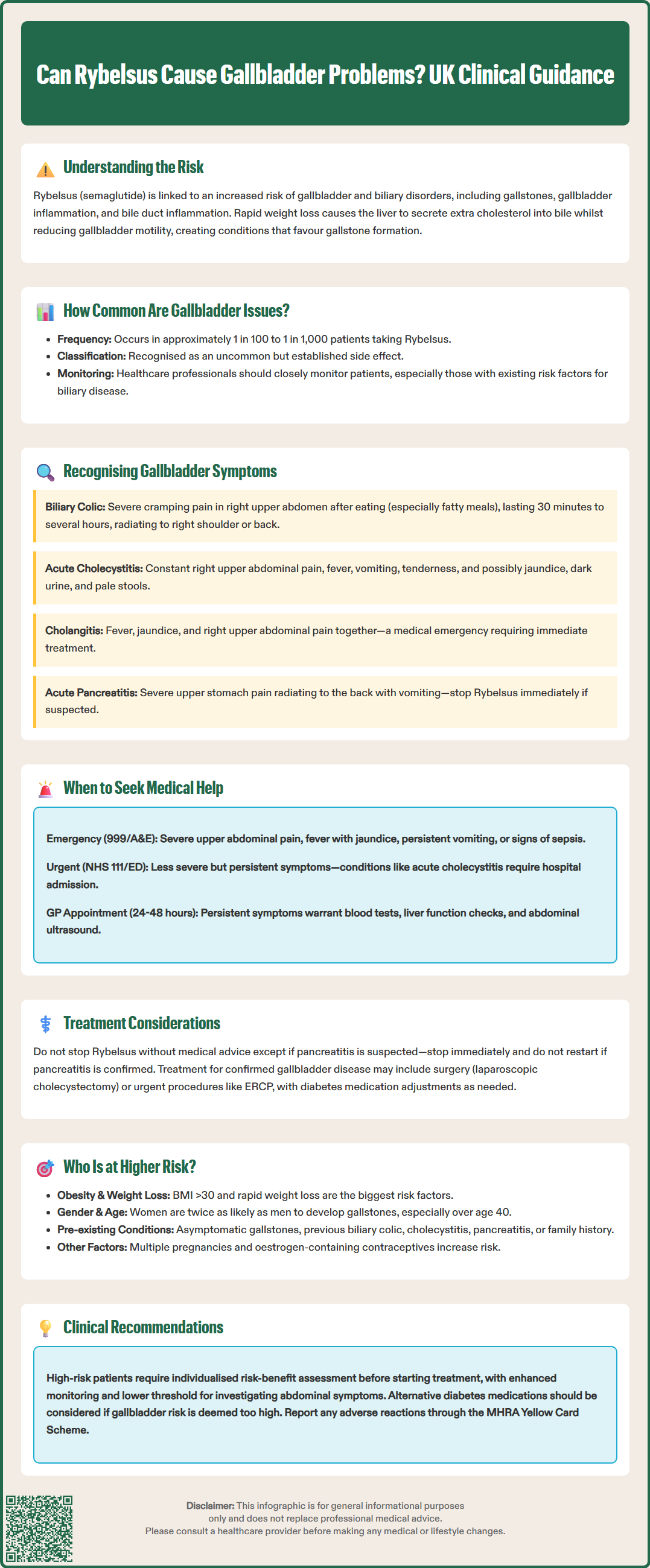
Early recognition of gallbladder-related symptoms is essential for timely diagnosis and management. Patients taking Rybelsus should be educated about the cardinal features of gallbladder disease, which may present acutely or develop gradually.
The most characteristic symptom is biliary colic—a severe, cramping pain in the right upper quadrant or epigastrium that may radiate to the right shoulder or back. This pain typically occurs after meals, particularly those high in fat, and may last from 30 minutes to several hours. Unlike the common gastrointestinal side effects of Rybelsus (nausea, vomiting, diarrhoea), biliary pain is usually more intense, persistent, and positionally unrelieved.
Acute cholecystitis presents with constant right upper quadrant pain, fever, and systemic upset. Patients may experience:
Persistent nausea and vomiting
Fever and rigors
Tenderness when the right upper abdomen is examined (Murphy's sign)
Jaundice (yellowing of skin and eyes), suggesting bile duct involvement
Dark urine and pale stools
Loss of appetite and general malaise
Cholangitis (infection of the bile ducts) may present with Charcot's triad: fever, jaundice, and right upper quadrant pain. This requires emergency treatment.
Acute pancreatitis can occur with severe epigastric pain radiating to the back, often accompanied by vomiting. The Rybelsus SmPC advises stopping treatment immediately if pancreatitis is suspected.
It is crucial to distinguish these symptoms from the expected gastrointestinal effects of Rybelsus, which are usually mild to moderate, occur early in treatment, and improve over time. Gallbladder symptoms tend to be more severe, localised, and associated with systemic features. Any patient experiencing persistent right upper quadrant pain, particularly if accompanied by fever or jaundice, should seek medical attention promptly.
If you develop symptoms suggestive of gallbladder disease whilst taking Rybelsus, prompt medical assessment is essential. Do not dismiss persistent abdominal pain as a routine side effect of your diabetes medication.
Call 999 or go to A&E immediately if you experience:
Severe, unrelenting right upper quadrant or epigastric pain
Fever above 38°C accompanied by abdominal pain and jaundice
Jaundice (yellowing of the skin or whites of the eyes)
Persistent vomiting preventing oral intake
Signs of sepsis (confusion, rapid heartbeat, breathlessness, feeling extremely unwell)
In less severe but concerning circumstances, contact NHS 111 or attend your local Emergency Department for urgent evaluation. Acute cholecystitis, cholangitis and pancreatitis are potentially serious conditions requiring hospital admission and specialist care.
For less severe but persistent symptoms, arrange a face-to-face appointment with your GP within 24–48 hours. Your doctor will perform a clinical examination and arrange appropriate investigations, which typically include:
Blood tests: Full blood count, liver function tests, inflammatory markers (CRP), amylase/lipase to assess for pancreatitis, and blood cultures if fever is present
Abdominal ultrasound: The first-line imaging modality for detecting gallstones, gallbladder wall thickening, and bile duct dilatation (NICE CG188)
Further imaging (CT or MRCP) may be indicated if complications are suspected
Do not stop Rybelsus abruptly without medical advice, as this may affect your glycaemic control. However, if pancreatitis is suspected, the SmPC advises stopping semaglutide immediately; if pancreatitis is confirmed, treatment should not be restarted.
If gallbladder disease is confirmed, management options range from conservative measures to surgical intervention. NICE recommends early laparoscopic cholecystectomy (gallbladder removal) for acute cholecystitis where appropriate. Suspected cholangitis may require urgent endoscopic retrograde cholangiopancreatography (ERCP). Your diabetes treatment plan may need adjustment in consultation with your diabetes specialist team.
Certain patient groups face elevated risk of developing gallbladder complications during Rybelsus therapy. Understanding these risk factors enables targeted patient counselling and enhanced clinical surveillance.
Obesity and substantial weight loss represent the most significant risk factors. Patients with a body mass index (BMI) above 30 kg/m² are inherently at increased risk of gallstone formation, and this risk is amplified during periods of rapid weight reduction. Women, particularly those of reproductive age with obesity, constitute a particularly high-risk demographic according to NHS guidance on gallstone risk factors.
Pre-existing gallbladder disease is an important consideration. Patients with:
Known asymptomatic gallstones (cholelithiasis)
Previous episodes of biliary colic
History of cholecystitis or pancreatitis
Family history of gallbladder disease
should be counselled about the potential for symptom development or disease progression during GLP-1 therapy.
Additional factors that contribute to risk stratification include:
Female sex: Women are approximately twice as likely as men to develop gallstones
Age: Risk increases progressively after age 40
Dyslipidaemia: Elevated triglycerides and cholesterol increase lithogenic potential
Pregnancy and parity: Multiple pregnancies increase risk
Oestrogen therapy: Including combined hormonal contraceptives
For high-risk patients, NICE guidance supports individualised risk-benefit assessment before initiating GLP-1 therapy. Enhanced patient education, regular monitoring, and a lower threshold for investigating abdominal symptoms are prudent strategies in this population. Alternative glucose-lowering agents should be considered if the risk profile is deemed unacceptably high.
Patients should report any suspected side effects to their healthcare professional or directly to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Gallbladder disorders are classified as uncommon adverse reactions to Rybelsus, affecting between 1 in 100 and 1 in 1,000 patients according to the Summary of Product Characteristics. The absolute risk remains small, though clinical vigilance is advised.
Key warning signs include severe right upper quadrant pain (especially after meals), fever, jaundice, persistent vomiting, dark urine, and pale stools. These symptoms differ from common Rybelsus side effects and require prompt medical assessment.
Do not stop Rybelsus without medical advice, as this may affect glycaemic control. Seek urgent medical assessment if you develop concerning symptoms; your doctor will advise whether to continue or discontinue treatment based on clinical findings.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.