Rybelsus (semaglutide) is an oral GLP-1 receptor agonist prescribed for type 2 diabetes management. Whilst gastrointestinal symptoms are the most frequently reported adverse effects, some patients experience itching during treatment. According to the Medicines and Healthcare products Regulatory Agency (MHRA) Summary of Product Characteristics, pruritus is classified as an uncommon side effect. Understanding when itching warrants medical attention and how to manage it safely is essential for patients continuing their diabetes treatment. This article examines the relationship between Rybelsus and itching, potential causes, and appropriate management strategies aligned with UK clinical guidance.
Quick Answer: Itching is an uncommon side effect of Rybelsus (semaglutide), affecting up to 1 in 100 people according to MHRA-approved prescribing information.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereRybelsus (semaglutide) is an oral medication used to manage type 2 diabetes mellitus, and whilst itching is not listed amongst its most common side effects, some patients do report experiencing pruritus (itching) during treatment. According to the Summary of Product Characteristics (SmPC) approved by the Medicines and Healthcare products Regulatory Agency (MHRA), itching is classified as an uncommon side effect with semaglutide preparations.
The relationship between Rybelsus and itching is not straightforward. Whilst clinical trials have documented cases of pruritus, it falls into the 'uncommon' frequency category (may affect up to 1 in 100 people) according to the SmPC. It is important to distinguish between itching that may be directly related to the medication and itching that could arise from other causes, such as underlying skin conditions, allergic reactions to excipients in the tablet, or coincidental dermatological issues.
Patients experiencing itching whilst taking Rybelsus should not immediately discontinue their medication without medical guidance. The symptom may be mild and transient, resolving as the body adjusts to treatment. However, persistent or severe itching, particularly when accompanied by other symptoms such as rash, swelling, or difficulty breathing, warrants prompt medical assessment. If you experience severe allergic symptoms, call 999 or go to A&E immediately. For less urgent concerns, contact your GP or call NHS 111 for advice. Understanding the potential causes and appropriate management strategies can help patients continue their diabetes treatment safely whilst addressing any uncomfortable symptoms that may arise.
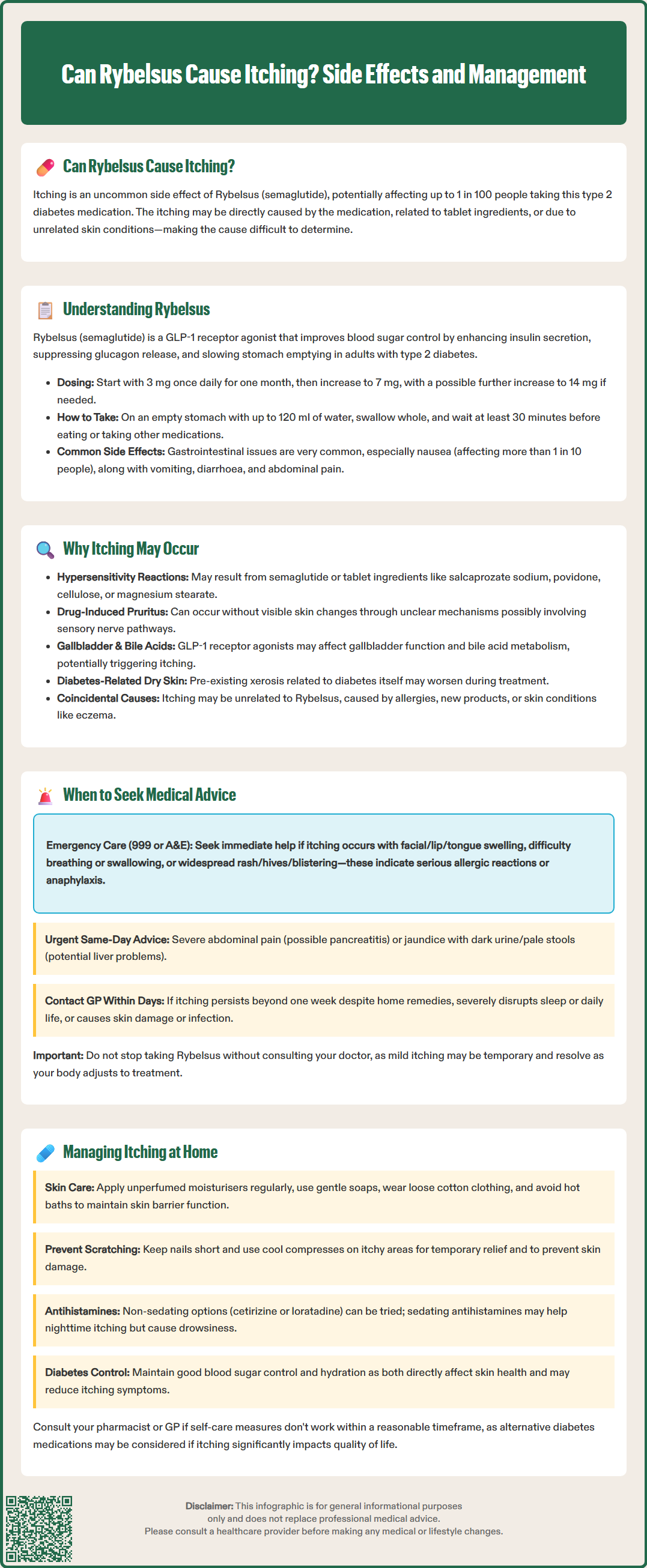
Rybelsus contains semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist that works by mimicking the action of naturally occurring incretin hormones. This medication enhances insulin secretion in a glucose-dependent manner, suppresses inappropriate glucagon release, and slows gastric emptying. These mechanisms collectively improve glycaemic control in adults with type 2 diabetes mellitus.
Rybelsus must be taken correctly to ensure absorption: take on an empty stomach with up to 120 ml of water, swallow the tablet whole (do not split, crush or chew), and wait at least 30 minutes before eating, drinking or taking other oral medicines. Rybelsus is typically initiated at 3 mg once daily for one month, then increased to 7 mg, with a possible further increase to 14 mg if additional glycaemic control is required.
The most frequently reported adverse effects of Rybelsus are gastrointestinal in nature, affecting a significant proportion of patients, particularly during the initial weeks of treatment. According to the SmPC, these include:
Nausea – very common (may affect more than 1 in 10 people)
Vomiting and diarrhoea – common (may affect up to 1 in 10 people)
Abdominal pain and decreased appetite – common
Constipation and dyspepsia – common
These gastrointestinal symptoms typically diminish over time as the body adapts to the medication. Other recognised side effects include hypoglycaemia (particularly when used with insulin or sulphonylureas) and rare cases of pancreatitis. If pancreatitis is suspected, Rybelsus should be discontinued immediately and not restarted if pancreatitis is confirmed. Patients should be counselled about these potential effects before commencing treatment, and healthcare professionals should monitor for tolerability, especially during dose escalation phases.
Patients with diabetes who experience rapid improvement in blood glucose control should be monitored for diabetic retinopathy complications, as per the SmPC. Understanding the expected side effect profile helps patients distinguish between common, manageable symptoms and those requiring medical attention.
Several mechanisms may explain why some patients experience itching whilst taking Rybelsus, though the precise pathophysiology remains incompletely understood. Hypersensitivity reactions represent one potential cause, whereby the immune system responds to either the active ingredient (semaglutide) or one of the tablet's excipients, which according to the SmPC include salcaprozate sodium, povidone, cellulose, and magnesium stearate. Such reactions may manifest as pruritus with or without visible skin changes.
Some patients may experience what is termed 'drug-induced pruritus' – itching that occurs without obvious skin lesions or systemic allergic features. While the exact mechanism for this with Rybelsus is not fully established, it may involve complex interactions with sensory nerve pathways.
Another consideration involves changes in bile acid metabolism. The European Medicines Agency's European Public Assessment Report (EPAR) for Rybelsus notes that GLP-1 receptor agonists can influence gallbladder function, with an increased risk of gallbladder and biliary adverse events. Alterations in bile acid circulation have been associated with pruritus in some contexts, though this connection with Rybelsus specifically requires further research.
Additionally, patients with diabetes may have pre-existing skin conditions or xerosis (dry skin) related to their metabolic condition, which could be exacerbated during treatment.
It is also worth noting that coincidental causes should not be overlooked. Patients starting Rybelsus may simultaneously experience itching from entirely unrelated factors such as seasonal allergies, new skincare products, laundry detergents, or dermatological conditions like eczema or psoriasis. A thorough assessment is therefore essential to determine whether the medication is genuinely implicated or whether alternative explanations exist.
If you suspect Rybelsus is causing side effects, you can report them through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk), which helps monitor medication safety.
Whilst mild itching may not always require immediate medical intervention, certain features should prompt patients to seek appropriate healthcare support. Emergency medical attention is warranted if itching is accompanied by:
Facial swelling, lip swelling, or tongue swelling – potential signs of angioedema
Difficulty breathing or swallowing – indicating possible anaphylaxis
Widespread rash, hives, or blistering – suggesting serious allergic reaction
In these situations, call 999 or go to A&E immediately.
Patients should also seek urgent medical advice (same day via GP or NHS 111) if they experience:
Severe abdominal pain – which could indicate pancreatitis, a serious complication. If pancreatitis is suspected, Rybelsus should be discontinued immediately and not restarted if pancreatitis is confirmed.
Yellowing of the skin or eyes (jaundice), dark urine or pale stools – which could indicate hepatobiliary issues
For routine medical advice (within a few days), contact your GP if you experience:
Persistent itching lasting more than one week despite simple measures
Itching that significantly disrupts sleep or daily activities
Development of skin changes such as excoriation marks, secondary infection, or unexplained bruising
When consulting a healthcare professional, patients should provide a comprehensive history including when the itching started relative to commencing Rybelsus, its location and severity, any associated symptoms, and whether any new products or medications have been introduced. This information helps clinicians determine whether the itching represents a medication-related adverse effect, an allergic reaction, or an unrelated dermatological condition. In some cases, temporary discontinuation of Rybelsus under medical supervision may be necessary to establish causality, though this decision should only be made by a qualified healthcare professional who can weigh the benefits of continued diabetes management against the discomfort of the symptom.
For patients experiencing mild to moderate itching whilst taking Rybelsus, several management strategies may provide relief whilst allowing continuation of diabetes treatment. First-line measures include:
Emollients and moisturisers – regular application of unperfumed, hypoallergenic moisturisers can help maintain skin barrier function and reduce itching, particularly if xerosis contributes to symptoms
Avoiding irritants – using gentle, fragrance-free soaps and detergents, wearing loose cotton clothing, and avoiding hot baths which can exacerbate dry skin
Cool compresses – applying cool, damp cloths to itchy areas can provide temporary symptomatic relief
Keeping nails short – to minimise skin damage from scratching and reduce risk of secondary infection
Pharmacological options may be considered under medical guidance. Non-sedating antihistamines such as cetirizine or loratadine can be trialled, though their efficacy for non-histamine-mediated itching varies. For nocturnal itching disrupting sleep, a sedating antihistamine like chlorphenamine might be suggested by a healthcare provider for short-term use. Note that chlorphenamine causes drowsiness and may affect your ability to drive or operate machinery; alcohol should be avoided when taking it.
Topical corticosteroids may be appropriate if there is associated inflammation or dermatitis, but should only be used following medical assessment. The lowest potency effective corticosteroid should be used for short courses on affected areas only.
Patients should maintain optimal diabetes control and stay well-hydrated, as both factors influence skin health. If symptoms persist despite these self-care measures, consult your pharmacist or GP for further advice. Regular follow-up with the prescribing clinician is essential to monitor symptom progression and treatment response. If itching persists despite conservative measures, or if it significantly impacts quality of life, the healthcare team may consider alternative diabetes medications. However, such decisions must balance the effectiveness of Rybelsus in achieving glycaemic targets against the burden of side effects. Documentation of symptoms, their severity, and response to interventions helps guide these clinical decisions and ensures patient-centred care that optimises both diabetes management and overall wellbeing.
Remember to report suspected side effects to the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Itching (pruritus) is classified as an uncommon side effect of Rybelsus according to the MHRA Summary of Product Characteristics, potentially affecting up to 1 in 100 people taking the medication.
Do not stop Rybelsus without medical guidance. Mild itching may resolve as your body adjusts, but persistent or severe itching, especially with rash, swelling, or breathing difficulties, requires prompt medical assessment via your GP, NHS 111, or emergency services.
Apply unperfumed emollients regularly, use gentle fragrance-free soaps, wear loose cotton clothing, and try cool compresses. Non-sedating antihistamines may help under medical guidance, and you should consult your GP or pharmacist if symptoms persist despite these measures.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.