
Many patients using Ozempic (semaglutide) wonder whether the injection site affects weight loss outcomes. Ozempic is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed by the MHRA for type 2 diabetes mellitus, with weight loss as a recognised effect. However, it is not licensed in the UK for weight management alone—Wegovy (semaglutide 2.4mg) holds specific authorisation for chronic weight management. This article examines the approved injection sites for Ozempic, explores whether site selection influences efficacy, and provides guidance on safe administration technique in line with UK clinical standards and manufacturer recommendations.
Quick Answer: No single injection site produces greater weight loss with Ozempic; all three approved sites (abdomen, thigh, upper arm) deliver consistent absorption when proper technique and rotation are used.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed by the MHRA for the treatment of type 2 diabetes mellitus. Whilst weight loss is a recognised effect of the medication, it is important to note that Ozempic is not licensed in the UK for weight management alone. A separate formulation, Wegovy (also semaglutide but at a higher 2.4mg dose), holds specific marketing authorisation for chronic weight management in adults with obesity or overweight with weight-related comorbidities, typically prescribed within specialist weight management services under NICE TA875.
The mechanism by which semaglutide promotes weight loss involves several physiological pathways. As a GLP-1 analogue, it binds to GLP-1 receptors in the pancreas, brain, and gastrointestinal tract. This action slows gastric emptying, which prolongs the sensation of fullness after eating. Additionally, semaglutide acts on appetite-regulating centres in the hypothalamus, reducing hunger and overall caloric intake. In clinical trials, patients using the higher 2.4mg dose (Wegovy) experienced significant reductions in body weight—typically 10–15% of baseline weight over 68 weeks. At the lower doses used for diabetes (Ozempic 0.25mg, 0.5mg, 1mg, and 2mg), weight loss is generally more modest.
It is essential to understand that semaglutide should be used as part of a comprehensive weight management programme that includes dietary modification, increased physical activity, and behavioural support. The medication is administered once weekly via subcutaneous injection, and adherence to proper injection technique is crucial for both efficacy and safety. Patients considering Ozempic should discuss their suitability with a healthcare professional, as off-label use carries specific considerations regarding monitoring, contraindications, and potential adverse effects.
Importantly, semaglutide should be discontinued at least two months before a planned pregnancy and is not recommended during pregnancy or breastfeeding.
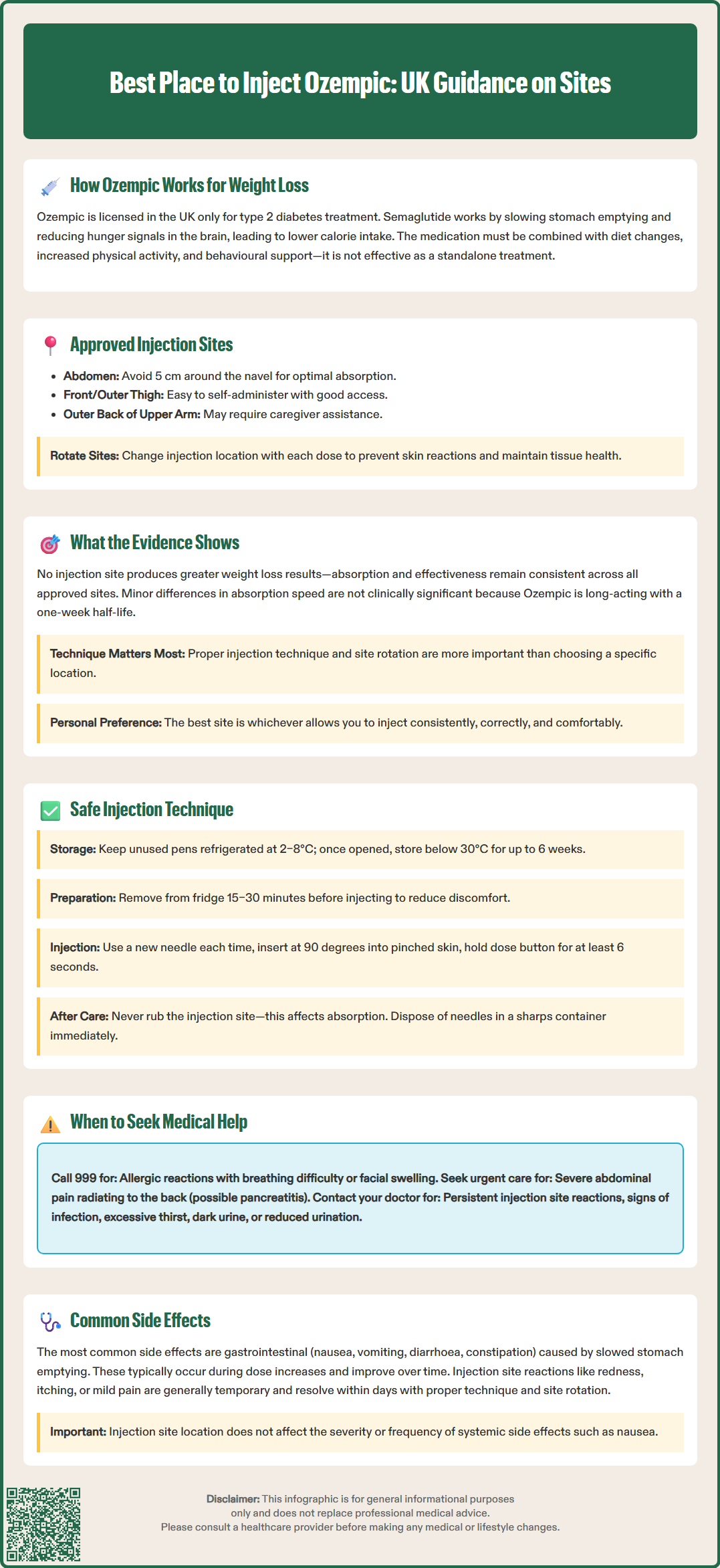
Ozempic is administered as a subcutaneous injection, meaning it is delivered into the fatty tissue layer beneath the skin rather than into muscle or a vein. According to the Summary of Product Characteristics (SmPC) approved by the MHRA and guidance from Novo Nordisk (the manufacturer), there are three approved injection sites for Ozempic:
Abdomen (stomach area): The front of the abdomen, avoiding a 5 cm radius around the navel
Thigh: The front or outer aspect of the thigh, typically the upper to mid-thigh region
Upper arm: The outer back portion of the upper arm, where there is adequate subcutaneous tissue
These sites are selected because they contain sufficient subcutaneous fat to allow proper absorption of the medication whilst minimising discomfort and the risk of inadvertent intramuscular injection. Rotating injection sites is strongly recommended to reduce the risk of injection site reactions, maintain skin integrity, and ensure consistent absorption. Patients should avoid injecting into areas where the skin is tender, bruised, red, hard, or scarred.
It is worth noting that whilst all three sites are officially approved, individual patient factors may influence site selection. These include body composition, skin condition, personal comfort, and the ability to reach the injection site independently. Many patients find that upper arm injections are difficult to self-administer and may require assistance from a caregiver. Healthcare professionals should provide personalised guidance during initial training, and patients should feel confident in their injection technique before self-administering at home.
Pens and needles should never be shared with others, even if the needle has been changed, due to the risk of cross-infection. Each injection should be performed with a new needle to maintain sterility and ensure proper delivery of the medication.
A common question among patients is whether one injection site is superior to others for maximising weight loss or minimising side effects. There is no official evidence to suggest that any single injection site produces greater weight loss outcomes when using Ozempic. According to the MHRA-approved SmPC for Ozempic, the pharmacokinetics of semaglutide—how the drug is absorbed, distributed, and metabolised—remain consistent across all three approved injection sites when proper technique is used.
Small studies examining subcutaneous insulin absorption have shown minor variations in absorption rates between sites (with abdominal injections sometimes showing slightly faster absorption), but these differences are not clinically significant for long-acting medications like semaglutide. Ozempic has a half-life of approximately one week, meaning it remains in the system for an extended period, and any minor variations in absorption speed do not materially affect steady-state drug levels or therapeutic outcomes.
What matters more than site selection is consistency and proper technique. Patients should rotate sites systematically (for example, alternating between abdomen, thigh, and upper arm across consecutive weeks) whilst ensuring each injection is delivered into subcutaneous tissue at the correct depth. Injecting too superficially may cause leakage or reduced absorption, whilst injecting too deeply into muscle can alter absorption patterns and increase discomfort.
Patient preference plays a legitimate role in site selection. Some individuals find the abdomen most convenient and least painful, whilst others prefer the thigh for ease of access. The 'best' site is ultimately the one where the patient can consistently perform the injection correctly, comfortably, and safely. Healthcare professionals should support patients in identifying their preferred site whilst emphasising the importance of rotation to maintain skin integrity.
Proper injection technique is essential for ensuring optimal drug delivery, minimising discomfort, and reducing the risk of complications. Patients should receive comprehensive training from a healthcare professional before self-administering Ozempic. The following steps outline best practice:
Preparation:
Store unused Ozempic pens in the refrigerator (2–8°C); once in use, they may be kept at room temperature (below 30°C) for up to 6 weeks
Remove the pen from the refrigerator 15–30 minutes before injection to allow it to reach room temperature, reducing injection discomfort
Wash hands thoroughly with soap and water
Check the medication is clear and colourless; do not use if cloudy, discoloured, or containing particles
Injection technique:
Clean the chosen injection site with an alcohol wipe and allow to dry completely
Attach a new needle to the pen for each injection
Perform an airshot (flow check) when starting a new pen as per manufacturer instructions to ensure the pen is working correctly
Pinch the skin gently to lift the subcutaneous tissue away from underlying muscle
Insert the needle at a 90-degree angle (or 45 degrees if very lean) in a swift, smooth motion
Press the dose button fully and hold for at least 6 seconds to ensure complete delivery
Withdraw the needle and dispose of it immediately in a sharps container
Post-injection care:
Do not rub the injection site, as this may affect absorption
Record the site used to facilitate rotation
Monitor for any unusual reactions
Dispose of used needles in a designated sharps bin (available from your GP, pharmacy, or local council)
Never share your pen with others, even if you change the needle
When to seek medical attention:
For severe abdominal pain (especially if radiating to the back), stop using Ozempic and seek urgent medical care via NHS 111 or A&E
For signs of allergic reaction (difficulty breathing, swelling of face/throat), call 999
For persistent pain, swelling, or redness at injection sites
Signs of infection (warmth, pus, fever)
Severe or worsening gastrointestinal symptoms, especially with signs of dehydration
Unexplained persistent nausea or vomiting
Like all medications, Ozempic can cause side effects, though not everyone experiences them. The most frequently reported adverse effects are gastrointestinal in nature and include nausea, vomiting, diarrhoea, constipation, and abdominal pain. These symptoms are related to the drug's mechanism of action (slowing gastric emptying) rather than the injection site chosen. They typically occur during dose escalation and often improve over time as the body adjusts.
Injection site reactions are generally mild and may include:
Redness or discoloration
Itching
Swelling or bruising
Mild pain or tenderness
These local reactions usually resolve within a few days and can be minimised through proper injection technique and systematic site rotation. There is no evidence that injection site selection influences the severity or frequency of systemic side effects such as nausea or gastrointestinal disturbance.
More serious but rare adverse effects include:
Pancreatitis: Severe, persistent abdominal pain (often radiating to the back) requires immediate medical attention and discontinuation of semaglutide
Gallbladder problems: Symptoms include upper abdominal pain, fever, and jaundice
Hypoglycaemia: More likely when used with insulin or sulphonylureas (medication review may be needed)
Diabetic retinopathy complications: Patients with pre-existing retinopathy should be monitored
Allergic reactions: Rash, difficulty breathing, or swelling of face/throat (seek emergency care)
Severe gastrointestinal side effects may lead to dehydration and acute kidney injury. Patients should maintain adequate fluid intake and seek urgent medical attention if experiencing signs of dehydration (excessive thirst, dry mouth, reduced urination, dark urine).
Patients should be counselled about these potential adverse effects during initiation. NICE guidance (NG28 for diabetes; TA875 for weight management) recommends regular monitoring during treatment. Any persistent, severe, or concerning symptoms warrant prompt medical review. Suspected side effects can be reported via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
No, there is no evidence that any single injection site produces greater weight loss outcomes. The pharmacokinetics of semaglutide remain consistent across all three approved sites (abdomen, thigh, upper arm) when proper technique is used.
You should rotate between the three approved injection sites systematically, for example alternating between abdomen, thigh, and upper arm across consecutive weeks. This reduces the risk of injection site reactions and maintains skin integrity.
Stop using Ozempic immediately and seek urgent medical care via NHS 111 or A&E, as severe abdominal pain (especially if radiating to the back) may indicate pancreatitis, a serious but rare adverse effect requiring prompt medical attention.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.