Many people prescribed Mounjaro (tirzepatide) for type 2 diabetes wonder whether they can continue drinking milk during treatment. The good news is that there are no pharmacological interactions between Mounjaro and milk or dairy products. However, understanding how this medication affects digestion can help you make informed choices about dairy consumption. This article explores the relationship between Mounjaro and milk, addressing common concerns about tolerance, nutritional considerations, and practical guidance for including dairy in your diet whilst managing type 2 diabetes effectively.
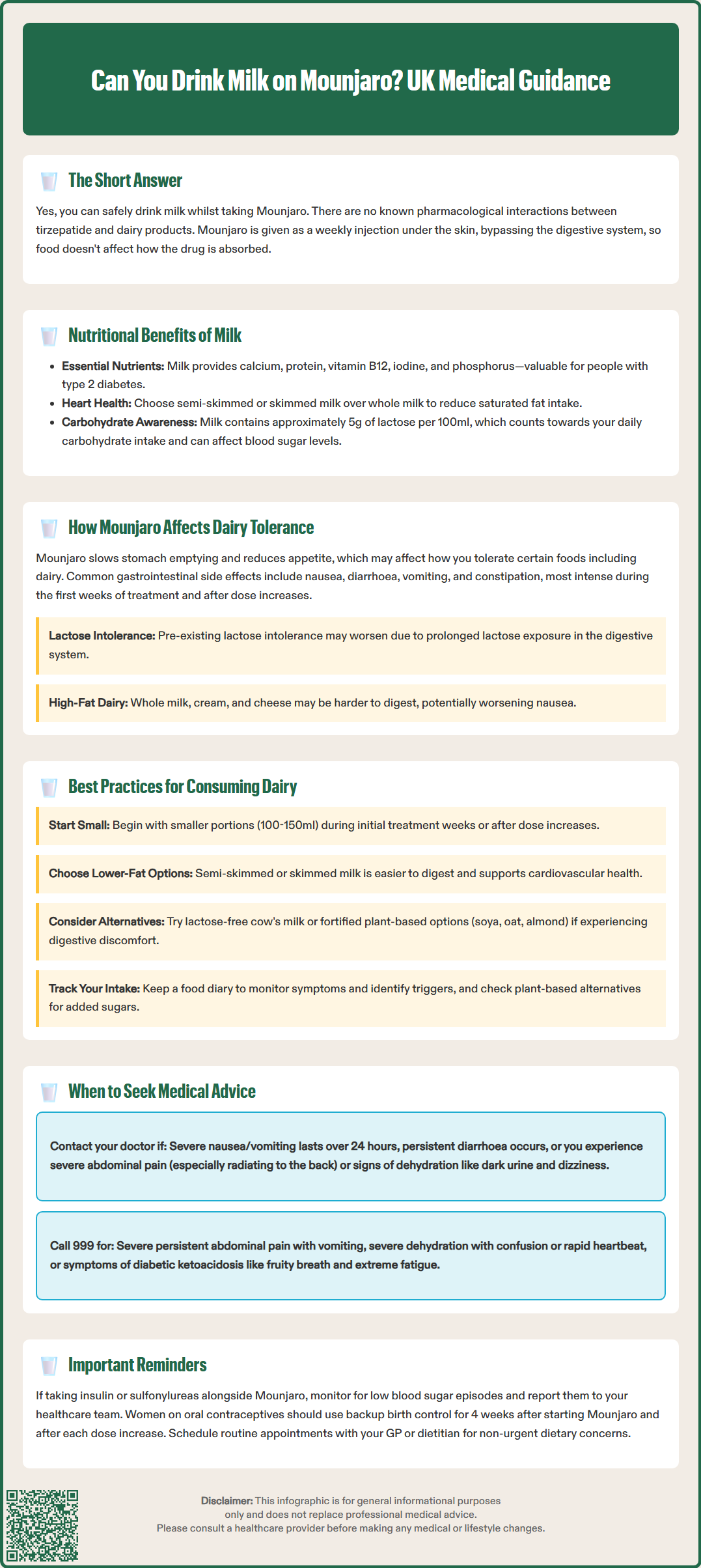
Quick Answer: Yes, you can drink milk whilst taking Mounjaro, as there are no pharmacological interactions between tirzepatide and dairy products.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMounjaro (tirzepatide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of medications known as dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonists. Tirzepatide works by mimicking the action of naturally occurring incretin hormones, which help regulate blood glucose levels by stimulating insulin secretion when blood sugar is elevated, suppressing glucagon release, and slowing gastric emptying.
Unlike some medications that require specific dietary restrictions or have direct interactions with certain foods, Mounjaro does not have any known pharmacological interactions with milk or dairy products. The medication is administered as a once-weekly subcutaneous injection, meaning it bypasses the gastrointestinal tract for absorption. This route of administration eliminates concerns about food affecting the drug's bioavailability, as can occur with oral medications.
However, understanding how Mounjaro affects the digestive system is important when considering dietary choices, including dairy consumption. The medication's mechanism of slowing gastric emptying and reducing appetite can influence how patients tolerate various foods. Whilst there is no medical contraindication to drinking milk whilst taking Mounjaro, individual tolerance may vary based on the medication's gastrointestinal effects.
It's important to note that milk contains lactose (a carbohydrate), which can impact blood glucose levels. People with diabetes should account for this in their overall carbohydrate intake and blood glucose management.
Patients prescribed Mounjaro should receive comprehensive counselling about the medication's effects and general dietary guidance. The MHRA-approved product information does not list milk or dairy as substances to avoid. However, the SmPC does note that tirzepatide can delay gastric emptying, which may reduce the exposure to oral contraceptives. Women using oral contraceptives should consider additional or alternative contraception for 4 weeks after initiating Mounjaro and following each dose escalation.
Yes, you can drink milk whilst taking Mounjaro. There are no official contraindications or warnings against consuming milk or other dairy products during tirzepatide treatment. The medication does not interact with dairy at a pharmacological level, and milk consumption will not reduce the effectiveness of Mounjaro through a direct drug-food interaction.
Milk and dairy products can form part of a balanced diet for individuals with type 2 diabetes. Semi-skimmed and skimmed milk provide valuable nutrients, including:
Calcium – essential for bone health
Protein – important for maintaining muscle mass during weight loss
Vitamin B12 – crucial for neurological function
Iodine – necessary for thyroid function
Phosphorus – supports bone and teeth health
It's important to remember that milk contains approximately 5g of lactose (milk sugar) per 100ml, which contributes to your overall carbohydrate intake and can affect blood glucose levels. For people managing type 2 diabetes, choosing lower-fat dairy options is generally recommended as part of a heart-healthy diet. Whole milk contains higher levels of saturated fat, which may contribute to cardiovascular risk when consumed in excess. The NHS Eatwell Guide suggests choosing lower-fat and lower-sugar dairy alternatives where possible.
Patients taking Mounjaro alongside insulin or sulfonylureas should be particularly mindful of their carbohydrate intake, including from milk, as these medication combinations can increase the risk of hypoglycaemia. Regular blood glucose monitoring is advisable, and medication doses may need adjustment with healthcare professional guidance.
It is worth noting that whilst milk itself does not interact with Mounjaro, individual tolerance to dairy may change during treatment due to the medication's effects on the digestive system. Some patients report increased sensitivity to certain foods, including dairy, particularly during the initial weeks of treatment or following dose escalations. These effects are related to how the medication affects gastrointestinal function rather than a true drug-food interaction, and they often improve as the body adjusts to treatment.
Mounjaro's mechanism of action includes delayed gastric emptying, which means food remains in the stomach for longer periods before moving into the small intestine. This physiological effect contributes to increased satiety and reduced appetite, supporting weight management and glycaemic control. However, delayed gastric emptying can also influence how patients tolerate various foods, including dairy products.
The most commonly reported gastrointestinal side effects of Mounjaro according to the SmPC include:
Nausea (very common, affecting up to one-third of patients at higher doses)
Diarrhoea (very common)
Vomiting (very common)
Constipation (common)
Abdominal discomfort or pain (common)
Reduced appetite (very common)
Dyspepsia (indigestion) (common)
These effects are typically most pronounced during the first few weeks of treatment and following dose increases. For some individuals, consuming dairy products—particularly full-fat milk, cream, or cheese—during this adjustment period may exacerbate feelings of nausea or fullness due to the higher fat content, which naturally slows digestion further.
Some patients with pre-existing lactose intolerance, which affects approximately 5% of Northern European populations and higher percentages in other ethnic groups, may notice their symptoms become more apparent during Mounjaro treatment. This could potentially be due to the delayed gastric emptying prolonging the time lactose remains in the digestive system, though this specific mechanism has not been formally studied. Symptoms might include bloating, cramping, or diarrhoea when consuming milk.
It's also worth noting that GLP-1 receptor agonists like tirzepatide have been associated with gallbladder-related events, including cholelithiasis (gallstones) and cholecystitis. While this is not directly related to milk consumption, patients should be aware of this potential side effect and seek medical attention for persistent right upper quadrant pain, fever, or jaundice.
Patients who notice digestive discomfort after consuming dairy whilst on Mounjaro might consider switching to lactose-free milk alternatives or reducing portion sizes. These adjustments can help distinguish between medication-related gastrointestinal effects and dairy intolerance.
To optimise comfort and nutritional intake whilst taking Mounjaro, consider the following evidence-based recommendations for dairy consumption:
Start with smaller portions: During the initial weeks of treatment or after dose escalations, begin with smaller servings of milk and dairy products. A small glass of milk (100–150ml) rather than a large serving may be better tolerated as your digestive system adjusts to the medication's effects.
Choose lower-fat options: Semi-skimmed or skimmed milk is generally better tolerated than whole milk, as the reduced fat content means quicker digestion. This can help minimise feelings of fullness or nausea. Lower-fat dairy choices also align with cardiovascular health recommendations for people with type 2 diabetes, as advised in the NHS Eatwell Guide.
Time your dairy consumption thoughtfully: Some patients find that consuming dairy products earlier in the day, when nausea tends to be less pronounced, improves tolerance. Avoid drinking large quantities of milk immediately before bed, as lying down with delayed gastric emptying may increase reflux symptoms.
Consider lactose-free alternatives: If you suspect lactose intolerance is contributing to digestive discomfort, lactose-free cow's milk provides the same nutritional benefits without the problematic sugar. Alternatively, fortified plant-based milk alternatives (soya, oat, almond) can provide calcium and other nutrients. Choose unsweetened, fortified versions and check labels for calcium, iodine and vitamin B12 content. Be aware that protein content varies significantly between plant milks, with soya typically offering the highest protein levels.
Be mindful of carbohydrates: Remember that milk contains carbohydrates (lactose) that affect blood glucose. If using plant-based alternatives, check for added sugars which can impact glycaemic control.
Maintain adequate hydration: Ensure you're drinking sufficient water throughout the day, as dehydration can worsen constipation—a common side effect of Mounjaro. Don't rely solely on milk for fluid intake.
Keep a food diary: Recording what you eat and any symptoms experienced can help identify specific triggers and patterns. This information is valuable when discussing dietary tolerance with your GP or diabetes specialist nurse.
Prioritise protein intake: If dairy tolerance is reduced, ensure adequate protein from other sources such as lean meats, fish, eggs, legumes, and plant-based proteins to support muscle maintenance during weight loss.
Whilst mild gastrointestinal effects are common when starting Mounjaro, certain symptoms warrant medical attention. Contact your GP or diabetes care team if you experience:
Persistent or severe nausea and vomiting that prevents you from keeping down fluids or food for more than 24 hours, as this increases the risk of dehydration and may require dose adjustment or temporary treatment interruption
Severe abdominal pain, particularly if constant or radiating to the back, which could indicate pancreatitis—a rare but serious side effect of GLP-1 receptor agonists requiring immediate medical assessment
Signs of dehydration including dark urine, dizziness, reduced urination, or extreme thirst, especially if accompanied by vomiting or diarrhoea, which may lead to acute kidney injury
Unexplained weight loss exceeding clinical targets or loss of muscle mass
Persistent diarrhoea lasting more than a few days, which may indicate an underlying issue requiring investigation
Difficulty maintaining adequate nutrition due to food intolerances or reduced appetite
Recurrent hypoglycaemia (low blood sugar), particularly if you're also taking insulin or sulfonylureas, which may require dose adjustments of these medications
Right upper quadrant pain, fever, or yellowing of the skin/eyes, which could indicate gallbladder problems reported with GLP-1 receptor agonists
Seek urgent medical attention (call 999 or attend A&E) if you develop:
Severe, persistent abdominal pain with vomiting
Signs of severe dehydration (confusion, rapid heartbeat, very low urine output)
Symptoms of diabetic ketoacidosis (though rare in type 2 diabetes unless insulin-deficient or during acute illness): excessive thirst, frequent urination, nausea, abdominal pain, confusion, unusual fatigue, fruity-smelling breath
For non-urgent dietary concerns, schedule a routine appointment with your GP, practice nurse, or diabetes specialist dietitian. They can provide personalised nutritional guidance, assess whether symptoms are medication-related or indicate other conditions, and adjust your treatment plan if necessary. Regular review of patients on GLP-1 receptor agonists is recommended to assess tolerability, effectiveness, and nutritional status.
If you're considering significant dietary changes, including eliminating dairy products, discuss this with your healthcare team to ensure nutritional adequacy and appropriate supplementation if needed. For urgent advice when unsure, contact NHS 111.
No, Mounjaro (tirzepatide) does not have any known pharmacological interactions with milk or dairy products. As it is administered by subcutaneous injection, food does not affect its absorption or effectiveness.
Mounjaro delays gastric emptying, meaning food stays in the stomach longer. This can make higher-fat dairy products feel heavier or increase nausea, particularly during the first few weeks of treatment or after dose increases.
Semi-skimmed or skimmed milk is generally better tolerated than whole milk due to lower fat content, which aids digestion. Lactose-free or fortified plant-based alternatives may suit those with lactose intolerance or digestive sensitivity.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.