
Injection site reactions are a recognised side effect of tirzepatide, a dual GIP and GLP-1 receptor agonist administered as a weekly subcutaneous injection for type 2 diabetes and weight management. Whilst generally mild and self-limiting, these localised reactions—including redness, swelling, itching, and bruising—can cause discomfort and concern for patients. Understanding why these reactions occur, how to minimise their frequency, and when to seek medical advice is essential for safe, effective treatment. This article provides evidence-based guidance on managing injection site reactions with tirzepatide, aligned with UK clinical practice and MHRA recommendations.
Quick Answer: Injection site reactions with tirzepatide are generally mild, self-limiting localised responses such as redness, swelling, itching, or bruising that typically resolve within 2–3 days without specific treatment.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereTirzepatide is a glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. In the UK, tirzepatide (Mounjaro) is also authorised for weight management in adults with obesity or overweight with weight-related comorbidities, subject to specific eligibility criteria. Tirzepatide works through dual incretin receptor activation that enhances glycaemic control and promotes weight reduction.
The medication is administered as a subcutaneous injection once weekly. Tirzepatide is supplied in pre-filled, single-dose pens containing doses ranging from 2.5 mg to 15 mg, with treatment typically initiated at the lowest dose and gradually titrated upwards every four weeks to minimise gastrointestinal side effects and optimise therapeutic response.
Recommended injection sites include:
The abdomen (avoiding the area around the navel)
The front of the thighs
The upper arms (if administered by another person)
Patients should rotate injection sites with each dose to reduce the risk of local tissue reactions. The injection can be administered at any time of day, with or without meals, though maintaining a consistent weekly schedule is advisable. Proper injection technique is essential—the pen should be held at a 90-degree angle to the skin, and after pressing the button, the pen should be held against the skin for 10 seconds until you hear or feel a second click to ensure complete dose delivery. The pre-filled pens are for single use only and should be disposed of safely after one injection. Healthcare professionals typically provide initial training on correct administration technique, and the Patient Information Leaflet contains detailed visual instructions.
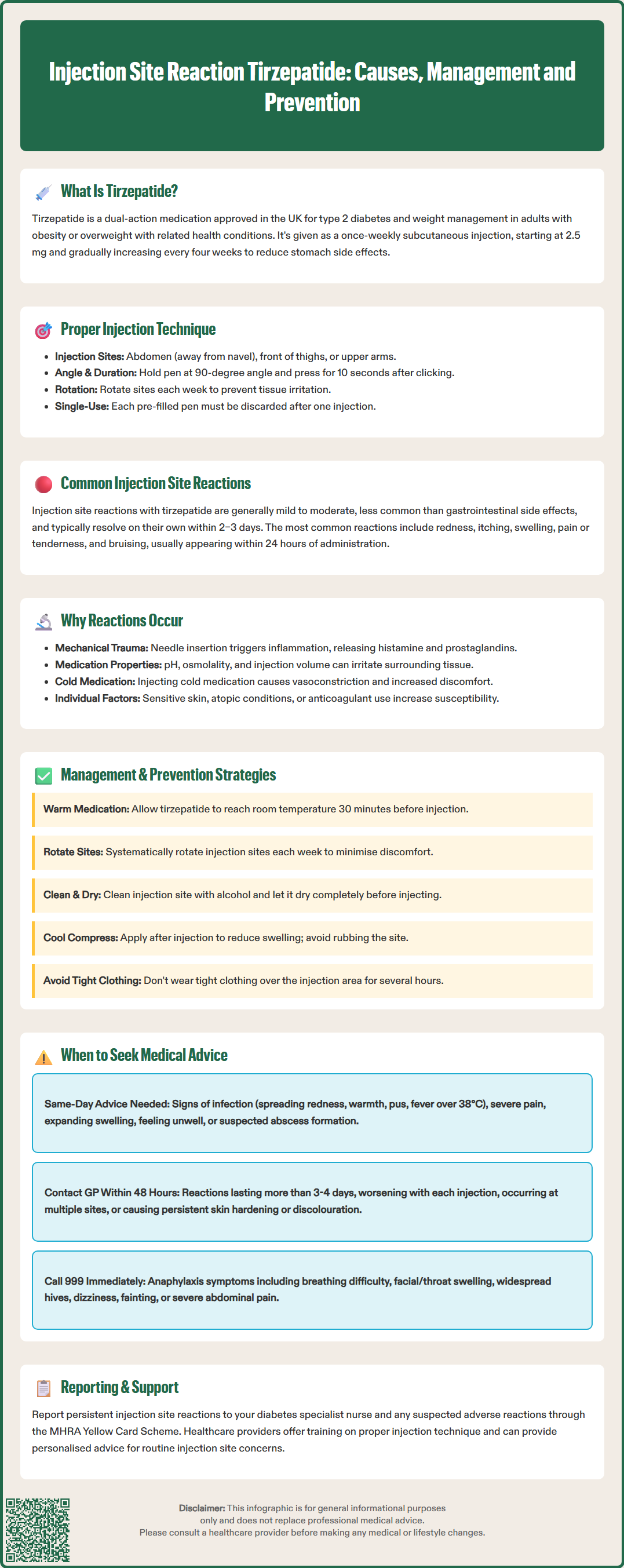
Injection site reactions can occur with tirzepatide therapy, though they are generally mild to moderate in severity and tend to resolve spontaneously without intervention. According to the MHRA Summary of Product Characteristics, injection site reactions are less common than gastrointestinal side effects. Clinical trial data from the SURPASS programme indicates that these reactions occur in a small percentage of patients receiving tirzepatide.
The most common injection site reactions include:
Erythema (redness): Localised redness surrounding the injection site, typically appearing within minutes to hours after administration
Pruritus (itching): Mild to moderate itching at or around the injection site
Swelling or induration: Raised, firm areas of skin that may persist for several hours
Pain or tenderness: Discomfort ranging from mild sensitivity to more pronounced soreness
Bruising (ecchymosis): Small haematomas resulting from minor blood vessel trauma during injection
Most injection site reactions develop within 24 hours of administration and resolve within 2–3 days without specific treatment. The reactions are typically localised and do not spread beyond the immediate injection area. Importantly, the frequency and severity of these reactions often diminish with continued use as patients become more proficient with injection technique and the body adapts to regular subcutaneous administration.
It is worth noting that injection site reactions do not necessarily indicate an allergic response to tirzepatide itself. Rather, they frequently result from mechanical trauma, injection technique, or localised inflammatory responses to the subcutaneous depot. However, persistent, worsening, or unusually severe reactions warrant medical review to exclude hypersensitivity or infection.
Understanding the underlying mechanisms of injection site reactions can help patients and healthcare professionals implement effective preventive strategies. Several factors contribute to the development of these localised responses, ranging from the physical properties of the medication to individual patient characteristics and injection technique.
Mechanical trauma represents the most straightforward cause. The act of piercing the skin and subcutaneous tissue with a needle inevitably causes minor tissue damage, triggering an inflammatory cascade. This physiological response involves the release of histamine, prostaglandins, and other inflammatory mediators, resulting in the classic signs of redness, warmth, and swelling. Damaged needles or rapid injection can exacerbate this trauma.
The formulation characteristics of injectable medications may also contribute to localised reactions. When injected subcutaneously, differences in pH and osmolality compared to physiological tissue fluid can create a temporary chemical gradient that may irritate surrounding tissues. Additionally, the volume of injection creates a depot that must be gradually absorbed, and this process can cause transient discomfort or visible swelling.
Individual patient factors play a significant role. Patients with sensitive skin, a history of atopic conditions, or those taking anticoagulant medications may be more prone to injection site reactions. Subcutaneous fat distribution, skin thickness, and local blood flow also influence how the body responds to injection. Injecting into areas with less subcutaneous fat or into muscle rather than the subcutaneous layer can increase discomfort and visible reactions.
Temperature of the medication is another important consideration. Injecting cold medication directly from refrigerated storage can cause vasoconstriction and increased discomfort. Allowing the pen to reach room temperature for 30 minutes before injection significantly reduces this effect.
Whilst injection site reactions are generally self-limiting, several evidence-based strategies can minimise their occurrence and severity, improving patient comfort and treatment adherence. Both preventive measures and symptomatic management approaches should be considered.
Optimising injection technique:
Allow medication to reach room temperature: Remove the pen from the refrigerator 30 minutes before injection to reduce discomfort
Ensure proper needle insertion: Insert at a 90-degree angle with a swift, confident motion
Rotate injection sites systematically: Use a different site each week and avoid injecting into areas that have not fully recovered
Avoid injecting into areas with visible skin changes: Do not inject into bruised, scarred, inflamed or infected skin
Use each pen only once: Tirzepatide pens are single-use devices and should be disposed of safely after one injection
Pre-injection preparation:
Clean the injection site with an alcohol wipe and allow it to dry completely before injecting (wet alcohol can cause stinging)
Gently pinch the skin to create a subcutaneous fold, ensuring injection into fat rather than muscle
Relax the injection area—tense muscles can increase discomfort
Post-injection care:
Apply gentle pressure with clean gauze if minor bleeding occurs, but avoid rubbing the site
A cool compress (not ice directly on skin) can reduce swelling and discomfort
Avoid tight clothing over the injection site for several hours
Monitor the site for 24–48 hours for any worsening symptoms
Symptomatic relief: For mild itching or discomfort, over-the-counter oral antihistamines (such as cetirizine) may provide relief, though patients should consult their pharmacist or GP before starting any new medication to check for potential interactions or contraindications. Topical treatments should only be used if specifically prescribed by a healthcare professional.
Patients experiencing persistent reactions despite optimal technique should discuss alternative injection sites or administration strategies with their diabetes specialist nurse or prescribing clinician.
Suspected adverse reactions to tirzepatide should be reported via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
Whilst most injection site reactions are benign and self-resolving, certain features warrant prompt medical assessment to exclude complications such as infection, abscess formation, or hypersensitivity reactions. Patients should be educated about warning signs that require professional evaluation.
Seek same-day medical advice if:
Signs of infection develop: Increasing redness spreading beyond the injection site, warmth, purulent discharge, or fever (temperature >38°C)
Severe pain: Pain that is disproportionate to the visible reaction or that interferes with daily activities
Large or expanding swelling: Induration or oedema that is progressively enlarging
Systemic symptoms: Feeling generally unwell, with malaise, fever, or lymph node swelling
Abscess formation: A fluctuant, tender mass suggesting collection of pus
Contact your GP or diabetes team within 48 hours if:
Injection site reactions persist beyond 3–4 days without improvement
Reactions are becoming progressively more severe with each injection
You develop reactions at multiple injection sites simultaneously
Skin changes such as persistent hardening, discolouration, or induration occur
You experience recurrent reactions despite optimal injection technique
Seek emergency care (999 or A&E) if signs of anaphylaxis develop:
Difficulty breathing or wheezing
Swelling of the face, lips, tongue, or throat
Widespread urticarial rash (hives)
Dizziness, fainting, or rapid pulse
Severe abdominal pain or vomiting
These symptoms, whilst extremely rare with tirzepatide, represent serious hypersensitivity reactions requiring immediate medical intervention. Patients with a confirmed severe allergic reaction should not continue tirzepatide and should be referred to an allergy specialist for assessment. For routine injection site concerns, diabetes specialist nurses provide an invaluable resource for troubleshooting technique and offering practical advice tailored to individual circumstances.
Most injection site reactions with tirzepatide develop within 24 hours of administration and resolve spontaneously within 2–3 days without specific treatment. Reactions persisting beyond 3–4 days warrant medical review.
Yes, preventive strategies include allowing the pen to reach room temperature before injection, systematically rotating injection sites each week, ensuring proper 90-degree needle insertion technique, and avoiding injection into bruised or damaged skin.
Seek same-day medical advice if you develop signs of infection (spreading redness, warmth, discharge, fever), severe or disproportionate pain, large expanding swelling, or systemic symptoms. Emergency care is required for signs of anaphylaxis such as difficulty breathing or facial swelling.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.