Many patients prescribed Wegovy (semaglutide) for weight management wonder whether using cannabis is safe or affects treatment outcomes. Wegovy is a GLP-1 receptor agonist licensed by the MHRA for chronic weight management, working by suppressing appetite and slowing gastric emptying. Cannabis, particularly THC, stimulates appetite and affects gastrointestinal function—systems that overlap with Wegovy's mechanisms. Whilst no formal pharmacokinetic interaction is listed, the opposing effects on appetite and potential for compounded side effects raise clinically important concerns. This article examines the evidence, risks, and medical guidance to help patients make informed decisions and communicate openly with healthcare professionals about substance use during Wegovy treatment.
Quick Answer: No formal drug interaction exists between cannabis and Wegovy, but cannabis may counteract Wegovy's appetite-suppressing effects and compound gastrointestinal side effects, potentially compromising weight loss outcomes.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
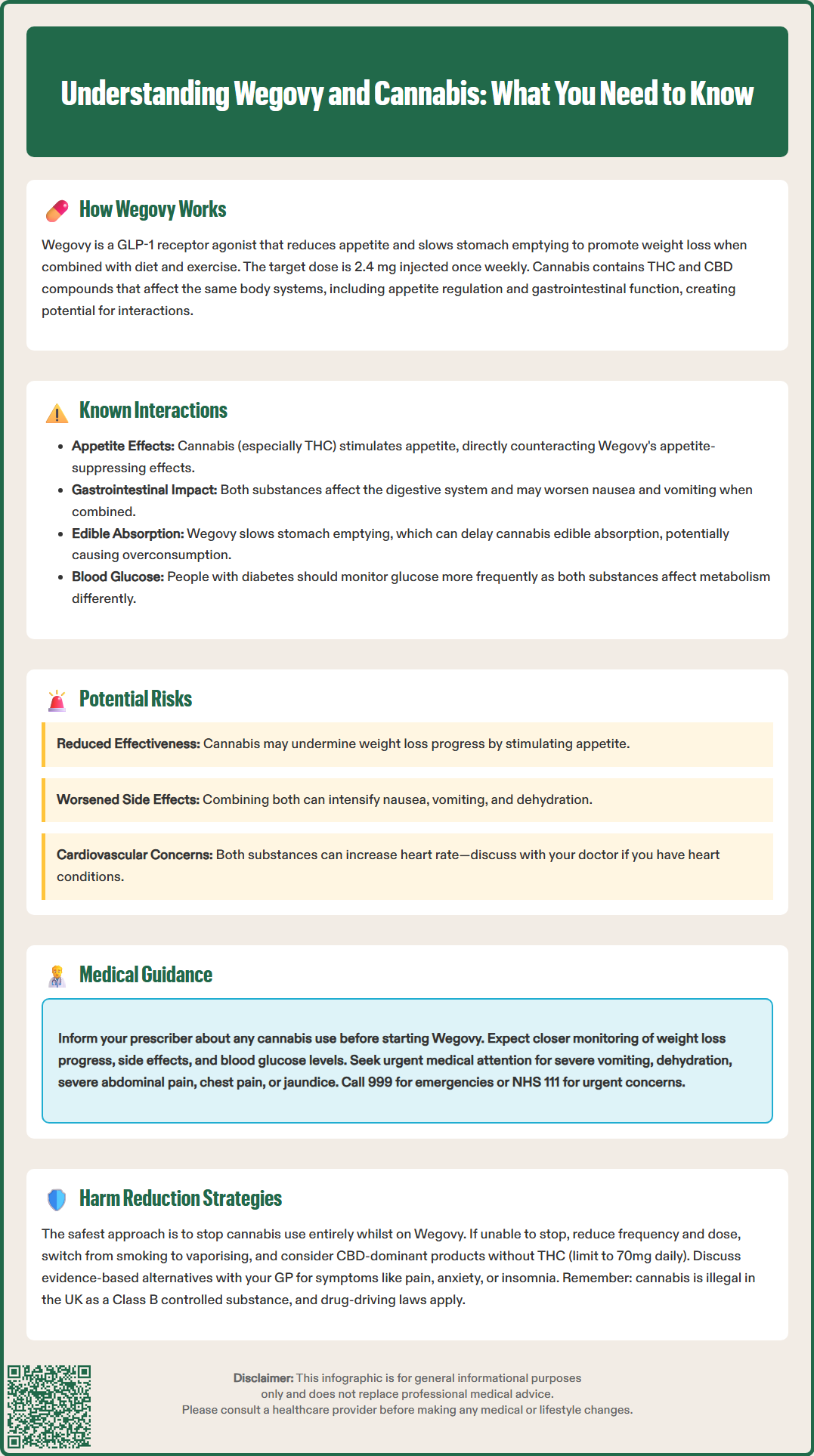
Start HereWegovy (semaglutide) is a prescription medicine licensed by the MHRA for chronic weight management in adults with obesity or overweight with weight-related comorbidities. It belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking a naturally occurring hormone that regulates appetite and food intake. Wegovy slows gastric emptying, increases feelings of fullness, and reduces hunger signals in the brain, leading to reduced calorie intake and gradual weight loss when combined with a reduced-calorie diet and increased physical activity.
The recommended dose of Wegovy is 2.4 mg once weekly, reached through a 16-week dose escalation schedule (0.25 mg, 0.5 mg, 1.0 mg, 1.7 mg, then 2.4 mg). Some patients may remain on the 1.7 mg dose if the higher dose is not tolerated. NHS eligibility criteria under NICE TA875 are more restrictive than the MHRA licence, with specific BMI thresholds and service requirements.
Cannabis refers to products derived from the Cannabis sativa plant, containing psychoactive compounds such as delta-9-tetrahydrocannabinol (THC) and non-psychoactive cannabidiol (CBD). In the UK, recreational cannabis remains a controlled Class B drug under the Misuse of Drugs Act 1971, though medical cannabis can be prescribed in limited circumstances. Cannabis affects the endocannabinoid system, influencing appetite, mood, pain perception, and gastrointestinal function—systems that may overlap with Wegovy's mechanisms.
Many patients prescribed Wegovy may wonder whether using cannabis—whether recreationally or medicinally—poses risks or affects treatment efficacy. This is a clinically relevant question, as both substances influence appetite regulation and gastrointestinal function. Additionally, Wegovy's effect on delaying gastric emptying may affect the absorption of orally consumed substances, including cannabis edibles. Understanding the potential interactions, risks, and medical guidance is essential for patient safety and treatment success. This article provides evidence-based information to help patients and healthcare professionals navigate this complex topic, emphasising the importance of open communication with prescribers about all substance use.
According to the British National Formulary (BNF) and the Wegovy Summary of Product Characteristics (SmPC), there is no listed pharmacokinetic interaction between cannabis and semaglutide. This means that cannabis does not appear to directly alter how the body absorbs, metabolises, or eliminates Wegovy, nor does Wegovy significantly change cannabis metabolism through hepatic enzyme systems.
However, the absence of a listed drug interaction does not mean the combination is without concern. Both substances affect overlapping physiological systems, particularly:
Appetite regulation: Cannabis, particularly THC, is well known for stimulating appetite (colloquially termed "the munchies") by activating CB1 receptors in the hypothalamus and limbic system. This effect directly opposes Wegovy's appetite-suppressing mechanism, potentially reducing the medication's effectiveness in promoting weight loss.
Gastrointestinal effects: Wegovy commonly causes nausea, vomiting, diarrhoea, and constipation, especially during dose escalation. Cannabis has complex gastrointestinal effects—whilst some patients use it to manage nausea, chronic heavy use is associated with cannabinoid hyperemesis syndrome (CHS), characterised by severe cyclical vomiting.
Metabolic effects: Both substances influence glucose metabolism and insulin sensitivity, though through different mechanisms. The clinical significance of combined use on glycaemic control remains unclear, and people with diabetes should monitor their blood glucose levels more frequently if using both substances.
Absorption effects: Wegovy significantly delays gastric emptying, which may alter the absorption timing of orally consumed cannabis products (edibles). This could lead to delayed onset of effects, potentially causing users to consume more thinking the initial dose was ineffective, resulting in eventual overconsumption when absorption finally occurs.
Whilst formal interaction studies are lacking, the pharmacodynamic opposition—particularly regarding appetite—represents a clinically meaningful concern that warrants discussion with healthcare providers. Patients should not assume safety simply because no interaction is listed in standard references.
Several potential risks arise from concurrent cannabis and Wegovy use, though robust clinical trial data specifically examining this combination are currently unavailable:
Reduced treatment efficacy: The most significant concern is that cannabis-induced appetite stimulation may counteract Wegovy's appetite-suppressing effects, potentially compromising weight loss outcomes. This theoretical interaction warrants careful monitoring of weight loss progress and eating behaviours. Patients investing considerable time and expense in Wegovy treatment may inadvertently undermine their progress through cannabis use, particularly if consumption occurs regularly or in higher doses.
Compounded gastrointestinal symptoms: Both substances can cause nausea and vomiting through different mechanisms. Combining them may increase the severity or frequency of these adverse effects, potentially leading to dehydration, electrolyte imbalances, or treatment discontinuation. Patients experiencing severe or persistent vomiting should seek medical attention promptly, as this may indicate cannabinoid hyperemesis syndrome or other serious conditions requiring assessment.
Gallbladder and pancreatic risks: The Wegovy SmPC highlights increased risks of gallbladder disease (cholelithiasis, cholecystitis) and pancreatitis. Patients should be alert to symptoms such as severe upper abdominal pain (potentially radiating to the back), fever, jaundice, or persistent vomiting, which require urgent medical assessment.
Cardiovascular considerations: Wegovy typically increases heart rate by approximately 2-4 beats per minute, and cannabis use—particularly smoking—can also elevate heart rate and blood pressure acutely. Whilst there is no established synergistic cardiovascular risk, patients with pre-existing cardiovascular disease should exercise particular caution and discuss any substance use with their cardiologist or GP.
Impaired judgement and adherence: Cannabis intoxication may affect decision-making regarding diet, exercise, and medication adherence—all crucial components of successful weight management. Patients may be more likely to overeat or make poor nutritional choices whilst under the influence.
Mental health interactions: Both Wegovy and cannabis can affect mood and mental health. The EMA and MHRA have reviewed reports of suicidal thoughts with GLP-1 receptor agonists, though causality remains unconfirmed. Patients should report any new or worsening mood symptoms to their healthcare provider promptly. Those with depression, anxiety, or other psychiatric conditions should be aware that cannabis may exacerbate symptoms or interact with concurrent psychiatric medications.
These risks underscore the importance of individualised medical advice rather than generalised assumptions about safety.
Healthcare professionals emphasise honest, non-judgemental communication about all substance use, including cannabis, when prescribing Wegovy. The General Medical Council (GMC) and NICE guidance support patient-centred care that acknowledges real-world behaviours whilst prioritising safety and treatment efficacy.
Key recommendations include:
Disclosure: Patients should inform their prescriber about any cannabis use—recreational or medicinal—before starting Wegovy. This allows for individualised risk assessment and monitoring plans. Prescribers are bound by confidentiality and focus on patient safety rather than judgement.
Monitoring: Patients using both substances should be monitored more closely for treatment efficacy (weight loss progress), adverse effects (particularly gastrointestinal symptoms), and overall wellbeing. Regular follow-up appointments allow for early identification of problems. People with diabetes should monitor blood glucose levels more frequently.
Dose adjustments: If gastrointestinal side effects are problematic, the Wegovy SmPC advises considering slower dose escalation or temporary dose reduction. This should always be discussed with the prescriber rather than self-managed.
Medical cannabis patients: Those prescribed medical cannabis for conditions such as chronic pain or chemotherapy-induced nausea face a more complex situation. These patients should ensure all prescribers are aware of their complete medication regimen and work collaboratively to balance therapeutic goals.
When to seek urgent medical attention:
Severe, persistent vomiting that prevents fluid intake
Signs of dehydration (dark urine, dizziness, confusion)
Severe abdominal pain, especially in the upper abdomen or right upper quadrant
Chest pain or significant palpitations
Symptoms of pancreatitis (severe upper abdominal pain radiating to the back)
Yellowing of the skin or eyes (jaundice)
For severe symptoms or chest pain, call 999. For urgent but non-emergency concerns, contact NHS 111 or your GP.
The MHRA Yellow Card scheme (yellowcard.mhra.gov.uk) allows reporting of suspected adverse drug reactions, including those potentially related to substance combinations. Healthcare professionals and patients can contribute to pharmacovigilance by reporting unexpected effects.
For patients committed to achieving weight loss goals with Wegovy, discontinuing cannabis use represents the most straightforward approach to avoiding potential interactions and maximising treatment efficacy. However, recognising that some patients may be unwilling or unable to stop completely, harm reduction strategies can minimise risks:
Harm reduction approaches:
Reduce frequency and dose: Limiting cannabis use to occasional rather than daily consumption, and using lower doses, may reduce appetite stimulation and other interfering effects whilst acknowledging that any use carries potential risks.
Avoid smoking: If cannabis use continues, vaporising or using edible preparations avoids the cardiovascular and respiratory risks associated with smoking. However, edibles can be harder to dose accurately and may have significantly delayed, prolonged effects when taken with Wegovy due to delayed gastric emptying. This increases the risk of overconsumption if patients take additional doses thinking the first was ineffective.
Legal considerations: Remember that recreational cannabis remains illegal in the UK as a Class B controlled substance. Drug-driving laws apply, and cannabis can remain detectable in your system for days after use. Never drive or operate machinery while under the influence.
CBD-dominant products: Cannabidiol (CBD) without significant THC content does not produce intoxication or appetite stimulation to the same degree. The Food Standards Agency (FSA) advises healthy adults not to take more than 70mg of CBD per day unless under medical supervision. CBD products in the UK vary widely in quality and regulation, and CBD may interact with other medications.
Address underlying reasons for use: Patients using cannabis for pain, anxiety, insomnia, or other symptoms should discuss evidence-based alternatives with their GP. NICE-recommended treatments for these conditions may be more appropriate and avoid potential interference with weight management.
Alternative approaches to common concerns:
For nausea: First try non-drug measures such as small, frequent meals, avoiding trigger foods, ginger, and staying hydrated. If medication is needed, discuss with your prescriber—options may include antiemetics, but these have their own safety considerations (domperidone has cardiac risks and is only for short-term use; ondansetron can cause constipation)
For pain: Multimodal pain management including physiotherapy, appropriate analgesia, and psychological approaches
For anxiety: Cognitive behavioural therapy (CBT), mindfulness-based interventions, or appropriate pharmacotherapy
For sleep: Sleep hygiene education, cognitive behavioural therapy for insomnia (CBT-I)
Patients should work collaboratively with their healthcare team to develop an individualised plan that supports both their weight management goals and overall health, recognising that successful treatment requires addressing all factors that may influence outcomes.
There is no listed pharmacokinetic interaction between cannabis and Wegovy in the BNF or SmPC. However, cannabis stimulates appetite whilst Wegovy suppresses it, creating a pharmacodynamic opposition that may reduce treatment efficacy and compromise weight loss outcomes.
Cannabis, particularly THC, is known to stimulate appetite, which may counteract Wegovy's appetite-suppressing effects and potentially reduce weight loss progress. Patients should discuss any cannabis use with their prescriber for individualised monitoring.
Yes, patients should inform their prescriber about all cannabis use—recreational or medicinal—to allow for individualised risk assessment, appropriate monitoring, and optimisation of treatment outcomes. Healthcare professionals maintain confidentiality and focus on patient safety.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.