Many patients prescribed Ozempic (semaglutide) for type 2 diabetes experience digestive side effects such as nausea, bloating, and altered bowel habits. These symptoms arise because Ozempic slows gastric emptying as part of its mechanism of action. Some individuals wonder whether taking digestive enzymes whilst on Ozempic might alleviate these uncomfortable gastrointestinal effects. Whilst no direct contraindication exists between semaglutide and over-the-counter digestive enzyme supplements, there is limited evidence supporting their use for GLP-1 receptor agonist-related symptoms. This article examines the relationship between digestive enzymes and Ozempic, explores the evidence for combining them, and provides guidance on managing digestive side effects safely and effectively.
Quick Answer: There is no contraindication to taking digestive enzymes whilst on Ozempic, but no robust evidence supports their effectiveness for GLP-1 receptor agonist-related digestive symptoms.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. It is administered as a once-weekly subcutaneous injection and works by mimicking the action of the naturally occurring hormone GLP-1. The Medicines and Healthcare products Regulatory Agency (MHRA) has approved Ozempic for improving glycaemic control in adults with type 2 diabetes as an adjunct to diet and exercise; as monotherapy only when metformin is inappropriate (due to intolerance or contraindication), or in combination with other glucose-lowering medicines.
The mechanism of action of semaglutide directly impacts the digestive system in several ways. GLP-1 receptor agonists slow gastric emptying, meaning food remains in the stomach for longer periods before moving into the small intestine. This delayed gastric emptying contributes to improved blood glucose control by reducing post-prandial glucose spikes and promoting satiety, which can assist with weight management. However, this same mechanism is responsible for many of the gastrointestinal side effects commonly reported by patients.
Common digestive side effects associated with Ozempic include:
Nausea (very common, affecting ≥1/10 patients)
Vomiting
Diarrhoea
Constipation
Abdominal pain
Dyspepsia (indigestion)
Abdominal distension
Reduced appetite
Eructation (belching)
These gastrointestinal symptoms are typically most pronounced during the initial weeks of treatment or following dose escalation. The NICE guidance (NG28) on type 2 diabetes management acknowledges these side effects and the Summary of Product Characteristics (SmPC) recommends gradual dose titration to improve tolerability. Most patients experience a reduction in symptoms over time as the body adapts to the medication, though some individuals may continue to experience persistent digestive discomfort that affects their quality of life and adherence to treatment.
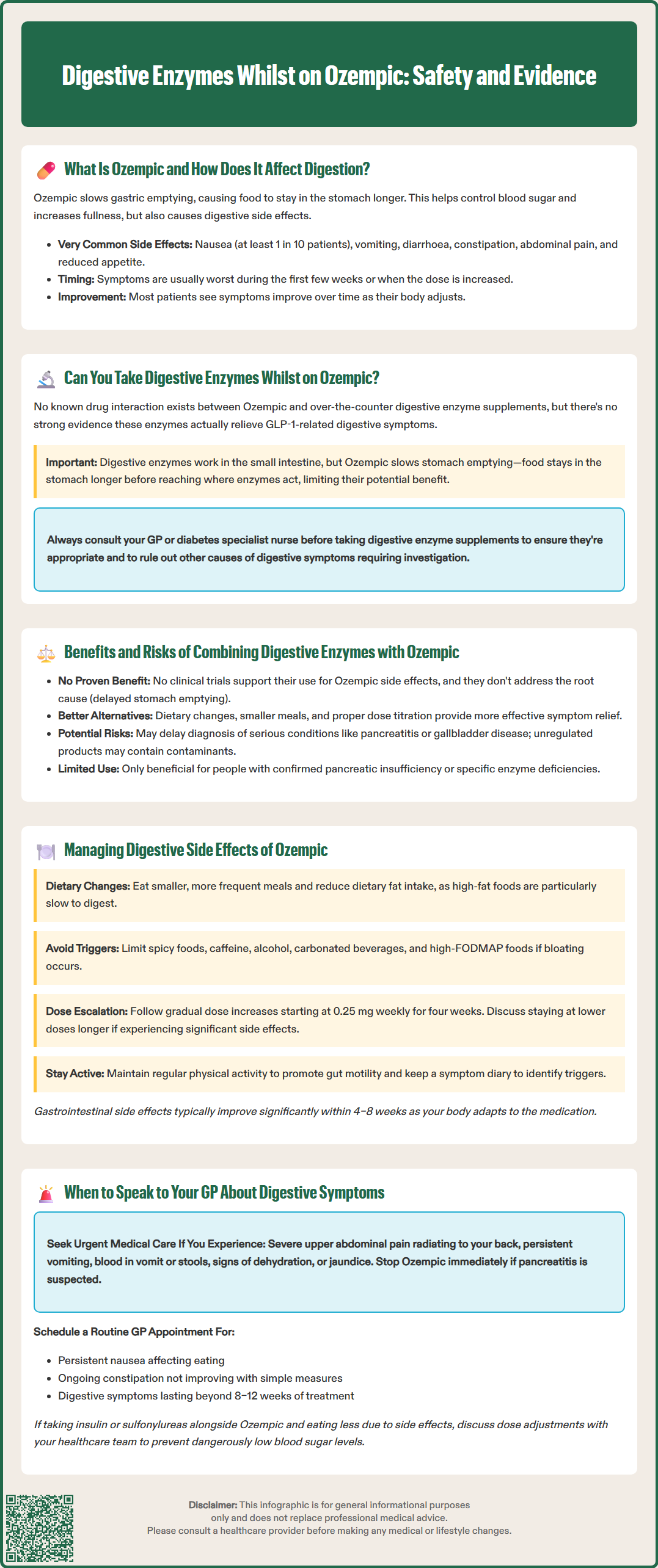
No contraindication or interaction is listed in the Ozempic SmPC regarding the use of digestive enzyme supplements, and no known direct pharmacological interaction exists between semaglutide and over-the-counter digestive enzyme preparations. However, there is no robust evidence that over-the-counter digestive enzymes improve GLP-1 receptor agonist-related gastrointestinal symptoms.
Digestive enzymes—such as those containing amylase, lipase, protease, or lactase—are designed to assist with the breakdown of carbohydrates, fats, proteins, and lactose respectively. These supplements are commonly used by individuals experiencing symptoms of maldigestion or enzyme insufficiency.
It is important to note that prescribed pancreatic enzyme replacement therapy (PERT) such as pancrelipase (Creon) is different from over-the-counter supplements. PERT is a licensed medicine for treating exocrine pancreatic insufficiency and should not be substituted with non-prescription supplements.
Digestive enzymes address different physiological processes than those affected by Ozempic. Whilst Ozempic slows gastric emptying and reduces gut motility, digestive enzymes work within the small intestine to facilitate nutrient breakdown. The delayed gastric emptying caused by semaglutide means food spends more time in the stomach before reaching the small intestine where these enzymes would typically act. Therefore, the theoretical benefit of supplemental digestive enzymes in managing Ozempic-related symptoms may be limited.
Before starting any digestive enzyme supplement, patients should consider several factors:
The specific digestive symptoms being experienced
Whether symptoms are related to delayed gastric emptying or actual enzyme deficiency
The quality and regulatory status of the supplement product
Potential effects on blood glucose monitoring
Patients with type 2 diabetes should be particularly cautious, as some digestive enzyme products may contain added sugars or fillers that could affect glycaemic control. Food supplements are regulated as foods (not medicines) by the Food Standards Agency, so product quality can vary considerably. It is strongly recommended that patients discuss the use of any supplements with their GP or diabetes specialist nurse before commencing, to ensure the approach is appropriate for their individual circumstances and to rule out other underlying causes of digestive symptoms that may require specific investigation or treatment.
Potential benefits of using digestive enzymes alongside Ozempic remain largely theoretical and are not supported by robust clinical evidence. No randomised trials have been identified assessing digestive enzymes for GLP-1 receptor agonist-related gastrointestinal side effects. Some patients report subjective improvement in symptoms such as bloating, gas, or feelings of fullness when using enzyme supplements, though it is difficult to determine whether this represents a genuine pharmacological effect or a placebo response. For individuals with confirmed pancreatic insufficiency or specific enzyme deficiencies (such as lactose intolerance), appropriate enzyme supplementation may provide benefit regardless of Ozempic use.
The pathophysiology of Ozempic-related digestive symptoms—primarily delayed gastric emptying and altered gut motility—suggests that enzyme supplementation would not address the root cause. Patients seeking symptom relief may benefit more from dietary modifications, eating smaller meals, and following the dose titration schedule recommended by their healthcare professional.
Potential risks and considerations include:
Delayed diagnosis: Relying on supplements may mask symptoms of serious underlying conditions such as pancreatitis, gallbladder disease, or gastroparesis that require medical investigation
Product quality concerns: Unregulated supplements may contain contaminants, incorrect doses, or unlisted ingredients
Financial cost: Digestive enzyme supplements can be expensive and are not typically available on NHS prescription for this indication
False reassurance: Patients may delay seeking appropriate medical advice if they believe supplements are addressing their symptoms
Rare but serious gastrointestinal complications associated with Ozempic include acute pancreatitis, cholelithiasis (gallstones) and cholecystitis. If pancreatitis is suspected (severe, persistent upper abdominal pain, particularly if radiating to the back, with or without vomiting), stop semaglutide immediately and seek urgent medical assessment. Gallbladder problems may present with right upper quadrant pain, especially after fatty meals. The Ozempic SmPC includes warnings about these risks, emphasising the importance of proper medical evaluation of significant or persistent digestive symptoms.
Evidence-based strategies for managing Ozempic-related digestive symptoms focus on dietary and lifestyle modifications rather than supplementation. NICE guidance (NG28) and diabetes specialist consensus recommend a stepwise approach to minimising gastrointestinal side effects whilst maintaining the therapeutic benefits of GLP-1 receptor agonist therapy.
Dietary modifications that may help reduce symptoms include:
Eating smaller, more frequent meals rather than large portions, which can overwhelm the already-delayed gastric emptying
Reducing dietary fat intake, as high-fat meals are particularly slow to empty from the stomach
Avoiding foods that commonly trigger symptoms such as spicy foods, caffeine, alcohol, and carbonated beverages
Eating slowly and chewing thoroughly to reduce the amount of air swallowed and ease the digestive process
Staying well hydrated, particularly if experiencing diarrhoea, though avoiding drinking large volumes with meals
Identifying and limiting foods high in fermentable carbohydrates (FODMAPs) if bloating and gas are problematic—this approach should ideally be supervised by a dietitian to avoid nutritional compromise
Medication management strategies are equally important. The standard approach involves gradual dose escalation as specified in the SmPC, typically starting at 0.25 mg weekly for four weeks, then increasing to 0.5 mg weekly. Further increases to 1 mg or 2 mg weekly should only occur if tolerated and if additional glycaemic control is needed. Patients experiencing significant side effects may benefit from remaining at a lower dose for a longer period before escalating, or temporarily stepping back to a previously tolerated dose—this should be discussed with their diabetes team or GP.
According to the SmPC, Ozempic should be administered on the same day each week, at any time of day, independent of meals. Due to the long half-life and steady-state pharmacokinetics of semaglutide, changing the time of administration is unlikely to significantly affect gastrointestinal side effects.
Additional supportive measures include maintaining regular physical activity, which can help promote gut motility, and keeping a symptom diary to identify specific triggers or patterns. Patients should be reassured that gastrointestinal side effects typically improve significantly after the first 4–8 weeks of treatment as the body adapts to the medication.
Patients should contact their GP or diabetes care team if digestive symptoms are severe, persistent, or significantly affecting their quality of life and ability to maintain adequate nutrition. Whilst mild nausea and occasional digestive discomfort are common and expected side effects of Ozempic, certain symptoms warrant prompt medical evaluation to rule out serious complications or alternative diagnoses.
Red flag symptoms requiring urgent medical attention include:
Severe, persistent abdominal pain, particularly if located in the upper abdomen and radiating to the back (potential pancreatitis)—if pancreatitis is suspected, stop semaglutide immediately and seek urgent medical assessment
Persistent vomiting that prevents adequate fluid or medication intake
Signs of dehydration such as dizziness, reduced urine output, or dark urine
Severe diarrhoea lasting more than 48 hours
Blood in vomit or stools
Unexplained weight loss beyond what is expected from the medication's therapeutic effect
Jaundice (yellowing of skin or eyes), which may indicate gallbladder or liver problems
Patients should contact NHS 111 for urgent advice when GP access is not immediately available. Patients taking insulin or sulfonylureas alongside Ozempic should discuss dose adjustments with their healthcare team if food intake is reduced, to avoid hypoglycaemia.
Non-urgent symptoms that should be discussed at a routine appointment include persistent nausea affecting food intake, ongoing constipation not responding to simple measures, or any digestive symptoms that have not improved after 8–12 weeks of treatment. The GP may consider adjusting the Ozempic dose, switching to an alternative GLP-1 receptor agonist with potentially better tolerability, or investigating for other causes of symptoms.
Before considering digestive enzyme supplementation, patients should undergo appropriate clinical assessment. This may include:
Review of medication history and dose escalation schedule
Dietary assessment and advice from a dietitian
Blood tests including amylase, lipase, liver function, and coeliac serology if indicated
Consideration of imaging or endoscopy if symptoms suggest structural pathology
Patients should never discontinue Ozempic without medical advice (except if pancreatitis is suspected), as abrupt cessation can lead to deterioration in glycaemic control. If side effects are intolerable, the healthcare team can develop an appropriate management plan, which may include temporary dose reduction, additional symptomatic treatment, or transition to alternative diabetes medications. Patients should report suspected side effects via the MHRA Yellow Card scheme. Maintaining open communication with healthcare professionals ensures that digestive symptoms are managed safely and effectively whilst preserving the important metabolic benefits of GLP-1 receptor agonist therapy.
There is no robust clinical evidence that over-the-counter digestive enzymes improve Ozempic-related gastrointestinal symptoms such as nausea or bloating. Dietary modifications and gradual dose escalation are more evidence-based approaches to managing these side effects.
Whilst no direct contraindication exists, relying on supplements may delay diagnosis of serious conditions such as pancreatitis or gallbladder disease. Patients should discuss any supplement use with their GP or diabetes team before starting.
Seek urgent medical attention for severe abdominal pain (especially if radiating to the back), persistent vomiting, signs of dehydration, blood in vomit or stools, or jaundice. Contact your GP for persistent symptoms not improving after 8–12 weeks or significantly affecting nutrition.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.