Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes management. Whilst effective for glycaemic control, constipation is a commonly reported side effect due to delayed gastric emptying and reduced gut motility. Choosing the best laxative to use with Ozempic requires understanding both the underlying mechanism and safe, evidence-based options. This article explores why constipation occurs, which laxatives are recommended by NICE and the BNF, and how lifestyle modifications can support bowel health during semaglutide therapy. Always consult your GP or pharmacist before starting any laxative treatment.
Quick Answer: Macrogol (polyethylene glycol) and bulk-forming laxatives such as ispaghula husk are generally considered the safest and most effective first-line options for managing Ozempic-related constipation.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. A higher dose formulation of semaglutide (Wegovy) is licensed for weight management, but Ozempic itself is not approved for this purpose. Whilst the medication offers significant benefits in glycaemic control, gastrointestinal side effects are amongst the most commonly reported adverse reactions.
Constipation occurs because semaglutide slows gastric emptying and reduces gut motility as part of its mechanism of action. By mimicking the naturally occurring GLP-1 hormone, Ozempic delays the passage of food through the digestive tract, which helps regulate blood glucose levels and promotes satiety. However, this delayed transit time can result in harder, less frequent stools. Clinical trials have shown that gastrointestinal disturbances, including constipation, affect a notable proportion of patients, particularly during dose escalation phases. This gastric emptying delay is often most pronounced early in treatment and may attenuate somewhat with continued use.
Additionally, dietary changes often accompany Ozempic therapy. Patients may reduce their overall food and fluid intake due to decreased appetite, inadvertently lowering their fibre and water consumption—both essential for regular bowel movements. Dehydration can compound the problem, as adequate hydration is crucial for maintaining soft, easily passed stools.
It is important to recognise that whilst constipation is an expected side effect for some individuals, it should not be dismissed. Persistent or severe constipation warrants medical review, as it may indicate the need for dose adjustment or additional management strategies. Severe, persistent abdominal pain (especially if accompanied by vomiting) or symptoms suggesting bowel obstruction require urgent medical assessment, as these could indicate serious complications such as pancreatitis or intestinal obstruction. Understanding the underlying pharmacological cause empowers patients to take proactive steps in managing this common adverse effect.
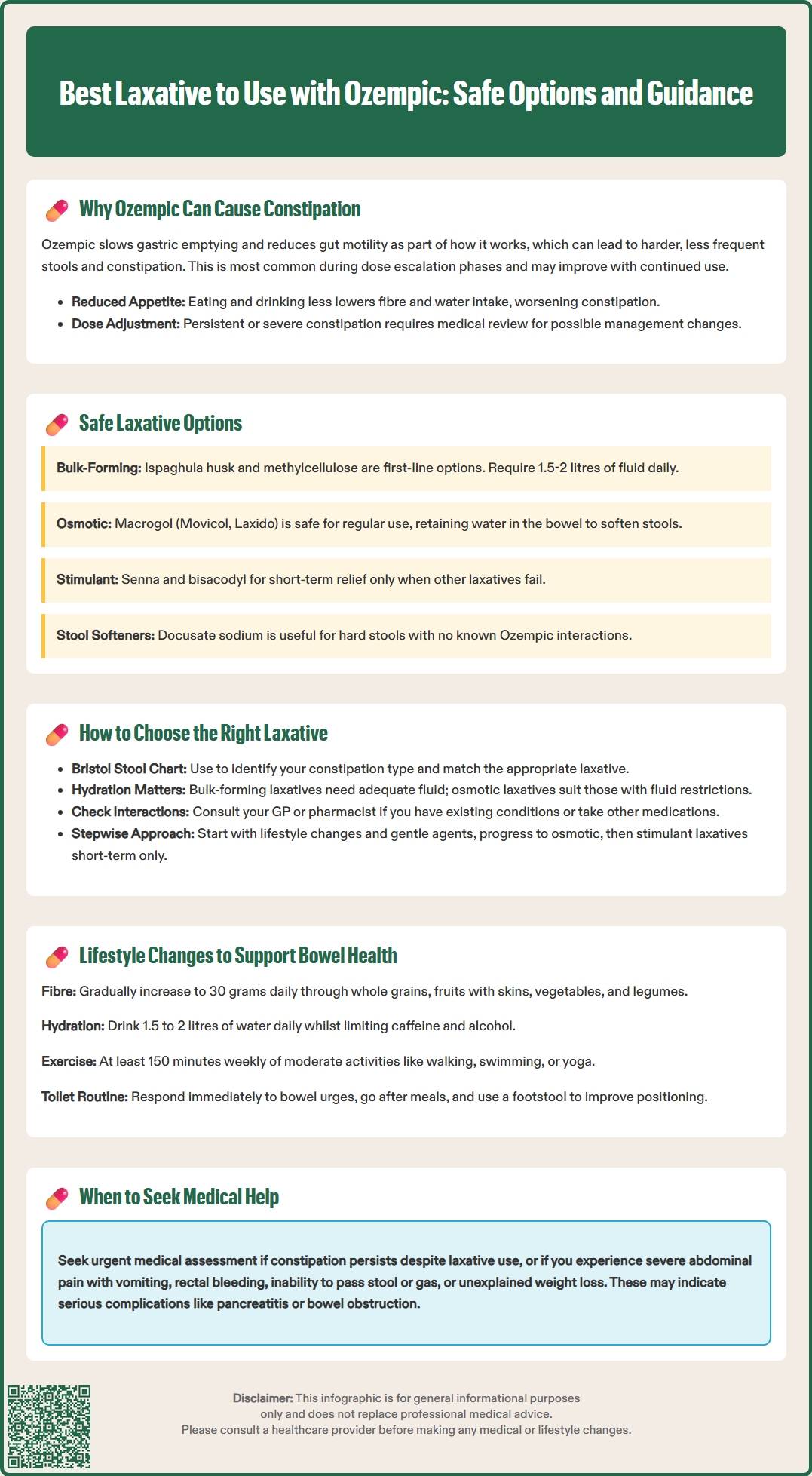
When lifestyle measures alone prove insufficient, laxatives can provide effective symptomatic relief for constipation associated with Ozempic therapy. The National Institute for Health and Care Excellence (NICE) and British National Formulary (BNF) guidance support a stepwise approach to laxative selection, prioritising agents with favourable safety profiles.
Bulk-forming laxatives, such as ispaghula husk (Fybogel) or methylcellulose, are often considered first-line options. These agents increase stool mass by absorbing water, thereby stimulating peristalsis naturally. They are generally well tolerated and suitable for long-term use. However, adequate fluid intake is essential to prevent paradoxical worsening of constipation or intestinal obstruction. Aim for at least 1.5-2 litres daily unless you have been advised to restrict fluids due to a medical condition such as heart failure or kidney disease. Bulk-forming laxatives should be avoided if faecal impaction is suspected or in cases of severe immobility.
Osmotic laxatives represent another safe choice. Macrogol (polyethylene glycol, such as Movicol or Laxido) is widely recommended and works by retaining water within the bowel lumen, softening stools and increasing their volume. Macrogol preparations containing electrolytes have an excellent safety profile and are designed to minimise electrolyte disturbances when used as directed. Lactulose, another osmotic agent, is also effective, though it may cause bloating or flatulence in some individuals.
Stimulant laxatives, including senna or bisacodyl, may be used for short-term or intermittent relief when other measures fail. These agents stimulate colonic contractions and should generally be reserved for short-term use. Long-term use may be appropriate in some cases but should be under medical supervision with monitoring.
Stool softeners such as docusate sodium can be helpful, particularly when stools are hard and difficult to pass. There is no evidence of significant drug interactions between these laxative classes and semaglutide, but patients should always inform their GP or pharmacist of all medications they are taking. If constipation persists despite laxative use, or if warning symptoms such as severe abdominal pain, rectal bleeding, or unexplained weight loss occur, urgent medical assessment is required.
Suspected adverse effects related to Ozempic or laxatives should be reported through the MHRA Yellow Card Scheme.
Selecting an appropriate laxative requires consideration of individual symptoms, medical history, and treatment goals. A personalised approach ensures both efficacy and safety whilst minimising potential adverse effects.
Assess the nature of your constipation. The Bristol Stool Chart can help characterise your symptoms. If stools are infrequent but soft, a bulk-forming laxative may suffice to increase stool volume and stimulate regular bowel movements. Conversely, if stools are hard and difficult to pass (Types 1-2 on the Bristol Stool Chart), an osmotic laxative such as macrogol is often more effective, as it directly addresses stool consistency by increasing water content.
Consider your fluid intake and mobility. Bulk-forming agents require adequate hydration to work effectively and may not be suitable for individuals with restricted fluid intake or swallowing difficulties. Osmotic laxatives are generally better tolerated in these circumstances. Patients with reduced mobility may benefit from a combination approach, as physical activity plays a significant role in promoting gut motility.
Review your medication list and comorbidities. Certain laxatives may be contraindicated in specific conditions. For example, lactulose contains galactose and lactose, though it is usually safe for people with diabetes as systemic absorption is minimal. Patients should seek individual advice from their healthcare provider. Stimulant laxatives are best avoided in individuals with inflammatory bowel disease or intestinal obstruction. Always consult your GP or pharmacist before starting a new laxative, particularly if you have pre-existing gastrointestinal conditions or take multiple medications.
Start with the gentlest option and escalate as needed. NICE guidance advocates a stepwise approach: begin with lifestyle modifications and bulk-forming agents, progressing to osmotic laxatives if necessary, and reserving stimulant laxatives for short-term or intermittent use. This strategy minimises the risk of adverse effects.
Monitor your response and adjust accordingly. Keep a symptom diary noting bowel frequency, stool consistency (using the Bristol Stool Chart), and any side effects. If a particular laxative proves ineffective after one to two weeks of regular use, discuss alternative options with your healthcare provider. Persistent constipation may require investigation to exclude other underlying causes.
Whilst laxatives provide symptomatic relief, addressing lifestyle factors is fundamental to achieving sustainable bowel regularity during Ozempic therapy. Evidence-based modifications can significantly reduce the frequency and severity of constipation.
Increase dietary fibre intake gradually. The NHS recommends a daily fibre intake of approximately 30 grams for adults. Incorporate a variety of fibre sources, including:
Whole grains (oats, brown rice, wholemeal bread)
Fruits (apples, pears, berries—preferably with skins)
Vegetables (broccoli, carrots, leafy greens)
Legumes (lentils, chickpeas, beans)
Introduce fibre gradually to avoid bloating and gas, and always pair increased fibre with adequate fluid intake.
Maintain optimal hydration. Aim for at least 1.5 to 2 litres of water daily, adjusting for activity level and climate, unless you have been advised to restrict fluids due to a medical condition. Adequate hydration softens stools and facilitates their passage through the colon. Limit caffeinated and alcoholic beverages, as these can contribute to dehydration.
Engage in regular physical activity. Exercise stimulates intestinal motility and promotes regular bowel movements. The UK Chief Medical Officers' guidelines recommend at least 150 minutes of moderate-intensity aerobic activity weekly. Even gentle activities such as walking, swimming, or yoga can be beneficial.
Establish a consistent bowel routine. Respond promptly to the urge to defecate, as delaying can worsen constipation. Allow adequate time for bowel movements, ideally after meals when the gastrocolic reflex is most active. Adopting a squatting position (using a footstool to elevate the feet whilst seated on the toilet) can facilitate easier evacuation.
Review your Ozempic dosing schedule with your GP. If constipation is severe or persistent, your healthcare provider may consider adjusting the dose escalation schedule or exploring alternative GLP-1 receptor agonists with different gastrointestinal side effect profiles. Any changes to your semaglutide dosage must be made by your prescriber in accordance with the product licence.
When to seek medical advice: Contact your GP if you experience severe abdominal pain (especially if accompanied by vomiting), rectal bleeding, unexplained weight loss, abdominal distension, or absolute constipation (complete inability to pass stool or gas). These symptoms may warrant urgent investigation to exclude serious complications such as pancreatitis, bowel obstruction, or other underlying pathology.
Yes, laxatives can be safely used with Ozempic. Bulk-forming laxatives (such as ispaghula husk) and osmotic laxatives (such as macrogol) are generally recommended first-line options, with no known significant drug interactions with semaglutide.
Constipation is often most pronounced during the initial weeks of Ozempic therapy and dose escalation phases. Symptoms may improve with continued use as the body adjusts, though some individuals may require ongoing management strategies.
Seek urgent medical advice if you experience severe abdominal pain (especially with vomiting), rectal bleeding, unexplained weight loss, abdominal distension, or complete inability to pass stool or gas, as these may indicate serious complications requiring investigation.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.