
Many people prescribed GLP-1 receptor agonists for type 2 diabetes or weight management wonder whether they'll need to take these medications indefinitely. The answer isn't straightforward—treatment duration depends on your underlying condition, treatment goals, response to therapy, and ability to maintain improvements through lifestyle changes. Whilst GLP-1 medications are often used long-term, particularly for diabetes management, they're not necessarily lifelong for everyone. Understanding the factors that influence treatment duration, what happens when you stop, and the alternatives available can help you make informed decisions with your healthcare team about the most appropriate approach for your individual circumstances.
Quick Answer: GLP-1 medications are not necessarily lifelong treatments, but duration depends on your condition, treatment response, and ability to maintain improvements through lifestyle changes.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
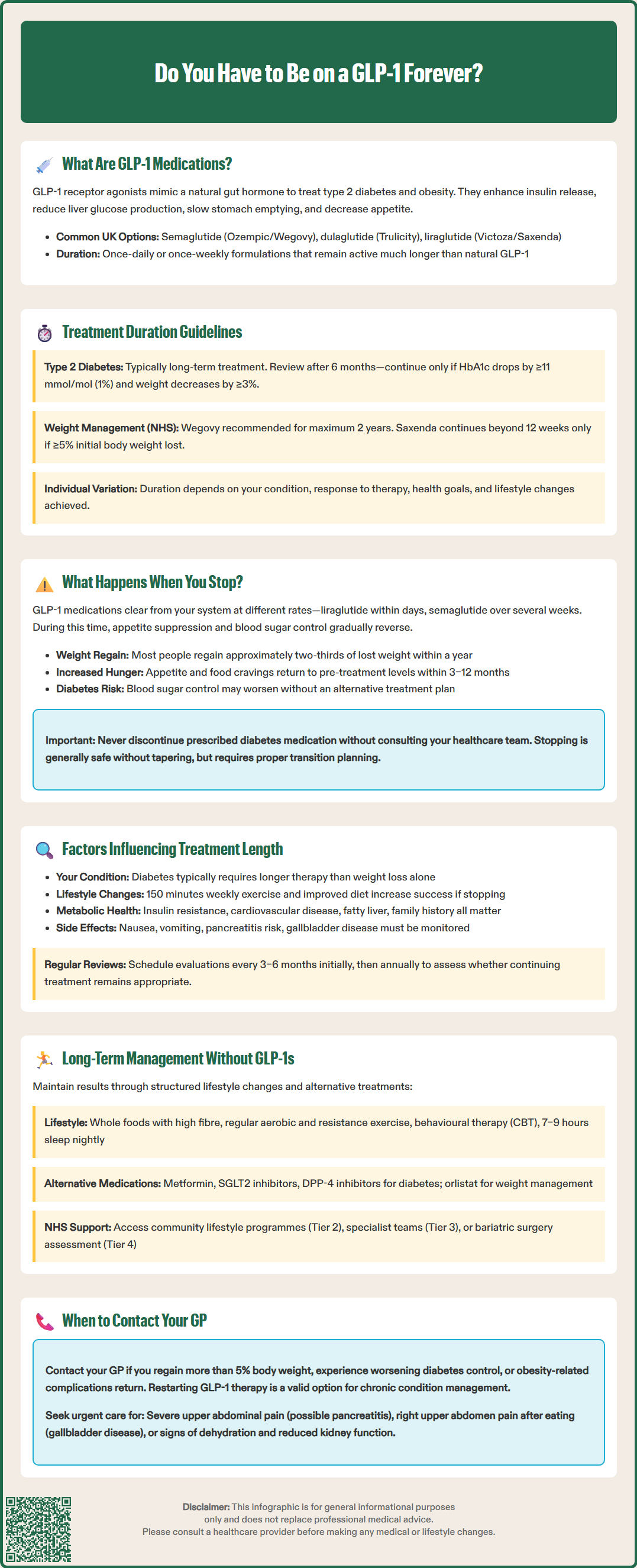
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily used to manage type 2 diabetes and, more recently, obesity. These medicines mimic the action of a naturally occurring hormone called GLP-1, which is produced in the intestines in response to food intake. The body's own GLP-1 plays several important roles in regulating blood glucose and appetite.
When you take a GLP-1 medication, the drug binds to GLP-1 receptors throughout the body. This triggers several beneficial effects:
Enhanced insulin secretion from the pancreas when blood glucose levels are elevated
Reduced glucagon release, which prevents the liver from producing excess glucose
Slowed gastric emptying, meaning food moves more slowly from the stomach into the intestines
Increased satiety signals to the brain, reducing appetite and food intake
These combined mechanisms help lower blood glucose levels in people with type 2 diabetes and promote weight loss in those with obesity. In the UK, different GLP-1 receptor agonists have specific licensed indications:
For type 2 diabetes: semaglutide (Ozempic), dulaglutide (Trulicity), and liraglutide (Victoza)
For weight management: semaglutide 2.4mg (Wegovy) and liraglutide 3.0mg (Saxenda)
NICE guideline NG28 recommends GLP-1 receptor agonists as treatment options for type 2 diabetes when first-line therapies have not achieved adequate glycaemic control. For weight management, NICE technology appraisals TA875 and TA664 provide specific criteria for NHS use.
Unlike the body's natural GLP-1, which breaks down within minutes, these medications are designed to remain active for much longer—ranging from once-daily to once-weekly formulations. This extended duration of action makes them practical for long-term use, but it also raises important questions about treatment duration and whether lifelong therapy is necessary.
It's worth noting that GLP-1 receptor agonists should not be used in combination with DPP-4 inhibitors, as both work on the same pathway and NICE does not recommend this combination.
The short answer is: not necessarily, but it depends on your individual circumstances. GLP-1 medications are not inherently lifelong treatments, but the duration of therapy varies considerably based on why you're taking them, your response to treatment, and your overall health goals.
For type 2 diabetes management, GLP-1 receptor agonists are typically considered long-term treatments. Type 2 diabetes is a chronic, progressive condition, and most people require ongoing medication to maintain glycaemic control. However, NICE guideline NG28 specifies continuation criteria: treatment should be reviewed after approximately 6 months and only continued if you've achieved both a reduction in HbA1c of at least 11 mmol/mol (1%) and weight loss of at least 3%. Some individuals may be able to reduce or discontinue GLP-1 therapy if they achieve substantial lifestyle changes that improve their insulin sensitivity and glucose metabolism.
For weight management, the picture is somewhat different but still complex. In the UK, there are specific NHS criteria:
Semaglutide 2.4mg (Wegovy): NICE technology appraisal TA875 recommends this only within specialist weight management services and for a maximum of 2 years on the NHS
Liraglutide 3.0mg (Saxenda): NICE technology appraisal TA664 specifies that treatment should only continue beyond 12 weeks if you've lost at least 5% of your initial body weight
Clinical trials have demonstrated that most people regain weight after stopping GLP-1 medications. The STEP trials with semaglutide showed that participants regained approximately two-thirds of their lost weight within a year of discontinuation. This suggests that for many people with obesity, ongoing treatment may be necessary to maintain weight loss.
Your GP or specialist will work with you to determine the most appropriate duration based on your treatment goals, response to therapy, and ability to maintain improvements through lifestyle measures alone.
When you discontinue GLP-1 therapy, the medication's effects gradually wear off as the drug is eliminated from your system. The timeline varies depending on the specific medication—shorter-acting formulations like liraglutide clear within days, whilst longer-acting options like semaglutide may take several weeks to fully leave your body.
The most commonly reported changes after stopping GLP-1 medications include:
Return of appetite: The appetite-suppressing effects diminish, and many people notice increased hunger and food cravings returning to pre-treatment levels
Weight regain: Clinical evidence consistently shows that most individuals regain weight after discontinuation, often within 3–12 months
Rising blood glucose levels: For those with type 2 diabetes, HbA1c levels typically increase, sometimes returning to pre-treatment values
Changes in eating patterns: Gastric emptying returns to normal speed, which may affect feelings of fullness after meals
It's important to note that stopping GLP-1 medications is generally safe from a withdrawal perspective—these drugs do not cause physical dependence or withdrawal symptoms in the way some medications do, and tapering is not typically required. However, the metabolic changes that occur can feel significant, particularly the return of appetite and potential weight regain.
For people with type 2 diabetes, stopping GLP-1 therapy without an alternative treatment plan can lead to deteriorating glycaemic control, which increases the risk of diabetes-related complications over time. You should never stop taking prescribed diabetes medication without consulting your healthcare team first. Your GP or diabetes specialist can help you develop a safe discontinuation plan if appropriate, which may include transitioning to alternative medications, intensifying lifestyle interventions, or implementing more frequent monitoring of blood glucose levels (typically HbA1c at around 3 months post-cessation, or earlier if symptoms develop).
Seek urgent medical advice if you experience:
Severe, persistent upper abdominal pain (with or without vomiting), which could indicate pancreatitis
Symptoms of gallbladder disease (pain in the right upper abdomen, especially after eating)
Signs of dehydration or reduced kidney function if you've had vomiting or diarrhoea
If you suspect any adverse effects from your medication, you can report them through the MHRA Yellow Card scheme.
Several interconnected factors determine the optimal duration of GLP-1 therapy, and these should be regularly reviewed with your healthcare team. Understanding these variables can help you and your clinician make informed decisions about continuing, adjusting, or potentially stopping treatment.
Your underlying condition and treatment goals are paramount. People using GLP-1 medications for type 2 diabetes management often require longer treatment durations than those using them solely for weight loss. As per NICE guideline NG28, if you've achieved your target HbA1c and maintained it for an extended period alongside substantial lifestyle changes, your doctor may consider whether dose reduction or medication adjustment is appropriate.
The degree of lifestyle modification you've achieved during treatment significantly influences long-term medication needs. Those who have successfully implemented sustainable changes—including regular physical activity (UK Chief Medical Officers recommend at least 150 minutes of moderate-intensity activity weekly), improved dietary patterns, and behavioural strategies for weight management—may have better outcomes if discontinuing GLP-1 therapy. Conversely, if medication has been the primary driver of improvement without accompanying lifestyle changes, stopping treatment is more likely to result in relapse.
Your metabolic health and comorbidities also matter. Factors such as:
Degree of insulin resistance
Presence of other conditions (cardiovascular disease, fatty liver disease, sleep apnoea)
Family history of diabetes or obesity
Age and menopausal status
Previous weight loss attempts and patterns of weight regain
Safety considerations and tolerability play an important role. While many people tolerate GLP-1 medications well, some experience ongoing side effects such as nausea, vomiting, or diarrhoea. More serious concerns include the risk of pancreatitis, gallbladder disease, and—for semaglutide—potential worsening of diabetic retinopathy in some patients. People taking GLP-1 medications with insulin or sulfonylureas have an increased risk of hypoglycaemia. Additionally, these medications are not recommended during pregnancy or breastfeeding, and women of childbearing age should use effective contraception during treatment.
Regular medication reviews—typically every 3–6 months initially, then annually—allow you and your healthcare team to reassess whether continuing GLP-1 therapy remains the best approach for your individual circumstances, based on both benefits and risks.
If you're considering stopping GLP-1 therapy or exploring alternatives, several evidence-based approaches can help maintain metabolic improvements and manage weight or blood glucose levels effectively.
Lifestyle interventions remain the cornerstone of long-term management for both type 2 diabetes and obesity. NICE guidance emphasises structured lifestyle programmes that include:
Dietary modifications: Focus on whole foods, increased fibre intake, reduced processed foods, and appropriate portion control. Mediterranean-style and low-carbohydrate diets have good evidence for diabetes management according to NICE guideline NG28
Regular physical activity: Combining aerobic exercise with resistance training improves insulin sensitivity and helps maintain weight loss
Behavioural support: Psychological interventions, such as cognitive behavioural therapy (CBT), can address emotional eating and help establish sustainable habits
Sleep optimisation: Adequate sleep (7–9 hours) supports metabolic health and appetite regulation
Alternative medications may be appropriate depending on your condition. For type 2 diabetes, options include metformin (typically first-line), SGLT2 inhibitors, DPP-4 inhibitors, or insulin therapy. For weight management in the UK, NICE-approved options are limited to orlistat (available over-the-counter or on prescription) and, within specialist weight management services, liraglutide 3.0mg (Saxenda) or semaglutide 2.4mg (Wegovy) with their specific continuation criteria.
NHS weight management pathways offer structured support. These include:
Tier 2 services: Community-based lifestyle interventions
Tier 3 services: Specialist multidisciplinary teams for complex obesity
Tier 4 services: Bariatric surgery assessment and procedures
Referral criteria for these services are outlined in NICE guideline CG189 for obesity management.
Ongoing monitoring and support are crucial after discontinuing GLP-1 therapy. This should include:
Regular weight and HbA1c monitoring (for those with diabetes)
Periodic review appointments with your GP or practice nurse
Access to dietetic support or weight management services
Clear action plans for what to do if weight regain or glucose levels become concerning
When to seek medical advice: Contact your GP if you experience significant weight regain (typically >5% of body weight), worsening diabetes control (if applicable), or return of obesity-related complications. Early intervention can prevent further deterioration and allow timely adjustment of your management plan. Remember that needing to restart or continue GLP-1 therapy is not a failure—obesity and type 2 diabetes are chronic conditions that often require long-term medical management alongside lifestyle measures.
Yes, stopping GLP-1 medications is generally safe and does not cause physical withdrawal symptoms. However, you should never discontinue prescribed diabetes medication without consulting your healthcare team first, as blood glucose levels may rise and weight regain is common.
NICE recommends semaglutide 2.4mg (Wegovy) for a maximum of 2 years on the NHS within specialist weight management services. Liraglutide 3.0mg (Saxenda) should only continue beyond 12 weeks if you've lost at least 5% of your initial body weight.
Clinical trials show that most people regain weight after stopping GLP-1 medications, with approximately two-thirds of lost weight returning within a year. Appetite typically increases back to pre-treatment levels as the medication's effects wear off.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.